- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Brensocatib Improves Outcomes in Non-Cystic Fibrosis Bronchiectasis With or Without Comorbid COPD
Brensocatib improves lung structure and reduces exacerbations in non-cystic fibrosis bronchiectasis with or without COPD, according to posters presented at this year's CHEST meeting.
Brensocatib (Brinsupri; Insmed) demonstrated significant clinical and structural benefits, including reduced exacerbations, slower lung function decline, and improved CT outcomes, in patients with non-cystic fibrosis bronchiectasis, both with and without comorbid chronic obstructive pulmonary disease (COPD), according to 2 posters presented at the 2025 CHEST annual meeting last month.2,4
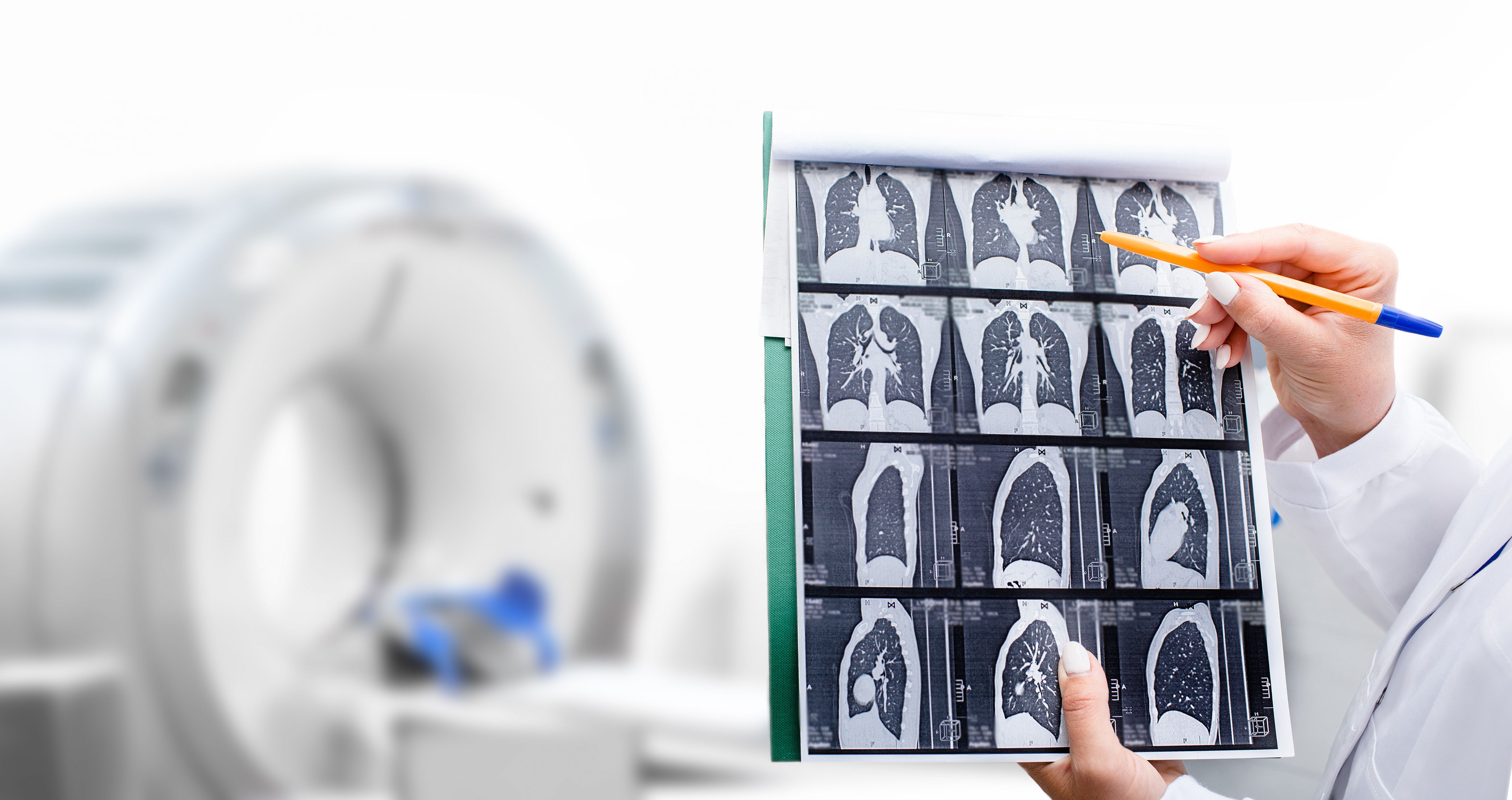
Brensocatib improves lung structure and reduces exacerbations in non-cystic fibrosis bronchiectasis with or without COPD, according to posters presented at this year's CHEST meeting. | Image Credit: Peakstock - stock.adobe.com
Landmark Therapy Improves Outcomes in Non–Cystic Fibrosis Bronchiectasis
Brensocatib, an oral, competitive, and reversible inhibitor of dipeptidyl peptidase 1 (DPP1) that prevents the activation of neutrophil serine proteases, was recently approved by the FDA for non-cystic fibrosis bronchiectasis.1 This approval makes brensocatib both the first approved therapy for this patient population and the first DPP1 inhibitor approved to treat a neutrophil-mediated disease.
The approval was supported by data from the phase 3 ASPEN trial (NCT04594369), which randomized adults and adolescents to receive either a once-daily placebo or brensocatib at 10 mg or 25 mg. The trial found that brensocatib, regardless of dose, significantly reduced the annualized rate of pulmonary exacerbations, prolonged the time to first exacerbation, and increased the odds of remaining exacerbation-free over 52 weeks compared with placebo.2 Additionally, patients who received 25 mg of brensocatib experienced a significant reduction in lung function decline and nominally significant improvements in patient-reported symptoms.
Brensocatib Reduces Structural Lung Changes in Bronchiectasis
Posters presented at the 2025 CHEST annual meeting further explored findings from the ASPEN trial to better understand brensocatib's clinical and structural impact. One analysis assessed its effect on structural lung disease in adult patients using high-resolution CT scans performed at screening and at week 52. The researchers evaluated these scans using the Bronchiectasis Scoring Technique for CT (BEST-CT), a grid-based visual scoring system, and LungQ-BA, an artificial intelligence-based, validated algorithm that automatically segments the bronchial tree and matches arteries to measure bronchus-artery (BA) dimensions and ratios.
The substudy included 100 patients with paired CT scans, of whom 37 received 10 mg of brensocatib, 24 received 25 mg, and 39 received a placebo. Although heterogeneity was observed in both the extent and severity of structural lung changes, the researchers observed that treatment with brensocatib produced measurable improvements.
Compared with placebo, 25 mg of brensocatib significantly reduced the extent of bronchiectasis with mucus plugging (least-squares [LS] mean difference [standard error (SE)], –0.11 [0.04]; P = .0084) and mucus plugging overall (LS mean difference [SE], –0.90 [0.36]; P = .0154). In contrast, it increased healthy lung tissue volume (LS mean difference [SE], 2.10 [0.95]; P = .0298). Similarly, the 10 mg dose reduced bronchiectasis without mucus plugging (LS mean difference [SE], –1.43 [0.72]; P = .0496).
The LungQ-BA analysis showed that fewer BA pairs were detected at week 52 in the 25-mg brensocatib group vs placebo (LS mean difference [SE], –38.35 [19.31]; P = .0499), suggesting improvements in bronchial wall thickness. It also found that the bronchus outer diameter was smaller with the 10-mg dose than with placebo (LS mean difference [SE], –0.15 [0.07]; P = .0339).
The researchers conclude that both doses of brensocatib, but particularly 25 mg, improved several CT end points, indicating that its impact on inflammatory processes may result in structural lung changes.
“Brensocatib is an important new tool for the treatment of bronchiectasis,” James D. Chalmers, MD, PhD, the poster’s lead investigator and presenter, said in an on-site interview with The American Journal of Managed Care® (AJMC).3 “…I think brensocatib will be really important as a treatment to prevent exacerbations and slow down the progression of disease, alongside the other things that we can offer patients, which include airway clearance, which is the critical backbone of management.”
Brensocatib Demonstrates Consistent Clinical Benefits in Patients With, Without COPD
Because many patients with bronchiectasis also have comorbid respiratory diseases such as COPD, another poster examined ASPEN trial outcomes among patients with and without comorbid COPD.4 The analysis, which included 262 patients with COPD and 1459 without, assessed exacerbation rate, time to first exacerbation, remaining exacerbation-free, changes in forced expiratory volume in 1 second (FEV1), and safety.
Both the 10-mg (with COPD: rate ratio [RR], 0.70; 95% CI, 0.44-1.13; without COPD: RR, 0.80; 95% CI, 0.68-0.93) and 25-mg (with COPD: RR, 0.81; 95% CI, 0.56-1.18; without COPD: RR, 0.80; 95% CI, 0.68-0.95) doses of brensocatib reduced exacerbation rates in all patients, regardless of COPD status. It also prolonged the time to first exacerbation in both those with (10-mg dose: HR, 0.67; 95% CI, 0.43-1.06; 25-mg dose: HR, 0.92; 95% CI, 0.62-1.37) and without (10-mg dose: HR, 0.82; 95% CI, 0.69-0.97; 25-mg dose: HR, 0.80; 95% CI, 0.67-0.96) COPD.
Additionally, both doses increased the odds of remaining exacerbation-free among patients with (10-mg dose: OR, 2.21; 95% CI, 1.15-4.26; 25-mg dose: OR, 1.32; 95% CI, 0.70-2.47) and without (10-mg dose: OR, 1.35; 95% CI, 1.04-1.77; 25-mg dose: OR, 1.44; 95% CI, 1.10-1.88) COPD. At week 52, compared with placebo, both doses also reduced the decline in FEV1 in those with (10-mg dose: LS mean difference, 10 mL; 95% CI, -45 to 65; 25-mg dose: LS mean difference, 39 mL; 95% CI, –12 to 90) and without (10-mg dose: LS mean difference, 10 mL; 95% CI, –19 to 39; 25-mg dose: 37 mL; 95% CI, 7-67) COPD.
Lastly, adverse events were consistent with the overall ASPEN study results. However, serious adverse events occurred more often in patients with vs without COPD across treatment arms (10-mg dose: 11.7% vs 8.9%; 25-mg dose: 16.9% vs 9.2%; placebo: 17.6% vs 12.1%).
“These results show that brensocatib improved clinical outcomes in patients with and without COPD, an important observation in a heterogeneous disease like bronchiectasis, where many patients have respiratory comorbidities,” the researchers concluded.
References
- McCormick B. Brensocatib becomes first FDA-approved therapy for bronchiectasis. AJMC. August 12, 2025. Accessed November 7, 2025. https://www.ajmc.com/view/brensocatib-becomes-first-fda-approved-therapy-for-bronchiectasis
- Chalmers JD, Mollica F, Caudri D, et al. Effect of brensocatib on computed tomography outcomes in patients with non-cystic fibrosis bronchiectasis: an analysis of the ASPEN trial. Presented at: CHEST; October 19-22, 2025; Chicago, Illinois. Poster 3708.
- Joszt L, Chalmers JD. Integrating brensocatib and CT scans into NCF bronchiectasis management. AJMC. October 22, 2025. Accessed November 7, 2025. https://www.ajmc.com/view/integrating-brensocatib-and-ct-scans-into-ncf-bronchiectasis-management-james-chalmers-mbchc-phd
- Swenson CE, Chalmers JD, De-Soyza A, et al. Efficacy and safety of brensocatib in patients with noncystic fibrosis bronchiectasis and comorbid COPD: a subgroup analysis of the ASPEN trial. Presented at: CHEST; October 19-22, 2025; Chicago, Illinois. Poster 3708.
