- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Frontline Daratumumab Plus VRd Outperforms Standard VRd Alone in Multiple Myeloma
A late-breaking abstract presented at the American Society of Hematology Annual Meeting and Exposition supports the addition of subcutaneous daratumumab to standard-of-care bortezomib, lenalidomide, and dexamethasone (VRd) in patients with newly diagnosed multiple myeloma who are eligible for autologous stem cell transplantation.
Primary results from the phase 3 PERSEUS trial (NCT03710603) found that adding subcutaneously administered daratumumab to the standard-of-care triplet regimen of bortezomib, lenalidomide, and dexamethasone (VRd) was associated with significantly higher rates of progression-free survival (PFS) in patients with newly diagnosed multiple myeloma. The findings, presented in a late-breaking abstract session at the 2023 American Society of Hematology Annual Meeting and Exposition, support the use of quadruplet therapy with daratumumab plus VRd (D-VRd) as first-line therapy for multiple myeloma.1
Patients with newly diagnosed multiple myeloma treated with intravenous D-VRd induction or consolidation, autologous stem cell transplantation (ASCT), and D-VRd consolidation showed deep, durable responses in the phase 2 GRIFFIN trial,2 but the randomized, phase 3 PERSEUS trial is the first to assess the quadruplet therapy in a head-to-head comparison with standard-of-care triplet therapy.3
The primary end point of the trial is PFS, with secondary end points of overall CR or better rate and the overall minimal residual disease (MRD) negativity rate. A total of 709 patients aged 18-70 years were randomized 1:1 to receive either D-VRd (n = 355) or standard-of-care VRd (n = 354). Other inclusion criteria were transplant eligibility and ECOG performance status of 2 or lower.
At a median follow-up of 47.5 months, patients in the quadruplet therapy cohort experienced a 58% reduction in the risk of disease progression or death compared with the standard-of-care therapy cohort (HR, 0.42; 95% CI, 0.30-0.59; P < .0001). While median PFS was not yet reached in either the D-VRd or VRd arms, estimated 48-month PFS rates in the D-VRd group and the VRd alone group were 84.3% and 67.7%, respectively. PFS benefits were seen across subgroups, including patients with high cytogenetic risk factors and those with International Staging System stage III disease.1
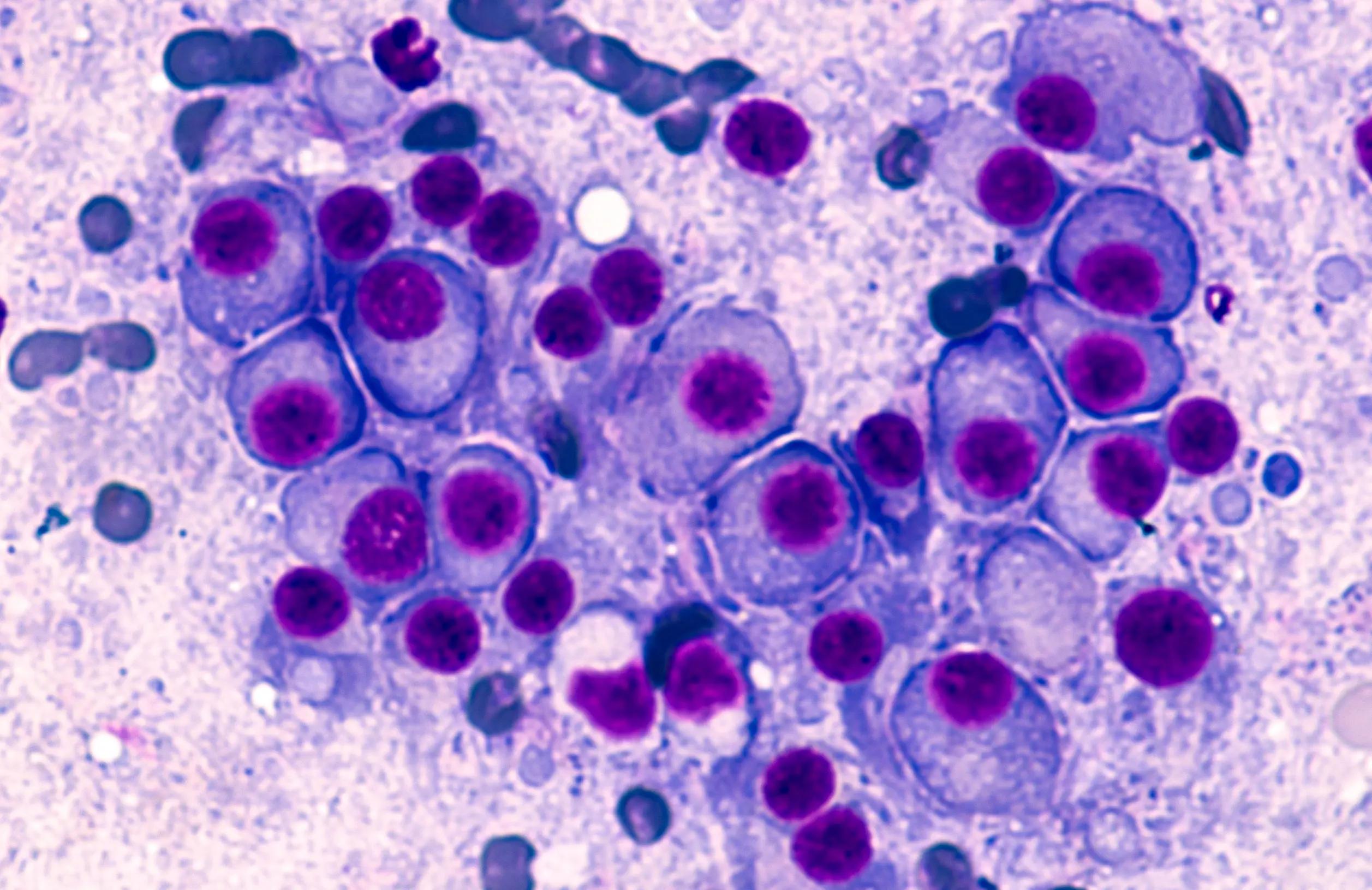
Multiple myeloma | Image credit: David Litman - stock.adobe.com
"One thing I would like to emphasize is that daratumumab was given as a subcutaneous infusion during induction and throughout the maintenance," lead author Pieter Sonneveld, MD, of the Erasmus MC Cancer Institute in Rotterdam, Netherlands, said in a presentation of the data on the final day of the meeting. "The second thing I would like to point out is we administered cycles of 28 days, making it a little bit easier for patients to tolerate this treatment."
The use of subcutaneous daratumumab vs intravenous (IV) administration is a distinguishing factor in the PERSEUS trial regimen, as are the 28-day cycles vs 21-day cycles in typical VRd.
Patients in the quadruplet therapy cohort received 4-6 cycles of 28 days of induction therapy, ASCT if possible, 2 cycles of 28 days of consolidation therapy, then maintenance therapy with daratumumab and lenalidomide (D-R) in 28-day cycles. Those showing MRD positivity continued D-R until progressive disease, while patients showing MRD negativity discontinued daratumumab only after at least 24 months of CR or better and 12 months of sustained MRD negativity. Patients in the latter group restarted daratumumab at CR loss or MRD recurrence.
At the time of the data cutoff, 314 patients in the quadruplet arm and 299 patients in the VRd alone arm had completed all 4 induction and 2 consolidation cycles, 309 and 294 patients in the D-VRd and VRd groups had undergone ASCT, and 322 and 300 patients entered maintenance, respectively.
Patients in the D-VRd cohort also experienced higher rates of complete response (CR) or better (87.9% vs 70.1%; P < .0001) as well as MRD negativity (75.2% vs 47.5%; P < .0001) compared with those receiving the standard of care.
“These randomized, phase 3 results support D-VRd followed by DR maintenance as a new standard of care for transplant-eligible patients with newly diagnosed multiple myeloma,” Sonneveld concluded.
The D-VRd arm experienced higher rates of serious treatment-related adverse events (TRAEs) compared with the VRd arm (57.0% vs 49.3%), although TRAEs led to treatment discontinuation less frequently in the D-VRd cohort vs the VRd cohort (8.8% vs 21.3%). The most common grade 3 or higher TRAEs occurring in at least 10% of patients in the D-VRd and VRd arms were neutropenia (62.1% and 51.0%, respectively), thrombocytopenia (29.1% and 17.3%), diarrhea (10.5% and 7.8%), pneumonia (10.5% and 6.1%), and febrile neutropenia (9.4% and 10.1%). Overall survival (OS) data were not mature at the time of the analysis.
References
1. Sonneveld P, Dimopoulos M, Boccadoro M, et al. Phase 3 randomized study of daratumumab (DARA) + bortezomib, lenalidomide, and dexamethasone (VRd) versus VRd alone in patients (pts) with newly diagnosed multiple myeloma (NDMM) who are eligible for autologous stem cell transplantation (ASCT): primary results of the Perseus trial. Presented at: 65th American Society of Hematology Annual Meeting & Exposition; San Diego, CA: December 9-12, 2023. Abstract LBA-1. https://ash.confex.com/ash/2023/webprogram/Paper191911.html
2. Voorhees PM, Rodriguez C, Reeves B, et al. Daratumumab plus RVd for newly diagnosed multiple myeloma: final analysis of the safety run-in cohort of GRIFFIN. Blood Adv. 2021;5(4):1092-1096. doi:10.1182/bloodadvances.2020003642
3. Daratumumab plus bortezomib, lenalidomide, and dexamethasone (VRd) outperforms VRd alone for multiple myeloma. News release. American Society of Hematology. December 12, 2023. Accessed December 12, 2023.
