- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Cancer Care Pathways: Hopes, Facts, and Concerns
Cancer pathways can potentially improve patient outcomes and reduce costs. Recent concerns about pathway adoption deserve attention, including excessive administrative burden to clinics.

The oncology landscape is rapidly changing, in great part due to unprecedented innovations in diagnostic and treatment technologies.1 Ironically, the same advances in cancer therapeutics that now benefit many patients also dramatically increase the complexity and costs of oncologic care.2 The latter have forced stakeholders to develop new strategies to provide high-quality, state-of-the-art cancer care while simultaneously bending the cost curve.3 Among the several new models of cancer care delivery and reimbursement that are currently under evaluation, cancer care pathways (CCPs) are emerging as a strategy to provide evidence-based oncology care at lower costs through reductions in unnecessary treatment variations.4
The rationale for adopting CCPs departs from the following assumptions:
- Cancer care and costs vary substantially across clinics and providers, a concern that many studies have confirmed to be true.5-8
- Low-value treatments account for at least a fraction of the variation, including the use of costly, but marginally effective, drug regimens.9
- Adoption of CCPs can change physician behavior to prioritize the use of high-value evidence-based treatments, thereby improving patient outcomes and reducing the use of costly therapies that are either marginally effective or more toxic.10
To the extent that these assumptions hold true, CCPs have great potential to succeed as a model for the delivery of high-value cancer care. But do they hold true?
As an increasing number of cancer care clinics are adopting CCPs, either voluntarily or as required by payers, an early look at pathways’ performance becomes necessary to inform stakeholders whether the investments in CCPs have resulted in the expected returns and what efforts need to take place to optimize pathway development, if any.
Our goal here is to discuss the impact of adoption of CCPs on treatment variation, patient outcomes, and cancer care costs, based on published literature. This review focuses on commercially available CCPs (ie, computer-based treatment decision programs offered by vendors as part of oncology management programs) because most of the available literature pertains to this particular type of pathway. Several academic cancer centers have developed their own CCPs for internal use, including the University of Washington, Dana-Farber Cancer Institute, and University of Tennessee, to name a few.11-13 A review of these programs is beyond the scope of this article, as very little published literature is available to inform their performance. Although this review is by no means comprehensive or exhaustive, it provides some insights about the promises and concerns regarding adoption of CCPs.
The Process of Developing Cancer Care Pathways
To ensure an informed discussion of how CCPs impact outcomes, a brief explanation is in order to define CCPs and clarify the process by which pathways are developed. Pathways consist of complex electronic treatment decision support tools that provide evidence-based treatment recommendations to physicians at the point-of-care for individual patients. These tools are often integrated with electronic health records (EHRs) in a manner that allows managers to evaluate whether the treatments actually delivered were concordant or discordant with pathway recommendations. This information is relevant for monitoring pathway adherence. Pathways, in general, cover several cancers at all stages. With a primary focus on drug regimens, some CCP programs have also developed content for supportive care and radiation therapy.10,14
CCP programs typically apply a hierarchical order of criteria to select the treatments to be included in the pathways. The first criterion is treatment efficacy, wherein regimens of superior efficacy receive top priority for pathway inclusion. As a side note, the available literature does not clearly specify the disease endpoints used to measure efficacy (eg, overall vs progression-free survival, response rates, etc.). Toxicity is the next selection criterion applied to regimens of similar efficacy; those with lower toxicity and similar efficacy receive priority. Drug cost is the third and last selection criterion; pathways prioritize regimens of lower cost when efficacy and toxicity are similar.
Most CCPs emanate from collaborative efforts involving physician network groups, healthcare payers, and oncology management—program consulting firms. Physicians elect disease-specific committees that appraise the current evidence and select the treatments for pathway inclusion. Leaders of several CCP programs have publically declared that the committees offer an opportunity to all physicians using the pathways to comment on the contents and participate in the process of pathway treatment selection.10,14,15 The committees are also in charge of continuously updating pathway contents—as evidence becomes available—to support the use of novel therapies.
Once physician committees decide on the contents of a pathway, the oncology management programs integrate the treatments into the electronic supporting tools and offer technical assistance to network physicians using the pathways in daily practice. Oncology management programs also assist clinics in reporting pathway adherence to healthcare payers, and help monitor patient outcomes and costs. Payers offer financial incentives to maximize pathway adherence, usually in the form of higher fees for on-pathway drugs and by increasing the reimbursement for evaluation and management charges for adherent physicians.
Cancer Care Pathways and Treatment Variation
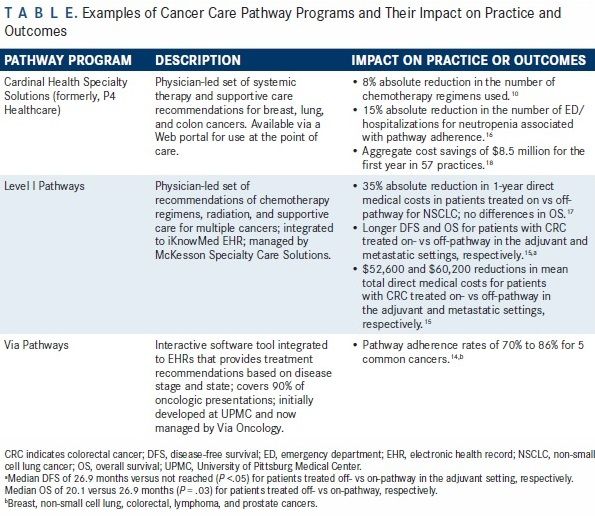
The central hypothesis for CCP use is that adherence to pathways reduces costs and maintains quality of care by curtailing the use of unnecessary and costly oncologic treatments. Surprisingly, there is very scant published evidence to support or reject this hypothesis. After a short PubMed literature search, I could only retrieve 1 article reporting on the impact of the Cardinal Health Specialty Solutions (formerly, P4 Healthcare) pathway on treatment variations. The study compared the number of chemotherapy regimens used for breast, lung, and colorectal cancers in the year preceding and the year following pathway implementation, in several practices located in Michigan.10
Table
Physicians used 168 and 136 distinct regimens in the years pre- and post-pathways implementation, respectively, which represents an 8% absolute reduction in treatment variation (). Interestingly, 10% of the study population accounted for 81% of the reduction in the number of drug regimens used, suggesting that a minority of patients drive most of the treatment variation, perhaps because of higher disease complexity. Although this single report does not provide any firm conclusions about the effects of pathways on treatment variation, the reduction in the number of chemotherapy regimens used was quite modest. An important point to note is that the report does not provide any information on the cost of the chemotherapy regimens avoided to establish a causal relationship between reductions in treatment variation and costs.
Cancer Care Pathways and Patient Outcomes
Table
At least 1 report indicates that adherence to CCPs reduces the number of emergency department (ED) visits and hospital admissions for treatment-related complications (). Kreys et al evaluated the effect of adherence to the Cardinal Health Specialty Solutions supportive care pathways on ED visits and hospitalizations for neutropenia, anemia, and chemotherapy-induced nausea and vomiting in patients with breast, lung, and colorectal cancers. Compared with patients who received off-pathway supportive care, pathway adherence was associated with a 15% absolute reduction in ED visits and hospitalizations for neutropenia (adjusted odds-ratio, 0.42; 95% CI, 0.30-0.58).16 The study demonstrated no clinically or statistically significant differences in admissions for anemia or chemotherapy-induced nausea and vomiting. Pathway adherence was associated with lower expenditures for hospitalizations to manage neutropenia and anemia, and with lower expenditures related to the use of granulocyte colony—stimulating factors and antiemetics.
Table
Current evidence suggests that adherence to CCPs results in either a neutral or favorable effect on survival outcomes, depending on the disease and treatment setting (adjuvant vs metastatic) (). Using EHR and pathway reporting data, Neubauer et al conducted a cost-effectiveness analysis of adherence to Level I Pathways among 1409 patients with non-small cell lung cancer (NSCLC) treated at several US Oncology network clinics. After adjusting for patient characteristics and line of therapy, the study showed no statistically significant difference in 1-year overall survival (OS) (HR, 0.95; 95% CI, 0.77-1.16) between patients treated on- versus off-pathway.17 Hoverman et al also utilized EHR and claims data to compare disease-free survival (DFS) and OS in patients treated on versus off Level I Pathways with adjuvant and palliative chemotherapy for stage III and IV colorectal cancer, respectively.15 Pathway adherence was associated with a substantial increase in DFS (HR, 4.98; 95% CI, 2.11-11.74 for non-adherence) in the adjuvant setting and prolongation of OS (HR, 1.57; 95% CI, 1.04-2.39 for non-adherence) in the metastatic setting, respectively.
Cancer Care Pathways and Direct Medical Costs
Table
Cost is perhaps the outcome measure for which the evidence is most robust to support the use of CCPs. At least 3 economic evaluations suggest that adherence to CCPs reduces direct medical costs (). The cost-effectiveness analysis of adherence to Level I Pathways for NSCLC found that total mean direct medical costs were 35% lower in patients treated on- versus off-pathway ($18,042 vs $27,737 per patient), suggesting that pathway adherence saves costs in this disease setting.17 The study by Hoverman et al showed mean reductions in total direct medical costs of $52,641 and $60,163 associated with adherence to Level I Pathways for adjuvant and metastatic treatment of colorectal cancer, respectively.15 Chemotherapy costs accounted for most of the cost reductions in this study.
In a time series study that compared 57 practices that participated in the Cardinal Health Specialty Solutions pathway with 43 non-participant practices, pathway participation was associated with an aggregate $8.5 million in cost savings 1 year after pathway implementation, the majority of the savings being related to drug expenditures.18 In a study of the same pathway implemented in different hospitals, drug expenditures did not differ before and after pathway implementation, although mean hospitalization costs were reduced by $1400 per patient.19
Collectively, these studies provide preliminary evidence that high adherence to CCPs can improve patient outcomes and reduce costs. The effect of pathways on treatment variation remains unclear, however. The results seem to vary considerably across hospital, disease, and treatment settings. Although the analyses show a consistent favorable impact of CCP adherence on total costs, the evaluations provide conflicting data as to the components of care responsible for the cost savings (ie, chemotherapy use, hospitalization, or supportive care).
Areas of Uncertainty and Concerns
These published studies contain several limitations that preclude an accurate estimate of the impact of CCPs on patient outcomes and costs. All study designs are observational and subject to selection bias—patients treated off-pathway may systematically differ from patients treated on-pathway with respect to characteristics that affect outcomes. Pre- and post-type of study designs do not account for changes in practice that occur over time, particularly the introduction of new expensive drugs in the market. This limitation may lead to an underestimate of any cost savings generated by adherence to CCPs. Ascertainment bias may also prevent accurate comparisons, as the availability of clinical data may differ between patients treated on- and off-pathways, respectively. Virtually no data inform about pathway adherence and its impact on patient outcomes for less common malignancies, although some programs intend to gradually cover additional cancers.14 Finally, no studies have evaluated how CCPs affect other important patient-reported outcomes (PROs), such as quality of life, symptoms, and satisfaction with care.
The oncology community has also voiced concerns about potential detrimental effects of pathway adoption on patient care and clinic workflow. The American Society of Clinical Oncology recently released a statement that outlines some of these concerns.20 Many oncology clinics are experiencing an excessive administrative burden imposed by payers that require frequent reporting of pathway adherence. This burden is particularly disruptive for clinics that have to report adherence to multiple pathways for the same disease because each payer requires the use of its own preferred pathway. Some oncologists and patient advocates worry that the process of pathway development is not as transparent as the leadership of CCPs claim it to be. Other concerns include a possible negative impact of pathway adoption on the patient—physician relationship if adherence forces physicians to significantly narrow treatment options, as well as a detrimental effect on the outcomes of patients treated off-pathways if pre-authorizations or other excessive administrative hurdles prevent timely initiation of therapy.
Future Directions
Physician adherence is critical for the successful implementation of CCPs, which implies that efforts to develop CCPs should include all physicians affected by them. Physicians need to have their voices heard in order to feel comfortable with using pathways in their daily routine.
Ideally, randomized controlled trials would provide more robust evidence on the effectiveness and economic impact of CCPs. In reality, such trials are difficult to conduct and unlikely to ever materialize because many clinics could not agree with randomization to either the intervention (pathway) or control (no pathway) arms. The oncology community will likely have to rely on the synthesis of the evidence generated by observational studies to develop a better understanding of how pathways affect variation in care, costs, and outcomes. Future investigations should focus on risk-adjusted comparisons between practices that participate in pathways versus practices that decide not to do so. Although still imperfect, this type of comparison is probably less subject to selection bias than studies that measure pathway effectiveness based on adherence.
If CCPs are to become a sustainable model of care delivery, the administrative burden of managing them has to be minimal. Payers cannot realistically expect that oncology clinics will be able to report adherence to multiple pathways for the same cancer, and even less so for different cancers, only because payers elect to use a particular pathway of their choice. A much more rational approach is to leave the choice of pathway to the oncology clinics and let the clinics manage 1 pathway for each cancer type.
Finally, the development of CCPs should include more than recommendations for drug regimens, in order to maximize the benefits of pathway use. Pathway recommendations need to cover the entire spectrum of cancer management—from early detection to end-of-life care. In doing so, pathway programs will have to face the challenge of incorporating the applications of precision oncology, including the many recommendations for biomarker-guided use of target therapies.
Although survival and hospitalizations are important metrics, PROs should become an additional outcome measure of pathway effectiveness.
EBO
In summary, preliminary evidence indicates that adherence to CCPs favorably impacts some patient outcomes and direct medical costs. The oncology community has a great opportunity to improve value in cancer care by engaging all stakeholders in transparent processes of pathway development. In order to ensure that pathways become a sustainable model of delivery of high-value cancer care, the administrative burden to oncology clinics needs to be minimal.
Author information:
Bernardo Haddock Lobo Goulart, MD, MS, is a faculty member of the Hutchinson Institute for Cancer Outcomes Research, Fred Hutchinson Cancer Research Center, and an assistant professor at the Division of Medical Oncology, University of Washington.
Address for correspondence:
Bernardo H. L. Goulart, MD, MS
1100 Fairview Avenue N. Seattle
Washington, 98109
E-mail: bgoulart@fredhutch.org
References
- American Society of Clinical Oncology. The state of cancer care in America, 2015: a report by the American Society of Clinical Oncology. J Oncol Pract. 2015;11(2):79-113. doi:10.1200/JOP.2015.003772.
- Hirsch BR, Balu S, Schulman KA. The impact of specialty pharmaceuticals as drivers of health care costs. Health Aff (Millwood). 2014;33(10):1714-1720. doi:10.1377/hlthaff.2014.0558.
- Smith TJ, Hillner BE. Bending the cost curve in cancer care. N Engl J Med. 2011;364(21):2060-2065. doi:10.1056/NEJMsb1013826.
- American Society of Clinical Oncology. Potential approaches to sustainable, long-lasting payment reform in oncology. J Oncol Pract. 2014;10(4):254-258. doi:10.1200/JOP.2014.001267.
- Nadpara P, Madhavan SS, Tworek C. Guideline-concordant timely lung cancer care and prognosis among elderly patients in the United States: a population-based study. Cancer Epidemiol. 2015;39(6):1136-1144. doi:10.1016/j.canep.2015.06.005.
- Bach PB, Cramer LD, Schrag D, Downey RJ, Gelfand SE, Begg CB. The influence of hospital volume on survival after resection for lung cancer. N Engl J Med. 2001;345(3):181-188.
- Clough JD, Patel K, Riley GF, Rajkumar R, Conway PH, Bach PB. Wide variation in payments for Medicare beneficiary oncology services suggests room for practice-level improvement. Health Aff (Millwood). 2015;34(4):601-608. doi:10.1377/hlthaff.2014.0964.
- Abdelsattar ZM, Birkmeyer JD, Wong SL. Variation in Medicare payments for colorectal cancer surgery. J Oncol Pract. 2015;11(5):391-395. doi:10.1200/JOP.2015.004036.
- Zhu J, Sharma DB, Gray SW, Chen AB, Weeks JC, Schrag D. Carboplatin and paclitaxel with vs without bevacizumab in older patients with advanced non-small cell lung cancer. JAMA. 2012;307(15):1593-1601. doi:10.1001/jama.2012.454.
- Feinberg BA, Lang J, Grzegorczyk J, et al. Implementation of cancer clinical care pathways: a successful model of collaboration between payers and providers. Am J Manag Care. 2012;18(5):e194-e199.
- Convergence: advancing every aspect of cancer treatment. Seattle Cancer Care Alliance website. http://www.scca-annual-report-2014.org. Published 2014. Accessed March 15, 2016.
- Dana-Farber pathways. Dana-Farber Cancer Institute website. http://www.dana-farber.org/Adult-Care/Treatment-and-Support/Quality-and-Patient-Safety/Improving-and-Innovating/Clinical-Pathways.aspx. Accessed March 15, 2016.
- Aston G. Exploring cancer care and payment models. Hospital & Health Networks website. http://www.hhnmag.com/articles/3066-health-cares-3-cs-collaboration-coordination-continuum. Published May 12, 2015. Accessed March 15, 2016.
- Ellis PG. Development and implementation of oncology care pathways in an integrated care network: the Via Oncology Pathways experience. J Oncol Pract. 2013;9(3):171-173. doi:10.1200/JOP.2013.001020.
- Hoverman JR, Cartwright TH, Patt DA, et al. Pathways, outcomes, and costs in colon cancer: retrospective evaluations in two distinct databases. J Oncol Pract. 2011;7(suppl 3):52s-59s. doi:10.1200/JOP.2011.000318.
- Kreys ED, Kim TY, Delgado A, Koeller JM. Impact of cancer supportive care pathways compliance on emergency department visits and hospitalizations. J Oncol Pract. 2014;10(3):168-173. doi:10.1200/JOP.2014.001376.
- Neubauer MA, Hoverman JR, Kolodziej M, et al. Cost effectiveness of evidence-based treatment guidelines for the treatment of non-small-cell lung cancer in the community setting. J Oncol Pract. 2010;6(1):12-18. doi:10.1200/JOP.091058.
- Scott JA, Wong W, Olson T, Fortner BV. Year one evaluation of regional pay for quality (P4Q) oncology program. J Clin Oncol. 2010; 28(suppl; abstract 6013):15s.
- Kreys ED, Koeller JM. Documenting the benefits and cost savings of a large multistate cancer pathway program from a payer's perspective. J Oncol Pract. 2013;9(5):e241-e247. doi:10.1200/JOP.2012.000871.
- Zon RT, Frame JN, Neuss MN, et al. American Society of Clinical Oncology policy statement on clinical pathways in oncology. J Oncol Pract. 2016;12(3):261-266. doi:10.1200/JOP.2015.009134.

Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More

