- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Continuous Glucose Monitoring: An Emerging Standard of Care
The potential value of continuous monitoring of blood glucose and the enzyme-based electrode that underlies continuous glucose monitoring (CGM) in the subcutaneous tissue were described in the 1960s. In 1999, the FDA approved the first “professional” CGM system, which stored data over 3 days for later retrieval and analysis. However, many patients (even volunteers in CGM-based clinical trials) found early-generation systems uncomfortable and difficult to wear. By contrast, current systems are more accurate, provide customizable alerts and alarms, are easier to use and less likely to cause skin irritation, resist interference from acetaminophen, allow for real-time data to be shared and remotely monitored, and are stable enough so as not to require periodic calibrations with SMBG values.
Background
Insulin is a foundation stone of diabetes therapy. It is the life-sustaining drug for everyone with type 1 diabetes (T1D) and an important treatment option in type 2 diabetes (T2D).
Whether given by multiple daily injections (MDI), continuous subcutaneous insulin infusion (CSII), or intranasally, insulin’s low therapeutic index makes precise dosing difficult, even for experienced users. Its absence or deficiency leads to persistent hyperglycemia and vasculopathy, which are leading causes of morbidity and premature mortality, while the acute dangers of insulin-induced hypoglycemia remain the key obstacle to therapy intensification efforts.1 Because insulin dosing decisions depend on knowledge of current and target glucose concentrations, as well as the individual’s likely response to the drug, the ability to measure glucose plays a key role in understanding and managing diabetes.
With the development and commercialization of insulin, the need for glucose quantification increased and technology for measuring glucose in urine and blood improved throughout the latter part of the 20th century. Self-monitoring of blood glucose (SMBG) technology improved throughout the late 1980s with devices that did not require subjective color matching, required less blood and less time, and allowed for wider ranges of hematocrits.2,3 However, SMBG testing remains painful and obtrusive, many patients test at suboptimal frequencies, and individual test results do not provide important trending information.4
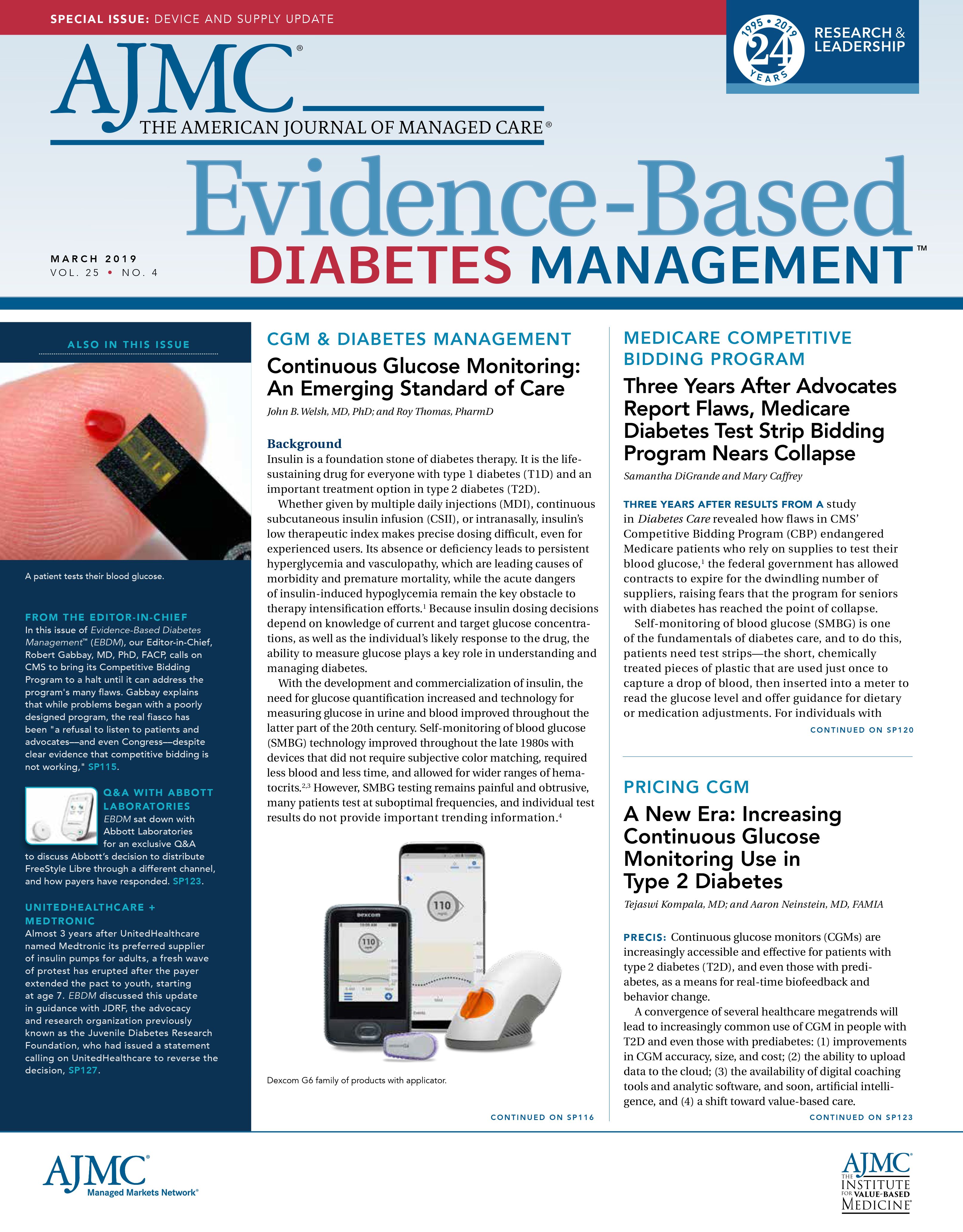
The potential value of continuous monitoring of blood glucose5 and the enzyme-based electrode that underlies continuous glucose monitoring (CGM) in the subcutaneous tissue6 were described in the 1960s. In 1999, the FDA approved the first “professional” CGM system, which stored data over 3 days for later retrieval and analysis. However, many patients (even volunteers in CGM-based clinical trials) found early-generation systems uncomfortable and difficult to wear.7,8 By contrast, current systems are more accurate, provide customizable alerts and alarms, are easier to use9 and less likely to cause skin irritation,10 resist interference from acetaminophen,11 allow for real-time data to be shared and remotely monitored,12 and are stable enough so as not to require periodic calibrations with SMBG values. Single-use transcutaneous sensors from Abbott, Dexcom, and Medtronic last for up to 14 days, while implantable sensors from Senseonics last up to 90 days. Systems are also distinguished by whether or not data are transmitted automatically to a receiving device or rely on the receiving device being brought into proximity with the transmitter. The latter “intermittently scanned” configuration is used by the Abbott FreeStyle Libre system and does not allow for automatic generation of alerts in response to abnormal glucose concentrations.
CGM has revolutionized the way diabetes, especially T1D, is managed. According to several contemporary experts,13 CGM is second only to insulin as the most important advance in caring for those with T1D. When used appropriately, modern CGM can guide decisions leading to average glucose concentrations that are closer to the normal range, reduce the severity of and worry associated with hypoglycemic events, and drive reductions in the cost of complications. Population-level statistics from the T1D Exchange Registry14 show that its adoption is rapidly increasing (from 7% in 2010-2012 to 30% in 2016-2018) and that CGM users with T1D, regardless of insulin delivery method or age, achieve lower glycated hemoglobin (A1C) levels than patients not using the technology.
Nonetheless, only a minority of adults and youth with T1D achieve goals outlined by the American Diabetes Association (ADA) for A1C14 and many patients face barriers when contemplating or continuing CGM use. CGM systems include multiple components, which have variable lifespans, prices, and reimbursement schedules. The extent to which clinical practices advocate for CGM usage and reimbursement also varies, and some practices may mistakenly associate CGM use with the requirement for adoption of a sensor-augmented pump system. Beyond these initial tasks of obtaining and paying for the system, there are additional requirements for long-term success with the technology: wearing the sensors consistently and incorporating CGM data into the daily routine.
The Evidence Base for CGM
Evidence for the clinical benefits of CGM comes from randomized controlled trials (RCTs), patient-reported outcomes, and observational studies. RCT results allow for quantification of prespecified outcomes, such as A1C reduction and hypoglycemia mitigation, for CGM users compared with usual care with SMBG. The Table15-22 summarizes several RCTs using current-generation devices; 3 recent reviews23-25 offer additional commentary. A1C reductions among adults using MDI were studied in the DIAMOND Type 1,15,26 DIAMOND Type 2,16 and GOLD17,27 studies. In these studies, CGM use was associated with significant reductions in A1C, independent of participant age, education, diabetes numeracy, or hypoglycemia awareness. In the DIAMOND study, A1C reduction was larger for subjects with the highest baseline A1C levels.28 The DIAMOND Type 1 and GOLD study results also illustrated that CGM use was associated with significantly reduced time spent in and episodes of hypoglycemia, particularly overnight.
Hypoglycemia reductions among hypoglycemia-prone adults with T1D were studied in the HypoDE19 and I HART CGM18,29 studies. The HypoDE study reported a 72% reduction in the incidence of hypoglycemic events (defined as a series of glucose values ≤54 mg/dL for ≥20 min) for participants in the CGM group. The I HART CGM study highlighted the value of real-time CGM compared with intermittently scanned CGM, in that users of the real-time system experienced larger reductions in hypoglycemia than users of the intermittently scanned system, presumably because of the automatically generated alerts in the former configuration. The impact of CGM use in pregnant women with T1D on neonatal outcomes was recently documented in the CONCEPTT trial, with findings that demonstrated that CGM use improved maternal glycemic control with lower rates of neonatal complications in both insulin pump and MDI users.22,30
Patient-reported outcome studies of CGM have documented the favorable experiences of patients and caregivers. Data collected with the DIAMOND Type 1 study demonstrated a broad satisfaction with the device for participants within the CGM group, which was associated with significant reductions in diabetes distress and hypoglycemia fear, as well as significant increases in hypoglycemia confidence and well-being.31 The reduction in hypoglycemia fear associated with CGM use in adults has been reported in multiple studies.27,32-34 For parents and caregivers of children with T1D, CGM, particularly with remote monitoring, has been found to improve multiple quality-of-life measures, reduce family stress, reduce overall worry and stress, and improve parental sleep.34,35 Although the effects of CGM data sharing among adolescents can vary,36 parents of youth who consistently use CGM report high general quality of life for their children.37
Observational studies have consistently associated higher device utilization rates with improved outcomes. Associations between device interactions and favorable decreases in mean glucose levels were observed by Dunn et al38 (over 6 million data points from users of the Abbott FreeStyle Libre system) and Battelino et al39 (10,501 users of Medtronic sensor-augmented pump systems). Welsh et al reported on 10,000 individuals who transitioned from Dexcom’s G5 to its G6 system.40 Patients who transitioned to the G6 system experienced fewer glucose readings in the hypoglycemic range than during their tenure as G5 users, which was attributed to a new G6-specific “Urgent Low Soon” alert triggered by impending hypoglycemia. A separate observational study reported on 15,000 youth with the ability to share their real-time G5 data with 1 or more remote monitors (“followers”).12 The presence of at least 1 follower was associated with significantly more sensor wear time and higher percentages of glucose values in relative euglycemia. This study’s results support the value of patient engagement and shared responsibility advocated elsewhere41,42 for successful T1D management. Although large patient numbers provide high levels of statistical significance in these studies, they are subject to selection bias and cannot be used to assert causal relationships.
In recognition of the considerable RCT-based and cohort study—based evidence of the utility of CGM use, the ADA issued several recommendations with regard to CGM in early 2019. These recommendations are excerpted in Box 1.43 The International Society for Pediatric and Adolescent Diabetes (ISPAD) agrees on the utility and value of CGM. It asserts that CGM allows improved recommendations for insulin management for all individuals with diabetes and may particularly benefit those with hypoglycemic unawareness. The ISPAD recommendations also concede that CGM presents a more sophisticated glucose monitoring approach than home SMBG; CGM can identify times of hyperglycemia and times of increased risk for hypoglycemia.44
Coverage and Potential Cost Savings of CGM
Three years ago in this journal, a Medicare beneficiary’s quest for CGM coverage was described as a “never-ending story” of appeals and denials.45 In 2017, CMS issued a ruling46 that allows Medicare coverage for beneficiaries who meet certain criteria summarized in Box 2.47,48 Importantly, the CGM system must provide data that guide treatment decisions (“therapeutic” CGM), and a dedicated receiver must be used (alone or in combination with a smartphone app) to view the results. Many commercial payers limit CGM coverage to patients with T1D through a durable medical equipment provision. Only a few cover the technology for patients with T2D using intensive insulin therapy even though these patients’ risk of insulin-induced hypoglycemia is comparable to the risk incurred by patients with T1D.
Coverage of CGM through the pharmacy benefit can allow patients with diabetes to readily pick up their supplies, treatments, and glucose monitors from the pharmacy and not risk being without appropriate monitoring while on insulin. Dexcom CGM systems and components are available on the national preferred formularies of most pharmacy benefit managers and can be provided as a pharmacy benefit if elected by the health plan or plan sponsor.
Improved coverage for CGM systems may result in cost savings in the long run. A recent study by Herman49 showed that 30 years of excellent control in T1D can substantially reduce the incidence of complications, comorbidities, and death; improve quality-of-life; and reduce costs. Mitigation of severe hypoglycemic episodes that require third-party assistance and impose substantial costs on the individual and on the healthcare system is likely to be a significant component of overall cost savings. Even nonsevere hypoglycemic events impose significant costs in the form of workplace absenteeism and lost productivity.50 Cost savings may also result from lower rates of end-organ damage (eg, retinopathy and nephropathy) and reductions in SMBG test strip utilization.51
Next Steps
CGM is revolutionizing our approach to insulin therapy and creating new opportunities for innovation and standardization. It offers patients, and those involved in their care, actionable information that leads to improved outcomes. In the context of clinical trials, CGM-derived metrics, such as time in range, may serve as validated outcomes,52 and CGM-derived average glucose values may reflect the adequacy of glycemic control with more robustness and precision than A1C.53
Currently, there are no professional society recommendations regarding CGM-derived metrics; however, several proposals for optimal use of trend arrows have been made54-57 and there is a guide to integrating CGM data into clinical practice.58 The Ambulatory Glucose Profile is a standardized tool for summarizing and displaying large amounts of CGM data and provides an efficient way to identify behaviors or times for judicious therapy intensification.59
In the near term, category awareness and adoption of CGM systems will likely increase, and systems with the “integrated CGM” designation will be used in a wider range of mobile health-related apps, decision support systems, and automated insulin delivery systems. The devices themselves are likely to become smaller, more accurate, more durable, and more cost-effective. Our expectation and personal experience is that CGM will continue to lessen the cognitive, emotional, physiologic, and economic burdens of insulin-requiring diabetes.
AUTHOR INFORMATION:
John B. Welsh, MD, PhD, is a physician who writes about diabetes technology and has had type 1 diabetes since 1976. Roy Thomas, PharmD, is a pharmacist and a medical science liaison at Dexcom.
CORRESPONDING AUTHOR:
John B. Welsh, MD, PhD, Dexcom, Inc., 6340 Sequence Drive, San Diego, CA 92121; Email: john.welsh@dexcom.com.
DISCLOSURES:
The authors are employees and shareholders of Dexcom, Inc. This work received no specific funding. REFERENCES:
- Adolfsson P, Rentoul D, Klinkenbijl B, Parkin CG. Hypoglycaemia remains the key obstacle to optimal glycaemic control -continuous glucose monitoring is the solution. Eur Endocrinol. 2018;14(2):50- 56. doi: 10.17925/EE.2018.14.2.50.
- Clarke SF, Foster JR. A history of blood glucose meters and their role in self-monitoring of diabetes mellitus. Br J Biomed Sci. 2012;69(2):83-93. doi: 10.1080/09674845.2012.12002443.
- Polonsky KS. The past 200 years in diabetes. N Engl J Med. 2012;367(14):1332-1340. doi: 10.1056/NEJMra1110560.
- Price D, Walker T. The rationale for continuous glucose monitoring-based diabetes treatment decisions and non-adjunctive continuous glucose monitoring use. Eur Endocrinol. 2016;12(1):24- 30. doi: 10.17925/EE.2016.12.01.24.
- Kadish AH. Physiologic monitoring of blood glucose. Calif Med. 1963;98:325-327.
- Updike SJ, Hicks GP. The enzyme electrode. Nature. 1967;214(5092):986-988.
- Bergenstal RM, Tamborlane WV, Ahmann A, et al. Effectiveness of sensor-augmented insulin-pump therapy in type 1 diabetes [erratum in N Engl J Med. 2010;363(11):1092]. N Engl J Med. 2010;363(4):311-320. doi: 10.1056/NEJMoa1002853.
- Diabetes Research in Children Network (DirecNet) Study G. Youth and parent satisfaction with clinical use of the GlucoWatch G2 Biographer in the management of pediatric type 1 diabetes. Diabetes Care. 2005;28(8):1929-1935.
- North R, Pospisil C, Clukey RJ, Parkin CG. Impact of human factors testing on medical device design: validation of an automated CGM sensor applicator [published online February 14, 2019]. J Diabetes Sci Technol. doi: 10.1177/1932296819831071.
- Gisin V, Chan A, Welsh JB. Manufacturing process changes and reduced skin Irritations of an adhesive patch used for continuous glucose monitoring devices. J Diabetes Sci Technol. 2018; 12(3):725- 726 doi: 10.1177/1932296817738076.
- Calhoun P, Johnson TK, Hughes J, Price D, Balo AK. Resistance to acetaminophen interference in a novel continuous glucose monitoring system. J Diabetes Sci Technol. 2018;12(2):393-396. doi: 10.1177/1932296818755797.
- Welsh JB, Derdzinski M, Parker AS, Puhr S, Jimenez A, Walker T. Real-time sharing and following of continuous glucose monitoring data in youth [published online January 30, 2019]. Diabetes Ther. doi: 10.1007/s13300-019-0571-0.
- Edelman SV, Hirsch IB, Pettus JH. Practical Management of Type 1 Diabetes. 2nd edition. West Islip, NY: Professional Communications, Inc; 2014.
- Foster NC, Beck RW, Miller KM, et al. State of type 1 diabetes management and outcomes from the T1D Exchange in 2016-2018. Diabetes Technol Ther. 2019;21(2). doi: 10.1089/dia.2018.0384.
- Beck RW, Riddlesworth T, Ruedy K, et al; DIAMOND Study Group. Effect of continuous glucose monitoring on glycemic control in adults with type 1 diabetes using insulin injections: The DIAMOND randomized clinical trial. JAMA. 2017;317(4):371-378. doi: 10.1001/ jama.2016.19975.
- Beck RW, Riddlesworth TD, Ruedy K, et al; DIAMOND Study Group. Continuous glucose monitoring versus usual care in patients with type 2 diabetes receiving multiple daily insulin injections: a randomized trial. Ann Intern Med. 2017;167(6):365-374. doi: 10.7326/M16-2855.
- Lind M, Polonsky W, Hirsch IB, et al. Continuous glucose monitoring vs conventional therapy for glycemic control in adults with type 1 diabetes treated with multiple daily insulin injections: The GOLD randomized clinical trial. JAMA. 2017;317(4):379-387. doi: 10.1001/ jama.2016.19976.
- Reddy M, Jugnee N, El Laboudi A, Spanudakis E, Anantharaja S, Oliver N. A randomized controlled pilot study of continuous glucose monitoring and flash glucose monitoring in people with type 1 diabetes and impaired awareness of hypoglycaemia. Diabet Med. 2018;35(4):483-490. doi: 10.1111/dme.13561.
- Heinemann L, Freckmann G, Ehrmann D, et al. Real-time continuous glucose monitoring in adults with type 1 diabetes and impaired hypoglycaemia awareness or severe hypoglycaemia treated with multiple daily insulin injections (HypoDE): a multicentre, randomised controlled trial. Lancet. 2018;391(10128):1367-1377. doi: 10.1016/S0140-6736(18)30297-6.
- Šoupal J, Petruzelkova L, Flekac M, et al. Comparison of different treatment modalities for type 1 diabetes, including sensor-augmented insulin regimens, in 52 weeks of follow-up: A COMISAIR Study. Diabetes Technol Ther. 2016;18(9):532-538. doi: 10.1089/ dia.2016.0171.
- van Beers CA, DeVries JH, Kleijer SJ, et al. Continuous glucose monitoring for patients with type 1 diabetes and impaired awareness of hypoglycaemia (IN CONTROL): a randomised, open-label, crossover trial. Lancet Diabetes Endocrinol. 2016;4(11):893-902. doi: 10.1016/S2213-8587(16)30193-0.
- Feig DS, Donovan LE, Corcoy R, et al; CONCEPTT Collaborative Group. Continuous glucose monitoring in pregnant women with type 1 diabetes (CONCEPTT): a multicentre international randomised controlled trial. Lancet. 2017;390:2347-2359. doi: 10.1016/ S0140-6736(17)32400-5.
- Hirsch IB, Battelino, Peters AL, Chamberlain JJ, Aleppo G, Bergenstal RM. Role of continuous glucose monitoring in diabetes treatment. American Diabetes Association website. professional. diabetes.org/sites/professional.diabetes.org/files/media/ final_ada-abbott_cgm_compendium_final.pdf. Published June 5, 2018. Accessed January 29, 2019.
- Welsh JB. Role of continuous glucose monitoring in insulin-requiring patients with diabetes. Diabetes Technol Ther. 2018;20(S2):S242-S249. doi: 10.1089/dia.2018.0100.
- Edelman SV, Argento NB, Pettus J, Hirsch IB. Clinical implications of real-time and intermittently scanned continuous glucose monitoring. Diabetes Care. 2018;41(11):2265-2274. doi: 10.2337/dc18-1150.
- Beck RW, Riddlesworth TD, Ruedy KJ, et al; DIAMOND Study Group. Effect of initiating use of an insulin pump in adults with type 1 diabetes using multiple daily insulin injections and continuous glucose monitoring (DIAMOND): a multicentre, randomised controlled trial. Lancet Diabetes Endocrinol. 2017;5(9):700-708. doi: 10.1016/S2213-8587(17)30217-6.
- Olafsdottir AF, Polonsky W, Bolinder J, et al. A randomized clinical trial of the effect of continuous glucose monitoring on nocturnal hypoglycemia, daytime hypoglycemia, glycemic variability, and hypoglycemia confidence in persons with type 1 diabetes treated with multiple daily insulin injections (GOLD-3). Diabetes Technol Ther. 2018;20(4):274-284. doi: 10.1089/dia.2017.0363.
- Billings LK, Parkin CG, Price D. Baseline glycated hemoglobin values predict the magnitude of glycemic improvement in patients with type 1 and type 2 diabetes: subgroup analyses from the DIAMOND Study Program. Diabetes Technol Ther. 2018;20(8):561-565. doi: 10.1089/dia.2018.0163.
- Reddy M, Jugnee N, Anantharaja S, Oliver N. Switching from flash glucose monitoring to continuous glucose monitoring on hypoglycemia in adults with type 1 diabetes at high hypoglycemia risk: the extension phase of the I HART CGM study. Diabetes Technol Ther. 2018; 20(11), 751-757. doi: 10.1089/dia.2018.0252.30.
- Feig DS, Corcoy R, Donovan LE, et al; CONCEPTT Collaborative Group. Pumps or multiple daily injections in pregnancy involving type 1 diabetes: a prespecified analysis of the CONCEPTT randomized trial. Diabetes Care. 2018;41(12):2471-2479. doi: 10.2337/dc18-1437.
- Polonsky WH, Hessler D, Ruedy KJ, Beck RW, Group DS. The impact of continuous glucose monitoring on markers of quality of life in adults with type 1 diabetes: Further findings from the DIAMOND randomized clinical trial. Diabetes Care. 2017;40(6):736-741. doi: 10.2337/dc17-0133.
- Beck RW, Lawrence JM, Laffel L, et al; Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group. Quality-of-life measures in children and adults with type 1 diabetes: Juvenile Diabetes Research Foundation Continuous Glucose Monitoring randomized trial. Diabetes Care. 2010;33(10):2175-2177. doi: 10.2337/dc10-0331.
- Polonsky WH, Hessler D. What are the quality of life-related benefits and losses associated with real-time continuous glucose monitoring? A survey of current users. Diabetes Technol Ther. 2013;15(4):295-301. doi: 10.1089/dia.2012.0298.
- Erie C, Van Name MA, Weyman K, et al. Schooling diabetes: Use of continuous glucose monitoring and remote monitors in the home and school settings. Pediatr Diabetes. 2018;19(1):92-97. doi: 10.1111/pedi.12518.
- Burckhardt MA, Roberts A, Smith GJ, Abraham MB, Davis EA, Jones TW. The use of continuous glucose monitoring with remote monitoring improves psychosocial measures in parents of children with type 1 diabetes: a randomized crossover trial. Diabetes Care. 2018;41(12):2641-2643. doi: 10.2337/dc18-0938.
- Messer LH, Johnson R, Driscoll KA, Jones J. Best friend or spy: a qualitative meta-synthesis on the impact of continuous glucose monitoring on life with type 1 diabetes. Diabet Med. 2018;35(4):409- 418. doi: 10.1111/dme.13568.
- Giani E, Snelgrove R, Volkening LK, Laffel LM. Continuous glucose monitoring (CGM) adherence in youth with type 1 diabetes: associations with biomedical and psychosocial variables. J Diabetes Sci Technol. 2017;11(3):476-483. doi: 10.1177/1932296816676280.
- Dunn TC, Xu Y, Hayter G, Ajjan RA. Real-world flash glucose monitoring patterns and associations between self-monitoring frequency and glycaemic measures: A European analysis of over 60 million glucose tests. Diabetes Res Clin Pract. 2018;137:37-46. doi: 10.1016/j. diabres.2017.12.015.
- Battelino T, Liabat S, Veeze HJ, Castañeda J, Arrieta A, Cohen O. Routine use of continuous glucose monitoring in 10 501 people with diabetes mellitus. Diabet Med. 2015;32(12):1568-1574. doi: 10.1111/dme.12825.
- Welsh JB, Gao P, Derdzinski M, et al. Accuracy, utilization, and effectiveness comparisons of different continuous glucose monitoring systems [published online January 25, 2019]. Diabetes Technol Ther. doi: 10.1089/dia.2018.0374.
- Hanna KM, Dashiff CJ, Stump TE, Weaver MT. Parent-adolescent dyads: association of parental autonomy support and parent-adolescent shared diabetes care responsibility. Child Care Health Dev. 2013;39(5):695-702. doi: 10.1111/j.1365-2214.2012.01373.x.
- Marker AM, Noser AE, Clements MA, Patton SR. Shared responsibility for type 1 diabetes care is associated with glycemic variability and risk of glycemic excursions in youth. J Pediatr Psychol. 2018;43(1):61-71. doi: 10.1093/jpepsy/jsx081.
- American Diabetes Association. 7. Diabetes technology: standards of medical care in diabetes-2019. Diabetes Care. 2019;42(suppl 1):S71-S80. doi: 10.2337/dc19-S007.
- Sherr JL, Tauschmann M, Battelino T, et al. ISPAD Clinical Practice Consensus Guidelines 2018: diabetes technologies. Pediatr Diabetes. 2018;19(suppl 27):302-325. doi: 10.1111/pedi.12731.
- Patrick D. A Medicare appeal for CGM coverage: one patient’s never-ending story. Am J Manag Care. 2016;22(SP7):SP258-SP261.
- Centers for Medicare and Medicaid Services. CMS Rulings: Ruling No: [CMS-1682-R]. CMS website. cms.gov/Regulations-and Guidance/Guidance/Rulings/Downloads/CMS1682R.pdf. Published January 12, 2017. Accessed February 22, 2019.
- Is Dexcom covered by Medicare? Dexcom website Rev012. dexcom. com/faq/medicare. Accessed February 14, 2019.
- Centers for Medicare and Medicaid Services. Medicare coverage of diabetes supplies & services. Medicare website. medicare.gov/pubs/ pdf/11022-Medicare-Diabetes-Coverage.pdf. Revised August 2018. Accessed February 14, 2019.
- Herman WH, Braffett BH, Kuo S, et al. What are the clinical, quality-of-life, and cost consequences of 30years of excellent vs. poor glycemic control in type 1 diabetes? J Diabetes Complications. 2018;32(10):911-915. doi: 10.1016/j.jdiacomp.2018.05.007.
- Brod M, Christensen T, Thomsen TL, Bushnell DM. The impact of non-severe hypoglycemic events on work productivity and diabetes management. Value Health. 2011;14(5):665-671. doi: 10.1016/j. jval.2011.02.001.
- Puhr S, Calhoun P, Welsh JB, Walker TC. The effect of reduced self-monitored blood glucose testing after adoption of continuous glucose monitoring on hemoglobin A1C and time in range. Diabetes Technol Ther. 2018;20(8):557-560. doi: 10.1089/dia.2018.0134.
- Beck RW, Bergenstal RM, Riddlesworth T, et al. Validation of time in range as an outcome measure in clinical trials. Diabetes Care. 2019;42(3):400-405. doi: 10.2337/dc18-1444.
- Beck RW, Connor CG, Mullen DM, Wesley DM, Bergenstal RM. The fallacy of average: how using HbA1C alone to assess glycemic control can be misleading. Diabetes Care. 2017;40(8):994-999. doi: 10.2337/dc17-0636.
- Aleppo G, Laffel LM, Ahmann AJ, et al. A practical approach to using trend arrows on the Dexcom G5 CGM system for the management of adults with diabetes. J Endo Soc. 2017;1(12):1445-1460. doi: 10.1210/js.2017-00388.
- Laffel LM, Aleppo G, Buckingham BA, et al. A practical approach to using trend arrows on the Dexcom G5 CGM system to manage children and adolescents with diabetes. J Endocr Soc. 2017;1(12):1461- 1476. doi: 10.1210/js.2017-00389.
- Kudva YC, Ahmann AJ, Bergenstal RM, et al. Approach to using trend arrows in the FreeStyle Libre flash glucose monitoring systems in Adults. J Endocr Soc. 2018;2(12):1320-1337. doi: 10.1210/js.2018-00294.
- Bianchi C, Aragona M, Rodia C, et al. Freestyle Libre trend arrows for the management of adults with insulin-treated diabetes: a practical approach. J Diabetes Complications. 2019;33(1):6-12. doi: 10.1016/j.jdiacomp.2018.10.012.
- Aleppo G, Webb K. Continuous glucose monitoring integration in clinical practice: a stepped guide to data review andinterpretation. J Diabetes Sci Technol. 2019;45(1 suppl):3S-20S). doi: 10.1177/0145721718818066.
- Mullen DM, Bergenstal R, Criego A, Arnold KC, Goland R, Richter S. Time savings using a standardized glucose reporting system and ambulatory glucose profile. J Diabetes Sci Technol. 2018;12(3):614- 621. doi: 10.1177/1932296817740592.
Specialty and Operator Status Influence Electronic Health Record Use Variation
January 22nd 2026Operators demonstrated specialty-specific differences in electronic health record efficiency, timeliness, and after-hours use, highlighting how workflow and training shape documentation behaviors across medical disciplines.
Read More
Exploring Pharmaceutical Innovations, Trust, and Access With CVS Health's CMO
July 11th 2024On this episode of Managed Care Cast, we're talking with the chief medical officer of CVS Health about recent pharmaceutical innovations, patient-provider relationships, and strategies to reduce drug costs.
Listen

