- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
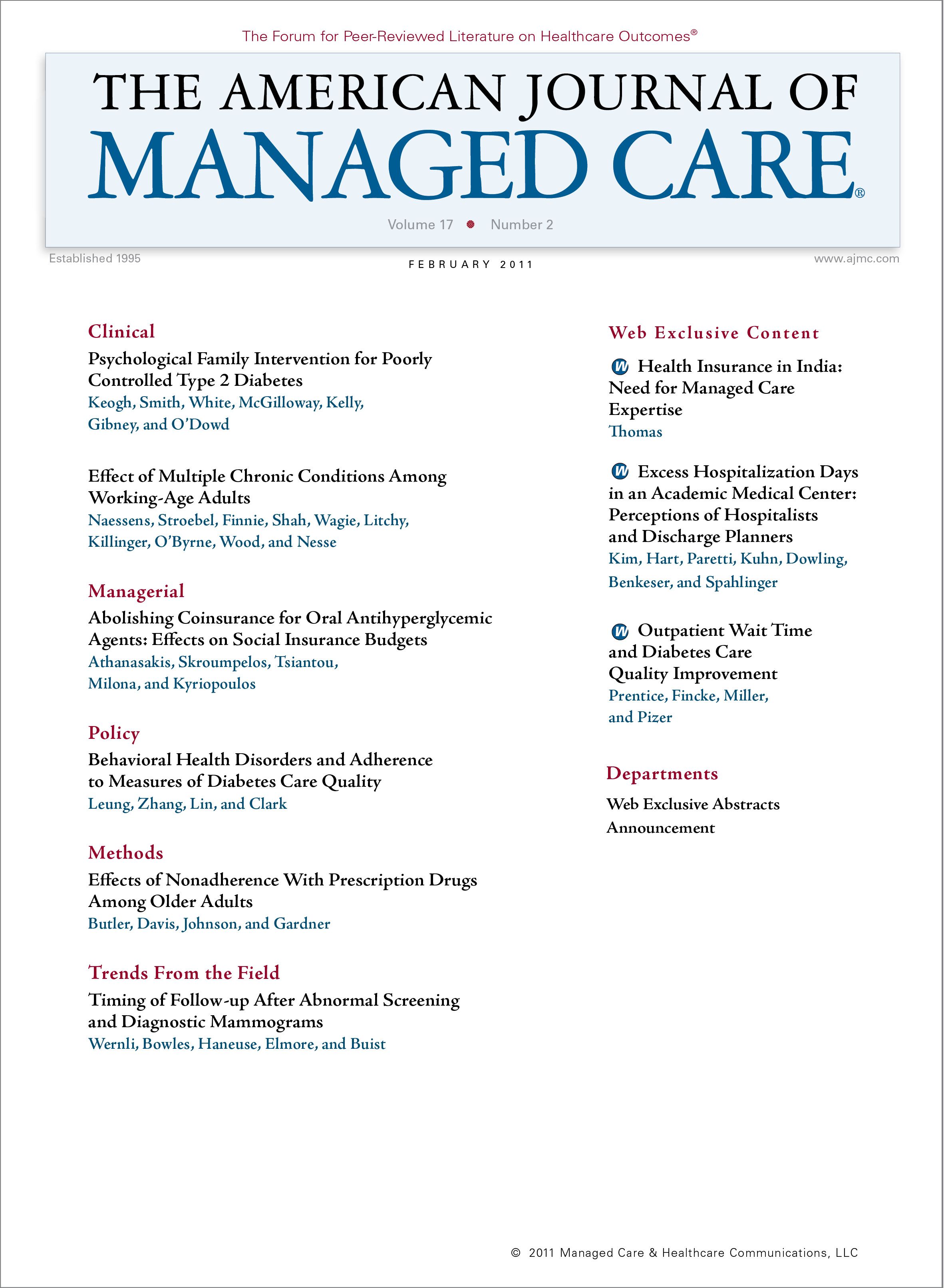
Excess Hospitalization Days in an Academic Medical Center: Perceptions of Hospitalists and Discharge Planners
We assessed the frequency of and reasons for medically unnecessary hospital days, which affect patients, payers, hospitals, and healthcare providers.
Objective:
To determine the frequency of and reasons for medically unnecessary hospital days.
Study Design:
Prospective observational cohort study.
Methods:
We developed an online survey to pro-spectively collect data on hospitalists' and discharge planners' perceived delays in treatment or discharge for patients on their general medicine services. Over a 2-month period, hospitalists and discharge planners completed a daily online survey.
Results:
We collected data on 3574 patient-days from our hospitalists and data on 2502 patient days from our discharge planners. Among the hospitalists'responses, 395 patient-days (11%) were thought to be unnecessary. Among the discharge planners' responses, only 186 patient-days (7%) were thought to be unnecessary. The hospitalists believed that the most common reason for discharge delay was lack of extended care facility availability (111 patient-days [28%]), followed by patient or family reasons (62 patient-days [15%]), procedure delays (62 patient-days [15%]), and test scheduling delays (52 patient-days [13%]). The discharge planners' data were similar.
Conclusions:
More than 10% of hospital days were reported by our hospitalists to be unnecessary at this academic medical center. Major reasons were lack of extended care facility availability, patient or family reasons, procedure delays, and test scheduling delays. A simple survey instrument to assess perceived delays in the hospital may provide real-time information to initiate improvement changes to reduce excess hospitalization days.
(Am J Manag Care. 2011;17(2):e34-e42)
More than 10% of hospital days were reported to be unnecessary at this academic medical center.
- This figure is in alignment with previously reported studies.
- Hospitalists working independently or with house officers reported similar rates of excess hospitalization days.
- Because hospitals are employing more hospitalists, the use of a simple real-time data collection tool to identify the frequency of and reasons for excess hospitalization days may focus improvement efforts in these highly occupied organizations.
Excess hospitalization days are of major concern to patients, payers, hospitals, and healthcare providers. Implications of excessive length of stay include the following: (1) greater costs, (2) potentially increased iatrogenic illness, and (3) high hospital occupancy with resultant loss of efficiency and access. To address these concerns, hospitals have developed support systems that include discharge planning services, home care services, and hospitalist services.
According to the Society of Hospital Medicine,1 the hospitalist field has grown rapidly, with more than 30,000 hospitalists now in practice. At academic medical centers (AMCs) in particular, many programs have expanded to include the following 2 types of hospitalist services: (1) the traditional resident team (RT), where a hospitalist is the supervising attending physician, and (2) a non—house staff hospitalist team (HT), where the hospitalist works independently to provide direct patient care.2 The growth of hospitalist programs in AMCs has been largely attributed to (1) offloading the volume of patients on RTs limited by work hour rules of the Accreditation Council on Graduate Medical Education and (2) filling an overall increasing demand for hospital care services.2-4
Previously, Selker et al5 published a study on the epidemiology of unnecessary hospital days in an AMC. Subsequent studies6-10 have measured and classified excess hospitalization days to assess the potential effect on healthcare systems. These studies found 10% to 20% of hospital days to be unnecessary. To determine the frequency of and most common reasons for delays on the general medicine services at our AMC, we asked our hospitalists and our discharge planners to complete a daily online survey. To our knowledge, this is the first study comparing the views of hospitalists (on RT and HT services) and of discharge planners on excess hospitalization days.
METHODS
Setting
Our hospital is a tertiary care AMC with more than 600 adult beds and 34,000 annual discharges. The 39 hospitalists in our group staff almost 10,000 total discharges. Hospitalists serve as supervising attending physicians on RTs and see patients individually on HTs. Both teams provide hospital coverage 24 hours a day and 7 days a week. Each discharge planner works with 1 to 3 of these RT or HT services.
Survey
Appendix
Using previously validated studies5,6 as guides, we developed a brief (<5 minute) online survey instrument that asked hospitalists and discharge planners whether any of their patients on the general medicine services experienced an excess hospitalization day. They could further categorize the delay as an intrahospital delay (related to an inhospital service not completed in a timely manner) or as a discharge day delay (prevented discharge of a patient who was otherwise medically ready for discharge). To facilitate completion of the voluntary surveys, we generalized the comprehensive categories of delay from previous studies to 4 intrahospital delay choices and 5 discharge day delay choices. The respondents were restricted to a single response choice and could type in more detailed information as free text, or they could select “other” and write in a response. We identified the hospitalists and their respective discharge planners working on the day shift for each day of the survey from a prearranged work schedule and sent daily e-mail messages asking them to independently complete the surveys from August 6 to October 1, 2008. The survey is given in the .
Statistical Analysis
The survey responses were the only data source utilized in analyzing our results. Descriptive statistics were used to assess the frequencies and categories of excess hospitalization days. X2 Analyses were used to assess unadjusted bivariate comparisons between groups of interest with respect to reasons for the excess hospitalization days. Two-tailed a was set at .05. All analyses were performed using commercially available statistical software (STATA/IC 10.0; StataCorp LP, College Station, Texas).
RESULTS
Hospitalists completed 65% of the potential total number of surveys, yielding data on 3574 patient-days, and discharge planners completed 63% of the potential total number of surveys, yielding data on 2502 patient-days. The hospitalists’ data included 1632 patient-days from the RT services and 1942 patient-days from the HT services. Among all hospitalist’ responses, 395 patient-days (11%) were believed to be unnecessary. The RT patients experienced 171 delay days (11%), while the HT patients experienced 224 delay days (12%). Further comparison between weekdays vs weekend days between the RT and HT services revealed no significant differences. Among all discharge planners’ responses, 186 patient-days (7%) were believed to be unnecessary, a statistically significant difference compared with the hospitalists’ responses (P <.01).
Hospitalists’ Data
Table 1
Of 395 excess hospitalization days reported by our hospitalists, 224 (57%) were due to discharge day delays, and 171 (43%) were due to intrahospital delays. The most common reasons for excess hospitalization days were lack of extended care facility availability, patient or family reasons, procedure delays, and test scheduling delays. lists the most commonly selected categories of delay as reported by our hospitalists and our discharge planners.
Discharge Planners’ Data
Of 186 excess hospitalization days reported by our discharge planners, 145 (78%) were due to discharge day delays, and 41 (22%) were due to intrahospital delays. The discharge planners generally agreed with the hospitalists’ categorization of the most common reasons for excess hospitalization days (Table 1).
Specific Categories of Intrahospital Delays
Table 2
As part of a postsurvey analysis of intrahospital delays, 2 hospitalist reviewers (ALH and RFP) manually reviewed each free-text response provided and totaled the number of days attributed to each type of delay (). From the hospitalists’ perspectives, procedure delays accounted for most of the intrahospital delays, followed by consult delays. Among the procedure delays, radiology-related services accounted for more than half of the delay days. The discharge planners provided fewer specific reasons for delays but generally agreed with the hospitalists’ views on intrahospital delays.
DISCUSSION
Hospitalists at our AMC perceived 11% excess hospitalization days, with no significant difference between the RT and HT services. Our discharge planners perceived 7% excess hospitalization days. Both hospitalists and discharge planners identified the following categories of discharge delay to be the most common: (1) lack of extended care facility availability, (2) patient or family reasons, (3) procedure delays, and (4) test scheduling delays.
We note similar rates of excess hospitalization days across study locations and periods relative to previously published studies. Carey et al6 reported a 14% rate of unnecessary hospital days in their general medicine services over 2762 days, while Selker et al5 reported a 17% rate of unnecessary hospital days among general medicine and gastrointestinal patients over 7795 days. More recently, a study7 of hospitalized general pediatric patients identified 9% excess hospitalization days over 911 days.
The hospitalist movement represents a dramatic evolution in healthcare, with 30,000 hospitalists now in practice.1 At most AMCs, where the house staff census remains fixed and the demand for hospital care increases, medicine hospitalist groups have expanded their presence to provide direct patient care.2 Resident teams have maintained the traditional structure of attending, resident, interns, and students. Attending-only hospitalist teams can theoretically run “leaner,” with improvements in efficiencies and work flow. However, our study shows no difference in the number of excess hospitalization days between these 2 types of general medicine services. When the categories of delays were classified as intrahospital delays vs discharge day delays, the rates were again similar between the 2 types of hospitalist services (38% on RTs and 47% on HTs for intrahospital delays vs 62% on RTs and 53% on HTs for discharge day delays). Despite speculation that direct attending—level care by hospitalist teams could run more efficiently and result in fewer excess hospitalization days, further studies are needed to determine how hospitalists’ daily work flow compares with that of house staff–run teams and whether these differences lead to greater efficiencies in patient care services. It may be that the lack of differences observed between the 2 types of hospitalist services in our facility reflects external factors beyond the control of primary hospitalists. As hospitals have engaged discharge planners, home care services, and hospitalists, the next logical approach may be to identify and work with specific hospital services such as stress tests, radiology studies, and gastrointestinal procedures, as well as to employ skilled nursing facilities to establish partnerships to expedite the transition of patients from the acute care facility. Providing real-time feedback to hospital administration and providers regarding specific reasons for excess hospitalization days may drive health system efficiency efforts to these selected areas identified by the hospitalists.
Our analysis also revealed that among the top perceived reasons for excess hospitalization days was patient or family unreadiness. For many patients, the course of a hospital stay can be an intense experience and require ongoing care as they transition out of the acute care setting. Early discharge initiatives can prepare patients and families for the discharge process.11 Patients and their family members need to be engaged and actively involved in the discharge process, identifying needs and facilities even as early as at the time of admission.
Excess hospitalization days raise concerns for patient safety, quality, and efficiency, but also herald significant financial costs to the healthcare system as a whole. Extrapolating our data over a year’s time yields 5500 excess hospitalization days (11% of 10,000 discharges staffed, with a mean length of stay of 5 days). Patients and healthcare practitioners and administrators should certainly appreciate the resultant cost burden. These resources could be better used to provide care to a broader patient population within the community.
Our study also included the perspectives of discharge planners, who work closely with our hospitalists, and found that the discharge planners perceived a lower rate of excess hospitalization days. Closer evaluation of the survey responses revealed that our discharge planners perceived that a greater percentage of delays occurred after patients were believed to be medically ready for discharge than our hospitalists (and vice versa, where the discharge planners thought that fewer delays were attributable to intrahospital delays compared with our hospitalists). Although we can only speculate as to the reasons for these differences in perception, we believe that contributing factors to this observation may include the following: (1) discharge planners, whose specialty is to primarily focus on the needs of patients after (or near the point where) they have been deemed ready for discharge, may have been biased to find more delays in this category, and (2) discharge planners in general do not review all the consultant records, nor do they speak with the diagnostic or therapeutic procedural departments to order tests or obtain results. Therefore, they may not always have had the information to determine if there was an intrahospital delay and could have underestimated this category of delays.
Ongoing quality improvement initiatives to reduce the number of excess hospitalization days are proposed. A simple data collection tool can help identify the most common reasons for excess hospitalization days on a real-time basis, which in turn can be used to deploy countermeasures with appropriate hospital-based specialists and staff. In our organization, we expect to further explore the intrahospital delays as characterized in Table 2. By implicating procedural services with the largest proportion of excess hospitalization days, valuable feedback can be provided to these departments to improve patient flow. Furthermore, although our data did not directly evaluate whether weekend services led to greater rates of excess hospitalization days, the literature suggests that weekend service restrictions may contribute to inappropriate delays and that weekend availability of services should continue to be monitored for perceived delays.10 This type of real-time information regarding specific hospital services may be helpful to hospital administration focusing on efficiency of clinical operations.
There are inherent limitations to our quality improvement survey. First, our data were collected from a single AMC, and the results may not be generalizable. Furthermore, given that our study population included patients admitted to the general medicine services, the results may not be applicable to other clinical services such as pediatrics and surgery. Second, we had less than 100% compliance with completion of the survey. In particular, if there was some sort of systematic lack of response in which some hospitalists may have responded to the survey at a much lower rate than other hospitalists, there may be overrepresentation or underrepresentation biases introduced within the results. Because we collected data on more than 3500 patient-days from our hospitalists and more than 2500 patient-days from our discharge planners, we believe that the data are fairly representative of our AMC during the study period. Third, we identified a difference in the perception of excess hospitalization days between the hospitalists vs the discharge planners. This could be attributed to our survey process in which discharge planners did not complete surveys on weekends, and review of the data showed that some discharge planners reported an unspecified number of multiple delay days. Given the lack of clarity, we input these data points as a single delay day, which may have underestimated some of the discharge planners’ perceptions. Fourth, weekend days may be times of reduced efficiency, with at least 1 study10 noting resultant excess hospitalization days on weekends, and there are likely other forces (such as staffing and hours of operation) that can lead to excess hospitalization days for a hospital. Fifth, given that our survey allowed for respondents to select only a single response, it is unclear how respondents may have dealt with competing reasons for a discharge delay, which in turn may have affected some of our categorization of results. Furthermore, because the primary intent of our evaluation was to determine the frequency of delay, we did not ask our discharge planners or our hospitalists to include patient-specific information, and we were unable to perform any sort of interrater comparative statistical analysis.
In conclusion, more than 10% of hospital days on the general medicine services were found to be unnecessary at our AMC. A simple-to-use data collection survey can help staff recognize excessive hospitalization days in real time and quickly identify the reasons for delay. Hospitalists could work cooperatively with discharge planners to gather data prospectively and report their findings on causes of delay. This may be relevant to hospitalist groups, who care for an increasing proportion of inpatients. Moreover, such data should be of interest to hospital administrators, as well as to payers of this nation’s increasingly costly inpatient care.
Acknowledgments
We thank all of the hospitalists and discharge planners who took the time to help us evaluate this issue in our health system by completing the daily online surveys. Their expertise and professional contribution to our ongoing efforts at improvement are much appreciated.
Author Affiliations: From the Department of Internal Medicine (CSK, ALH, RFP, LK, DAS), University of Michigan, Ann Arbor, MI; and the Department of Practice Management and Discharge Planning (AED, JLB), University of Michigan Health System, Ann Arbor, MI.
Funding Source: The authors report no external funding for this study.
Author Disclosures: The authors (CSK, ALH, RFP, LK, AED, JLB, DAS) report no relationship or financial interest with any entity that would pose a conflict of interest with the subject matter of this article.
Authorship Information: Concept and design (CSK, ALH, AED, JLB, DAS); acquisition of data (CSK, ALH, AED, JLB); analysis and interpretation of data (CSK, ALH, RFP, LK); drafting of the manuscript (CSK, RFP, LK); critical revision of the manuscript for important intellectual content (CSK, ALH, RFP, DAS); statistical analysis (ALH, LK); administrative, technical, or logistic support (AED, JLB); and supervision (CSK, DAS).
Address correspondence to: Christopher S. Kim, MD, MBA, Department of Internal Medicine, University of Michigan, 3119 Taubman Ctr, Box 5376, Ann Arbor, MI 48109-5376. E-mail: seoungk@umich.edu.
1. Society of Hospital Medicine. About SHM. http://www.hospitalmedicine.org/AM/Template.cfm?Section=About_SHM. Accessed 2010.
2. Sehgal NL, Shah HM, Parekh VI, Roy CL, Williams MV. Non-house staff medicine services in academic centers: models and challenges. J Hosp Med. 2008;3(3):247-255.
3. Saint S, Flanders SA. Hospitalists in teaching hospitals: opportunities but not without danger. J Gen Intern Med. 2004;19(4):392-393.
4. Fletcher KE, Underwood W III, Davis SQ, Mangrulkar RS, McMahon LF Jr, Saint S. Effects of work hour reduction on residents' lives: a systematic review. JAMA. 2005;294(9):1088-1100.
5. Selker HP, Beshansky JR, Pauker SG, Kassirer JP. The epidemiology of delays in a teaching hospital: the development and use of a tool that detects unnecessary hospital days [published correction appears in Med Care. 1989;27(8):841]. Med Care. 1989;27(2):112-129.
6. Carey MR, Sheth H, Braithwaite RS. A prospective study of reasons for prolonged hospitalizations on a general medicine teaching service. J Gen Intern Med. 2005;20(2):108-115.
7. Srivastava R, Stone BL, Patel R, et al. Delays in discharge in a tertiary care pediatric hospital. J Hosp Med. 2009;4(8):481-485.
8. Minichiello TM, Auerbach AD, Wachter RM. Caregiver perceptions of the reasons for delayed hospital discharge. Eff Clin Pract. 2001;4(6): 250-255.
9. Brasel KJ, Rasmussen J, Cauley C, Weigelt JA. Reasons for delayed discharge of trauma patients. J Surg Res. 2002;107(2):223-226.
10. Varnava AM, Sedgwick JE, Deaner A, Ranjadayalan K, Timmis AD. Restricted weekend service inappropriately delays discharge after acute myocardial infarction. Heart. 2002;87(3):216-219.
11. Manning DM, Tammel KJ, Blegen RN, et al. In-room display of day and time patient is anticipated to leave hospital: a "discharge appointment". J Hosp Med. 2007;2(1):13-16.
Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More
Building Trust: Public Priorities for Health Care AI Labeling
January 27th 2026A Michigan-based deliberative study found strong public support for patient-informed artificial intelligence (AI) labeling in health care, emphasizing transparency, privacy, equity, and safety to build trust.
Read More
Ambient AI Tool Adoption in US Hospitals and Associated Factors
January 27th 2026Nearly two-thirds of hospitals using Epic have adopted ambient artificial intelligence (AI), with higher uptake among larger, not-for-profit hospitals and those with higher workload and stronger financial performance.
Read More
Motivating and Enabling Factors Supporting Targeted Improvements to Hospital-SNF Transitions
January 26th 2026Skilled nursing facilities (SNFs) with a high volume of referred patients with Alzheimer disease and related dementias may work harder to manage care transitions with less availability of resources that enable high-quality handoffs.
Read More

