- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
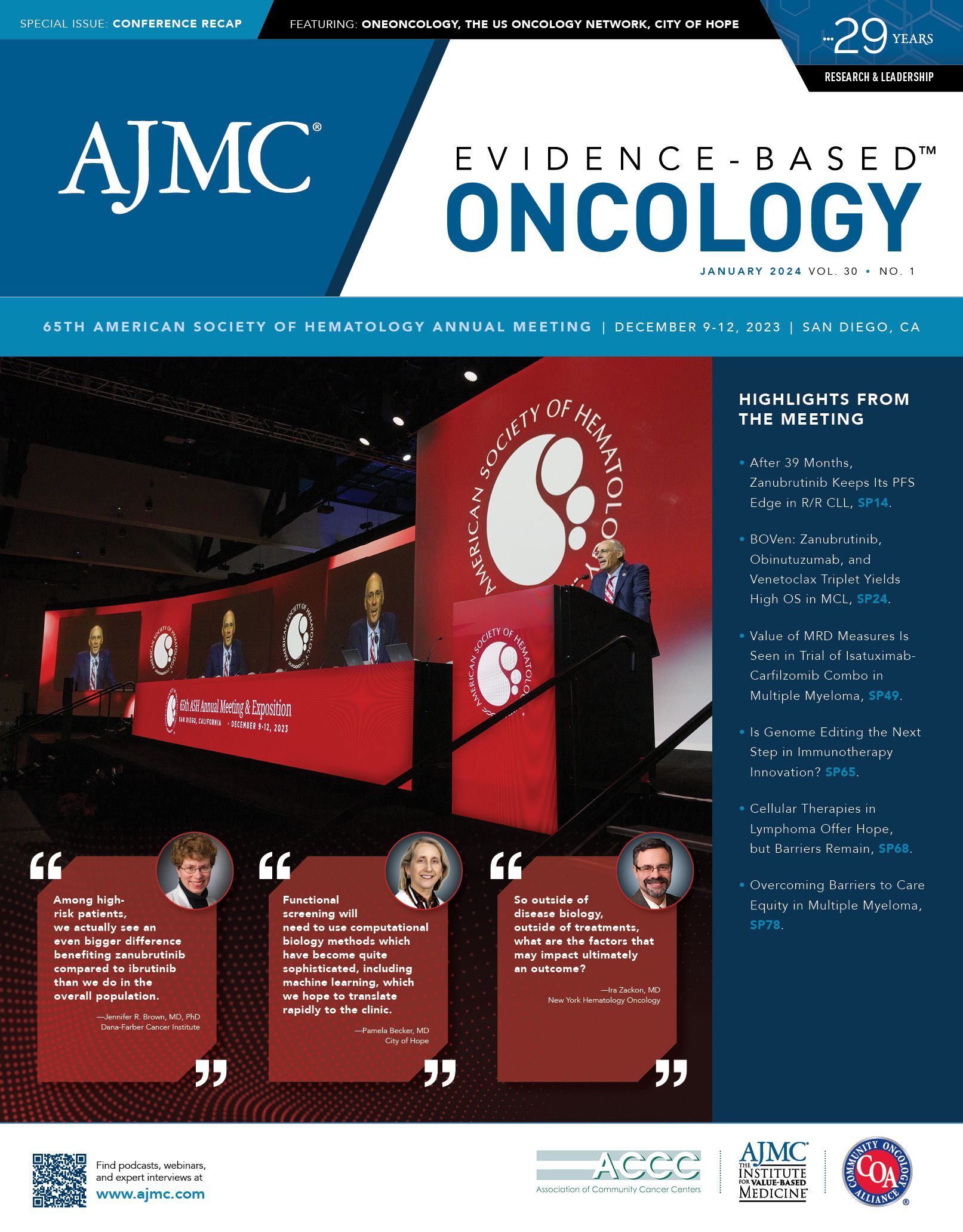
CLL Society’s Koffman Says ASH 2023 Offered “Evolutionary” Changes
Brian Koffman, MDCM, DCFP, FCFP, DABFP, MSEd, is the executive vice president and chief medical officer of CLL Society,1 an organization he cofounded after his own diagnosis in 2005. Koffman is a retired board-certified family physician, medical educator, and clinical professor at the Keck School of Medicine of the University of Southern California. He
Brian Koffman, MDCM | Image credit: CLL Advocates Network

spoke with Evidence-Based Oncology™ about the most important takeaways from the 65th American Society of Hematology (ASH) Annual Meeting and Exposition for patients living with chronic lymphocytic leukemia (CLL).
Q. From your perspective, what were the most important developments at this year’s ASH meeting?
Koffman: ASH 2023 brought some important evolutionary changes to how we’re going to treat CLL, but I don’t think there were any revolutionary changes or major practice changing presentations. Some of the data were continuations, with more follow-up data than had been previously presented.
One important paper reported the data that directly compared zanubrutinib to ibrutinib.2 We had previously seen data that suggested that zanubrutinib not only was freer of adverse events, but also offered better outcomes in terms of progression-free survival. It was, in other words, more efficacious. This year, we saw continuation of that data that’s at 3 years in some cases, and we saw those curves continue. And it becomes clear that zanubrutinib not only has fewer adverse events but seems to have improved progression-free survival compared to ibrutinib. So it continues to bear out and has important implications for therapy for patients down the line.
There were a number of papers that addressed the efficacy of various combinations of therapy, particularly combining BTK inhibitors with the BCL2 blocker. Most of this was data was around a combination of ibrutinib and venetoclax, [with] very high response rates. The vast majority of patients were able to get to undetectable minimal residual disease, with many patients having a prolonged drug-free period, especially when this combination is used in the frontline setting. I think there was some encouraging data in terms of various RT therapies and the use pirtobrutinib for one of the unmet needs in CLL, Richter transformation, showing impressive response rate and durability.3 But we still have a long way to go.
Q. When you consider the possibility of combination therapy, what would that mean for patients, assuming everyone could have access? Some patients already have issues gaining access to a second-generation BTK inhibitor.
Koffman: The use of oral combinations—an oral BTK inhibitor, and an oral BCL2—is obviously appealing. It’s appealing because it’s all oral healing. And because most of these are limited duration, it’s appealing because the patients can often get off the medications and have a real long glide path afterward. And depending on the length of that glide path, and the depth of their remission, they may be able to use either or both of the medications again and get a good response time. So that’s very encouraging. But the big problem is the combination that’s been best studied—ibrutinib and venetoclax—doesn’t have a clear path forward for approval in the United States. And if it’s not approved, it may be difficult for patients to get it paid for. For many patients, these medications will be prohibitively expensive—just 1 medication would be difficult for patients to be able to afford, let alone a combination. So this will limit the applicability of this important research, which is a problem because patients may be not getting their best option.
Q. Speaking of financial challenges, I wanted to address the issue of financial toxicity in CLL, given that with some of today’s therapies, patients may take them for a long time. What types of challenges do you hear about at CLL Society?
Koffman: In CLL Society we say, if you’ve seen one CLL patient, you’ve seen one CLL patient. We know that 20% of patients may never need therapy. But when patients do need therapy, we know, at least at this point, for the vast majority of CLL patients, no treatment is curative, and many patients will be able to kick the can down the road for a while. Depending on the prognostic markers [present] that may be a relatively short or relatively longer period. Eventually, almost everyone relapses on whatever the first therapy is, and they need a second therapy. We have excellent first- and second-line therapies. But by the time you get to the third therapy, we don’t have a lot of options for clinical trials. And all of these different treatments are extraordinarily expensive for patients. So when you’re getting beyond the first lines of therapy, you’re having to look at things that are maybe more experimental—such as additions of drugs. And this can become prohibitively expensive for patients.
There’s a lot of excitement and cost savings associated with clinical trials. But patients have to understand with a clinical trial, maybe the experimental drug is paid for. But maybe the drug that’s combined with it—which is already on the market and is not in the standard of care—or the bone marrow biopsy and aspiration or imaging test or the blood work may not all be paid for and that can be extraordinarily expensive. Clinical trials are often monitoring the patient closely, and that’s really good. But the expenses can be very high, and your insurance doesn’t always cover all the expenses related to the trial.
Q. That leads us to our next question: More than half of all Medicare beneficiaries are now in Medicare Advantage (MA). We are hearing more about how the rise of MA plans affects patients with CLL who are diagnosed with or living with this disease as they attempt to gain access to advanced therapeutics. What are you hearing?
Koffman: Traditional Medicare covers you anywhere in the country with any doctor, but there can be significant copays and direct costs to the patient. There is Medigap insurance, but you have to set that up at the time you start Medicare; it can be difficult to set up later. Insurance is very complicated when someone is considering Medicare; as a result, a lot of patients go to Medicare Advantage. And it does have advantages, because generally everything’s included. The costs are well covered if everything you do is inside that system. However, if you want to see a specialist outside that system, or if you want a clinical trial that’s not part of their system, while on paper all this is accessible, it can involve a lot of difficulties for patients to get those services.
And as I said, you know one CLL patient, you know one CLL patient. Each of us has different needs and a different path. Even the guidelines offer all kinds of different options, and individualizing treatment—that can be more difficult when [a patient] is inside a Medicare Advantage plan because that plan may have certain guidelines that they’re following; if [a patient needs to] get outside those guidelines or get into a clinical trial or get a different option, that can be very difficult for patients to access. That said, if the patient fits into a very indolent course and does well on conventional therapies in spite of CLL, MA can be a big money saver for them.
Q. Is there anything else from this past ASH meeting that you would like to mention?
Koffman: I was very encouraged that for the first time that I know of there was an oral presentation that talked about the emotional journey of patients going through CLL during active observation or the “watching and waiting” period, which is being recognized by the hematology professional community. This is not necessarily “good cancer,” but a cancer that’s associated with a lot of anxiety and difficulty around decisions. And for that to be recognized with an oral presentation, very encouraging.
References
- CLL Society. Accessed December 17, 2023. https://cllsociety.org/
- Brown JR, Eichhorst B, Lamanna N, et al. Extended follow-up of ALPINE randomized phase 3 study confirms sustained superior progression-free survival of zanubrutinib versus ibrutinib for treatment of relapsed/refractory chronic lymphocytic leukemia and small lymphocytic lymphoma (R/R CLL/SLL). Presented at: 65th American Society of Hematology Annual Meeting & Exposition; December 9-12, 2023; San Diego, CA. Paper No. 0202. doi:10.1182/blood-2023-174289
- Wierda WG, Shah NN, Cheah CY, et al Pirtobrutinib in Richter transformation: updated efficacy and safety results with 18-month survival follow-up from phase 1/2 BRUIN study. Presented at: 65th American Society of Hematology Annual Meeting & Exposition; December 9-12, 2023; San Diego, CA. Abstr 1737 https://ash.confex.com/ash/2023/webprogram/Paper181108.html
Evolving Treatment Paradigms for Hematologic Malignancies in Community Oncology Settings
January 11th 2026In an interview during ASH 2025, Ontada's Ira Zackon, MD explores the role of BTK inhibitors in chronic lymphocytic leukemia treatment, highlighting real-world challenges and emerging therapy strategies.
Read More
