- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Children With Sickle Cell Disease Experience Severe COVID-19 Infection
In a registry-based analysis, more hospitalized children with SCD and COVID-19 had severe infection requiring supplemental oxygen, compared with the general population.
This article was originally published by HCPLive.
A new analysis of data from the Pediatric COVID-19 United States Registry revealed children with sickle cell disease (SCD) are at risk of severe disease with SARS-CoV-2 infection.1
According to the registry-based analysis, approximately one-third of children with SCD required hospitalization with nearly half of the children with SCD who were hospitalized requiring supplemental oxygen.
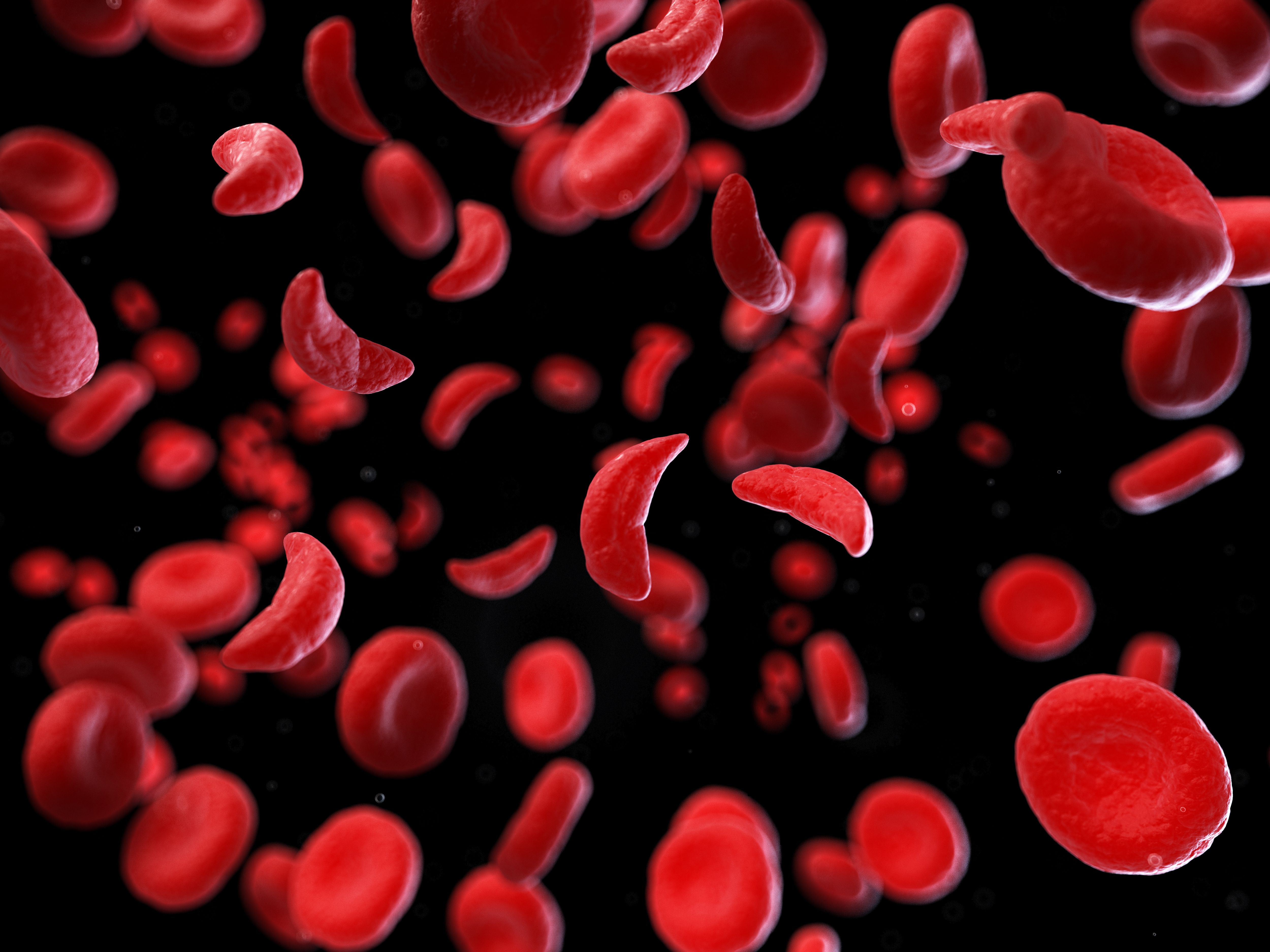
Model of Sickled Cells | image credit: Sebastian Kaulitzki - stock.adobe.com
“Our results indicate that a higher proportion of hospitalized children with SCD and COVID-19 had severe infection requiring supplemental oxygen compared to the general population, a finding that has been showing in other viral illnesses, particularly influenza,” wrote the investigative team led by Aleksandra S. Dain, MD, division of hematology, department of pediatrics at the Children’s Hospital of Philadelphia.
Adults with SCD are known to be at increased risk of SARS-CoV-2-related complications, including hospitalization, compared with a healthy population.2 Its exact mechanism remains unknown, but research has cited pre-existing end-organ damage as a potential cause. Hospitalization and mortality in SCD are often comparable to non-SCD populations with similar comorbidities.
Among children, those with underlying comorbidities and those who develop multisystem inflammatory syndrome (MIS-C) experience elevated morbidity and mortality secondary to SARS-CoV-2 infection.3 Reports suggest SCD is a risk for severe COVID-19 and hospitalization, but limitations of these findings include single-center populations or a lack of non-SCD comparators.
In this registry-based analysis, Dain and colleagues sought to describe the clinical characteristics and outcomes of both acute COVID-19 and MIS-C in pediatric patients with SCD and compare these findings with other populations.1
The Pediatric COVID-19 US Registry involved surveillance of pediatric COVID-19 cases diagnosed between March 2020 and April 2021. Eligible cases were individuals ≤ 21 years of age diagnosed with laboratory-confirmed SARS-CoV-2 infection. Hospitalizations, including intensive care unit (ICU) admissions, were documented.
Overall, the registry included 13,140 patients, and the primary analysis used 10,974 children with complete study data. Investigators identified a total of 263 patients with SCD. The study population had a median age of 12 years, and 140 (53%) patients were male.
Among those with SCD, 91 (35%) patients were hospitalized due to COVID-19, compared with 114 (34%) in the immune-compromised group and 1485 (14%) in the general pediatric populations. Notably, significantly fewer hospitalized patients with SCD required ICU care (18%) compared with the immune-compromised (32%; P = .016) and general pediatric groups (35%; P = .001).
In children who were hospitalized, those in the SCD cohort demonstrated the highest proportion of patients requiring supplemental oxygen (45%) compared with the immune-compromised (37%) and general pediatric (35%) cohorts. However, the between-group differences were not statistically significant (P = .17).
A total of 4 hospitalized (4.4%) patients with SCD in the cohort were diagnosed with MIS-C, compared with 2 (1.75%) and 288 (19.4%) in the hospitalized immune-compromised and general pediatric groups, respectively. All those with SCD or immune-compromised required ICU admission, compared with two-thirds of general pediatric patients.
Despite the COVID-19 global public health emergency ending, Dain and colleagues indicated that SARS-CoV-2 infection remains a persistent and relevant respiratory pathogen, particularly for those with SCD.
“The opportunity remains to protect vulnerable patients, including those with SCD, through optimization of vaccination and supportive care,” they wrote.
References
- Dain AS, Diorio C, Fisher BT, et al. Description of a national, multi-center registry of patients with sickle cell disease and SARS-CoV-2 infection: Data from the Pediatric COVID-19 United States Registry. Pediatr Blood Cancer. Published online March 12, 2024. doi:10.1002/pbc.30909
- Hoogenboom WS, Alamuri TT, McMahon DM, et al. Clinical outcomes of COVID-19 in patients with sickle cell disease and sickle cell trait: A critical appraisal of the literature. Blood Rev. 2022;53:100911. doi:10.1016/j.blre.2021.100911
- Kaushik A, Gupta S, Sood M, Sharma S, Verma S. A Systematic Review of Multisystem Inflammatory Syndrome in Children Associated With SARS-CoV-2 Infection. Pediatr Infect Dis J. 2020;39(11):e340-e346. doi:10.1097/INF.0000000000002888
