- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Elinzanetant Shows Promise for Menopausal Symptom Relief
Study participants treated with elinzanetant experienced significantly reduced hot flash frequency vs paroxetine, desvenlafaxine, and gabapentin in a new meta-analysis.
Elinzanetant, a novel, nonhormonal, selective dual neurokinin-1 (NK-1) and NK-3 receptor antagonist, may more effectively relieve vasomotor symptoms (VMS), also known as hot flashes, and sleep disturbances associated with menopause compared with other nonhormonal therapies, according to research presented at the Academy of Managed Care Pharmacy 2025 annual meeting.1
In a systematic literature review, researchers found that elinzanetant had the highest probability of being the most effective treatment for VMS and that it improved sleep disturbance vs other nonhormonal therapies. While the findings are based on estimates derived from indirect comparison, they suggest that elinzanetant is a potentially effective option for menopausal symptom relief.
VMS impacts up to 80% of women in the menopausal transition, the authors noted, adding that nonhormonal pharmaceutical therapies such as elinzanetant offer alternatives to standard hormone therapies that may be associated with elevated endometrial cancer, breast cancer, and thrombosis risks.
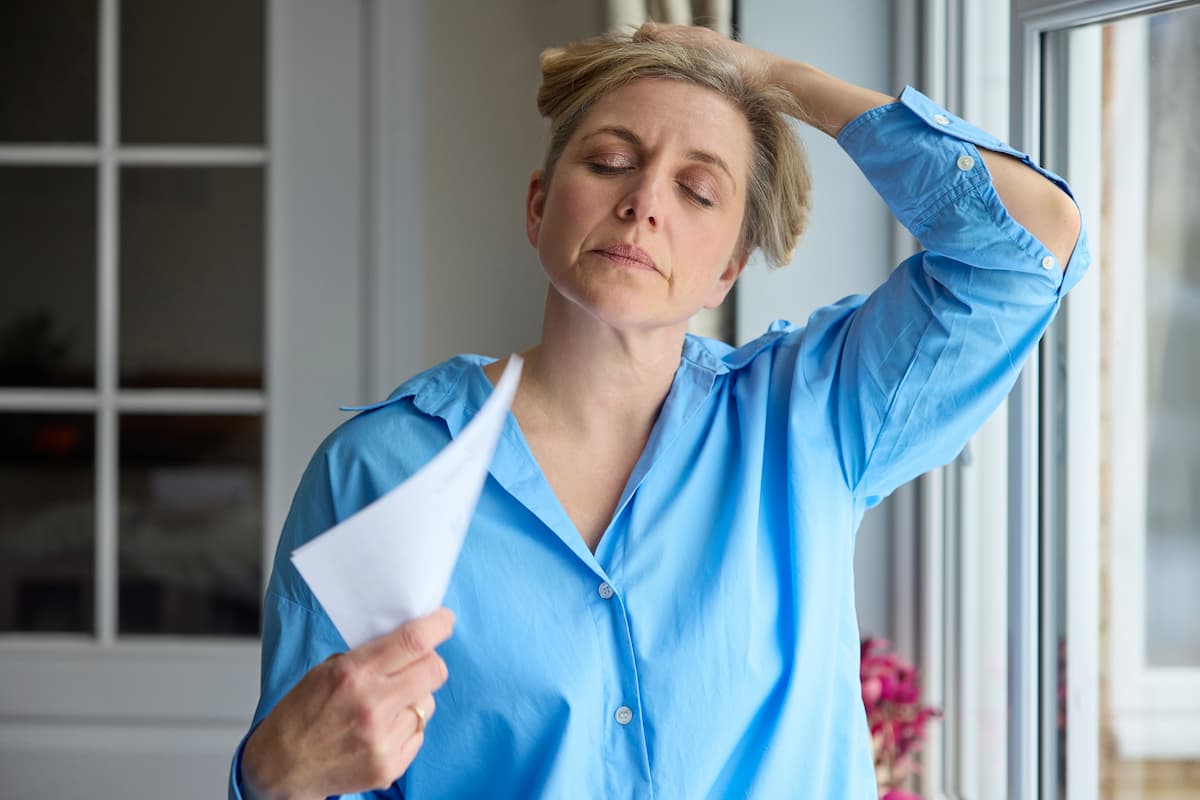
The meta-analysis showed that participants treated with elinzanetant experienced significantly reduced hot flash frequency vs paroxetine, desvenlafaxine, and gabapentin. | Image credit: highwaystarz - stock.adobe.com
“Elinzanetant is the first and only dual NK-targeted therapy blocking NK-1 and NK-3 receptors with demonstrated statistically significantly greater reduction in the frequency and severity of moderate to severe VMS, improvements in sleep disturbance and menopause-related quality of life, compared with placebo,” the authors explained. In the pivotal phase 3 OASIS 1 and OASIS 2 trials, elinzanetant met 4 primary end points and showed significant reductions in the frequency and severity of moderate to severe VMS.2
In the new meta-analysis, the researchers identified 17 randomized controlled trials (RCTs) in the Medline, Embase, and Cochrane databases up to August 2024, with 16 reporting 12-week outcomes.1 Among those 16 trials were 3 assessing elinzanetant, 3 assessing fezolinetant, 2 assessing paroxetine, 5 assessing desvenlafaxine, and 3 assessing gabapentin. The included trials had to report at least 1 of 3 outcomes: change from baseline in VMS frequency and severity, sleep disturbances, or the Menopause-Specific Quality of Life (MENQOL) score.
All but 1 of the studies, a phase 2 RCT assessing elinzanetant, were phase 3 RCTs, and the mean age at baseline ranged from 52 to 56 years across the trials. In all the studies, the daily hot flash frequency exceeded 8. The overall range was 8.5 to 15.4 hot flash events per day. In the meta-analysis, the estimates for between-treatment comparisons were considered statistically significant when the 95% CI did not cross 0 for mean differences (MD) and 1 for odds ratios.
The meta-analysis showed that participants treated with elinzanetant experienced significantly reduced VMS frequency vs paroxetine, desvenlafaxine, and gabapentin. Elinzanetant and fezolinetant had comparable efficacy for reducing hot flash frequency. VMS severity was also significantly less with elinzanetant vs desvenlafaxine 50 mg, although there were no significant differences between elinzanetant and the other treatments evaluated. A significantly higher proportion of participants treated with elinzanetant experienced a 50% or greater reduction in VMS frequency. The meta-analysis showed that participants treated with elinzanetant experienced significantly reduced hot flash frequency vs paroxetine, desvenlafaxine, and gabapentinpared with paroxetine (OR, 2.20) or desvenlafaxine 100 mg (OR, 1.52).
Those treated with elinzanetant also experienced a significantly greater reduction in mean nighttime awakenings vs any dose of desvenlafaxine and compared with paroxetine (MD, –0.82). Based on Patient-Reported Outcomes Measurement Information System Sleep Disturbance—Short Form 8b scores, elinzanetant significantly improved sleep disturbances vs fezolinetant (MD, –2.67). MENQOL changes were similar across treatments.
“Therefore, elinzanetant is a promising option for women seeking relief from menopausal symptoms,” the authors wrote. “The results should be interpreted in the context of estimates being derived from an indirect comparison.”
References
1. Sassarini J, Shulman LP, Giannopoulou A, et al. Comparative efficacy of elinzanetant versus other non-hormonal therapies for the treatment of moderate to severe vasomotor symptoms associated with menopause – a network meta-analysis. Presented at: Presented at: AMCP 2025; March 31-April 3, 2025; Houston, TX. Poster N7.
2. Bayer’s elinzanetant meets all primary and key secondary endpoints in pivotal OASIS 1 and 2 Phase III studies. News release. Bayer. January 8, 2024. Accessed April 10, 2025. https://www.bayer.com/media/en-us/bayers-elinzanetant-meets-all-primary-and-key-secondary-endpoints-in-pivotal-oasis-1-and-2-phase-iii-studies/
Infertility Coverage Boosts ART Use and Pregnancy Success: Richard A. Brook, MS, MBA
August 26th 2025In this episode, Richard A. Brook, MS, MBA, discusses his study showing that infertility treatment coverage increases assisted reproductive technology (ART) use and improves pregnancy outcomes.
Listen
Advancing Women's Health: CVS Health Leader on Access, Technology, and Breaking Stigmas
December 5th 2024On this episode of Managed Care Cast, we speak with CVS Health's vice president and chief medical officer for women's health and genomics about advancements and challenges in women's health, focusing on care access, technology, and maternal outcomes.
Listen
