- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
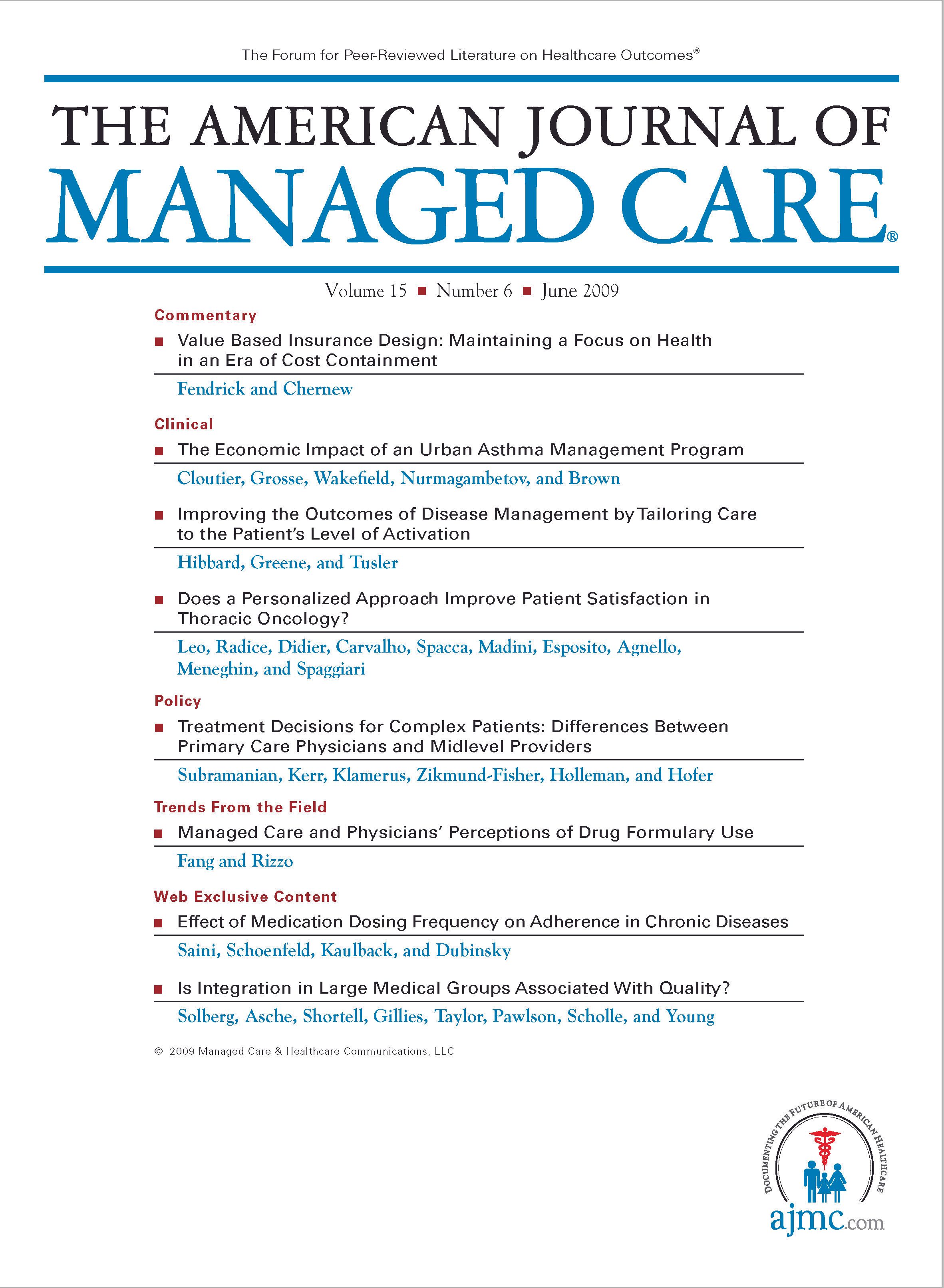
Managed Care and Physicians' Perceptions of Drug Formulary Use
This article examines the changing effects of managed care on prescription drug formulary use in the United States.
Objectives:
To investigate the effects of managed care on drug formulary use and to determine whether these effects have changed over time.
Study Design:
We use longitudinal data from the Community Tracking Study physician surveys and compare the effects of managed care on drug formulary use between 2000-2001 and 2004-2005.
Methods:
Ordinary least squares regression models are estimated to quantify the effects of managed care on drug formulary use. Data from 2000-2001 and 2004-2005 are pooled together, and the year trend effect is represented by a dummy variable for 2004-2005.
Results:
We find that the coefficient measuring the effects of managed care on drug formulary use declined from 0.37 (P <.01) in 2000-2001 to 0.27 (P <.01) in 2004-2005. However, this relative decline in the effects of managed care on formulary use reflects not an absolute decline in formulary use in managed care but an increase in formulary use in the nonmanaged care sector. For the typical physician who has a mix of managed care and nonmanaged care patients, drug formulary use increased over time.
Conclusions:
Differences in drug formulary use between managed care and nonmanaged care declined from 2000-2001 to 2004-2005. The overall level of drug formulary use increased, reflecting an increase in the nonmanaged care sector.
(Am J Manag Care. 2009;15(6):395-400)
Some observers have argued that managed care has relaxed restrictive practices designed to control costs in light of public backlash.
- We find that the effects of managed care on drug formulary use weakened from 2000-2001 to 2004-2005.
- However, nonmanaged care increased formulary use during this period, and the absolute level of formulary use under managed care remained virtually unchanged. Managed care and nonmanaged care were converging in formulary use over this period.
- These results are consistent whether we study capitated managed care, noncapitated managed care, or managed care as a whole.
Despite the rapid growth of managed care during the past 2 decades, its restrictive practices have drawn increasing criticism from physicians and their patients.1-3 In response to growing concerns about such restrictions, the role of managed care in constraining healthcare services is believed to have declined in recent years.3-5
If managed care has become less restrictive, this could have important implications for patient access and patterns of care. Yet, there is little quantitative evidence on these issues. Using a national physician sample,6 we found that the restrictions on the provision of physician services declined in managed care between 2000-2001 and 2004-2005. The present study seeks to provide further evidence on the evolving role of managed care with respect to the use of drug formularies. A drug formulary is a list of prescription medications covered under a health insurance plan. Many formularies have several copayment tiers, with the lowest copayments for “preferred drugs,” which are often generics or less costly brand-name drugs.7 This article investigates whether the association between physician involvement in managed care and prevalence of prescription formulary use among their patients has declined over time.
METHODS
Data
The present study uses data from the Community Tracking Study (CTS) physician surveys for 2000-2001 and 2004-2005, maintained at the Center for Studying Health System Change. The CTS physician surveys achieve response rates of about 60% and comprise a nationally representative sample of physicians in the United States. A review of the CTS database concluded that “there was little evidence of a systematic underrepresentation among demographic and practice characteristics available for all physicians from the AMA [American Medical Association] Masterfile.”8(ppC.19-C.20) The surveys include approximately 12,000 physicians in 2000-2001 and 6000 physicians in 2004-2005. The 2004-2005 CTS sample survey was 50% as large as the survey in 2000-2001, which accounts for the smaller size of our 2004-2005 sample. However, the sampling method was the same in both surveys.
Physicians in the CTS surveys engaged in direct patient care for at least 20 hours/week in 60 randomly selected communities in the United States, and the survey questionnaires include information on managed care revenue, medical care management, and various other physician and practice characteristics. After excluding approximately 9% of subjects who did not respond to the prescription formulary, managed care, and key control variables, our study sample includes 11,940 physicians in 2000-2001 and 5463 physicians in 2004-2005.
Variables
Prescription Formulary. To gauge the extent of physicians whose patients use prescription formularies, the CTS survey asked each physician the following question: “What percentage of your patients have prescription coverage that includes the use of a formulary?” Physician responses ranged from 0% to 100%.
Managed Care. Managed care involvement for physicians is measured as the percentage of their practice revenues from managed care organizations. More specifically, the CTS survey asked each physician: “What percentage, if any, of the patient care revenue received by the practice in which you work comes from all managed care combined?”
The share of revenue from managed care is correlated with the number of managed care patients. That is, a physician with a higher share of revenue from managed care has more patients in managed care than does a physician who has a lower share of revenue from managed care, other things being equal. Managed care is further disaggregated into the share of revenue from capitated managed care and noncapitated managed care, which we also examine separately.
Many managed care organizations offer point-of-service options so that patients may choose the provider and treatment style of their choice, albeit at higher cost. Although in 2004 only 16% of employees had a choice of conventional indemnity plans, 30% also had a point-of-service option.9 Therefore, there is substantial opportunity to go out of network for more traditional types of coverage. Indeed, Strunk and Reschovsky10 report that managed care revenues accounted for slightly less than half of physician practice revenues in 2001. In our sample, managed care revenues accounted for 46% of physician revenues in 2000-2001 and 44% in 2004-2005. Nevertheless, these revenue measures may underestimate the actual number of patients in managed care plans because reimbursement is typically lower in managed care.
Table 1
Other Explanatory Variables. We also control for several physician and practice characteristics that may be correlated with the percentage of patients whose prescription drug coverage includes formulary use. These variables are listed in .
Estimation Models
We first estimate separate prescription formulary equations for 2000-2001 and 2004-2005. This may be written as: Yt = βt,0 + βt,1Mt + βt,2Xt + εt, where Y indicates the percentage of patients who have formulary prescription coverage; M, the percentage of practice revenue from managed care; X, a vector of other explanatory variables; ε, a disturbance term; t, the time subscript for 2000-2001 or 2004-2005; and β0 and β2, the coefficients to be estimated. We estimate the equation using ordinary least squares regression because the dependent variable is a continuous measure from 0 to 100. We then compare the coefficients measuring the effects of managed care on drug formulary use in 2000-2001 versus 2004-2005 to examine whether the relationship between managed care and formulary coverage has changed over time.
To provide a direct estimate of year trend effects on formulary coverage between 2000-2001 and 2004-2005, we next pool these data, including a dummy variable for 2004-2005 and the interaction of this year dummy variable with the managed care variable. Therefore, the pooled multivariate regression model is as follows: Y = Θ0 + Θ1M + Θ2D + Θ3MXD + Θ4X + ε, where D indicates a dummy variable for 2004-2005; MXD, an interaction term between managed care and the year dummy; and Θ0 and Θ4, the coefficients to be estimated.
RESULTS
Table 1 gives descriptive statistics for each wave of the CTS physician surveys. From 2000-2001 to 2004-2005, we find that the percentage of patients having prescription coverage that includes the use of a formulary rose modestly from 60% to 64%. From 2000-2001 to 2004-2005, the percentage of revenue from managed care declined slightly from 46% to 44%.
Table 2
first summarizes the ordinary least squares regression results estimating data from 2000-2001 and 2004-2005 separately. The coefficients measuring the effects of managed care on drug formulary use are 0.37 in 2000-2001 and 0.27 in 2004-2005. Therefore, a 1% increase in managed care revenue will lead to a 0.37% increase in prescription formulary use among patients in 2000-2001 but only a 0.27% increase in 2004-2005. Therefore, the elasticity has been reduced by more than one-fourth from 2000-2001 to 2004-2005.
Table 2 also summarizes the ordinary least squares regression results when we pool the data from 2000-2001 and 2004-2005. We have included a dummy variable for 2004-2005 and its interaction term with the managed care variable. The coefficient of managed care is 0.37, and the coefficient of the interaction term is −0.09. Both estimates are statistically significant at the level of 1%. This robust test supports our hypothesis that the effects of managed care on the percentage of patients with formulary coverage declined over time. The effects of capitated managed care and noncapitated managed care on formulary coverage may differ, as prescription formulary coverage is believed to be more common among capitated managed care plans.11 Therefore, we also break managed care into 2 parts, capitated managed care and noncapitated managed care. Turning to separate estimates for each wave of data, we find that the coefficient of capitated managed care is 0.44 and the coefficient of noncapitated managed care is 0.32 in 2000-2001. Both coefficients (capitated managed care, 0.30; and noncapitated managed care, 0.25) decline in 2004-2005 compared with the earlier period. All these coefficients are statistically significant at the level of 1%. Because of space limitations, the full results are not presented herein but are available from the authors on request.
Has formulary coverage declined in managed care? Thus far, the results have shown that formulary coverage has declined in managed care relative to nonmanaged care. But what has happened to the absolute level of formulary use? To help answer this question, we use the estimated results in Table 2 to generate predicted values for formulary coverage in 2000-2001 and 2004-2005. When physician involvement in managed care is 100%, the mean predicted percentage of formulary coverage is virtually unchanged between 2000-2001 and 2004-2005. This indicates that the absolute level of formulary coverage did not change for managed care over this period. In contrast, when there is no managed care involvement, the mean predicted percentage of formulary coverage increases substantially from 43% in 2000-2001 to 52% in 2004-2005. Because most physicians have a mix of managed care and nonmanaged care patients, overall formulary coverage increased over time. Therefore, for physicians who receive 50% of their revenues from managed care, the mean percentage of prescription formulary coverage increased from 62% to 66%.
DISCUSSION
Some observers have argued that, in response to backlash from providers and patients, managed care has relaxed restrictive practices intended to control costs.3-5 This study has examined this issue in the context of prescription drug formulary use. We find that, while the effects of managed care on formulary coverage declined relative to that of nonmanaged care, the absolute level of formulary coverage in managed care did not change. Given the widespread presence of formulary use in managed care, the stability of formulary coverage over time may represent a ceiling effect. In contrast, formulary coverage became more common among nonmanaged care plans in 2004-2005 than in 2000-2001. This finding suggests that managed care and nonmanaged care plans are becoming more similar in terms of formulary coverage. Because of this convergence, changes in the mix of indemnity versus managed care plans may have little effect on the extent of prescription drug formulary use in the future. Given consumer and provider backlash against managed care, many plans are relaxing restrictions and allowing beneficiaries to go out of network.12 But others have observed that indemnity plans are assuming more features that were typical of managed care plans, including greater use of formularies:
Over time, the distinction between HMOs [health maintenance organizations] and indemnity plans has become increasingly blurred, says Larry Levitt, vice president at the Kaiser Family Foundation. “Traditional plans have introduced utilization measures that were historically found only in managed care plans,” he says…. Another familiar HMO-style feature found in traditional plans is the drug formulary—the list of medicines that a plan will pay for. When Blue Cross/ Blue Shield of New Jersey sent out its list to policymakers last year, it included a letter recommending they speak with their physicians about finding substitutions for prescriptions that weren’t on the formulary.13
Some investigators have questioned the success of drug formulary use as a cost-control measure, arguing that physicians contract with multiple plans and that these plans have very different formulary lists.14 In a review of health plans in California, Shrank et al note great heterogeneity in formulary lists:
None of the branded drugs evaluated were preferred on all formularies in 2002, and 10% were not available on any of the formularies. Formulary status varied greatly across plans, and more than 60% of drugs were preferred on 2 to 4 of the 6 formularies studied. Formulary status within health plans varied between 2000 and 2002 in more than half of the plans in the drug classes evaluated.15(p401) Moreover, formulary use may have adverse consequences for consumers. Huskamp et al7 found that, while the use of more restrictive formularies constrained spending for several drug classes, it also shifted the burden of costs onto consumers. These researchers also found that different types of formulary changes could have substantially different effects on drug utilization and costs and that changes in copayment structures have far-reaching consequences for compliance, patient costs, and possibly quality of care. Prescription formularies are an increasingly common feature of health insurance plans. Investigations to obtain more evidence on the implications of these changes for cost, access, and quality of care are important directions for further research.
Author Affiliations: Health Economics Research Group (HF), University of Miami, Coral Gables, FL; and Department of Economics (JAR) and Department of Preventive Medicine (JAR), Stony Brook University, Stony Brook, NY. Dr Fang is now with the Department of Health Systems, Management and Policy, University of Colorado Denver, Aurora.
Funding Source: None reported.
Author Disclosure: The authors (HF, JAR) report no relationship or financial interest with any entity that would pose a conflict of interest with the subject matter of this article.
Authorship Information: Concept and design (HF, JAR); acquisition of data (HF, JAR); analysis and interpretation of data (HF, JAR); drafting of the manuscript (HF, JAR); critical revision of the manuscript for important intellectual content (HF, JAR); statistical analysis (HF, JAR); provision of study materials or patients (HF, JAR); administrative, technical, or logistic support (HF, JAR); and supervision (HF, JAR).
Address correspondence to: Hai Fang, PhD, MPH, Department of Health Systems, Management and Policy, University of Colorado Denver, 13001 E 17th Ave, 3rd Fl, Campus Box B119, Aurora, CO 80045. E-mail:fanghaimail@gmail.com.
1. Blendon RJ, Brodie M, Benson JM, et al. Understanding the managed care backlash. Health Aff (Millwood). 1998;17(4):80-94.
2. Enthoven AC, Singer SJ. The managed care backlash and the task force in California. Health Aff (Millwood). 1998;17(4):95-110.
3. Robinson JC. The end of managed care. JAMA. 2001;285(20):2622-2628.
4. Draper DA, Hurley RE, Lesser CS, Strunk BC. The changing face of managed care. Health Aff (Millwood). 2002;21(1):11-23.
5. Shen YC, Melnick G. Is managed care still an effective cost containment device? Forum Health Econ Policy. 2006;9(1):e1007. Frontiers in Health Policy Research article 3. http://www.bepress.com/fhep/9/1/3. Accessed May 15, 2009.
6. Fang H, Rizzo JA. The changing effect of managed care on physician financial incentives. Am J Manag Care. 2008;14(10):653-660.
7. Huskamp HA, Deverka PA, Epstein AM, Epstein RS, McGuigan KA, Frank RG. The effect of incentive-based formularies on prescriptiondrug utilization and spending. N Engl J Med. 2003;349(23):2224-2232.
8. Center for Studying Health System Change. Community Tracking Study: Physician Survey Methodology Report: 2000-01 (Round Three). Washington, DC: Center for Studying Health System Change; May 2003:C.19-C.20. Appendices to Technical Publication No. 38. http://www.hschange.org/CONTENT/570/570a.pdf. Accessed August 30, 2008.
9. Health Research & Educational Trust (HRET) Web site. HRET and The Kaiser Family Foundation: 2004 Employer Health Benefits Annual Survey. http://www.hret.org/hret/publications/2004ehbs.html. Accessed September 14, 2008.
10. Strunk BC, Reschovsky JD. Kinder and gentler: physicians and managed care, 1997-2001. Center for Studying Health System Change Tracking Report: results from the Community Tracking Study No. 5. November 2002. http://www.hschange.com/CONTENT/486/486.pdf. Accessed September 14, 2008.
11. Lyles A, Palumbo FB. The effect of managed care on prescription drug costs and benefits. Pharmacoeconomics. 1999;15(2):129-140.
12. Cooper PF, Simon KI, Vistnes J. A closer look at the managed care backlash. Med Care. 2006;44(5)(suppl):I4-I11.
13. www.badfaithinsurance.org Web site. Ten things your health insurer won’t tell you. http://www.badfaithinsurance.org/reference/HL/0015a.htm. Accessed January 21, 2009.
14. Mays GP, Hurley RE, Grossman JM. Consumers face higher costs as health plans seek to control drug spending. Center for Studying Health System Change Issue Brief: findings from HSC No. 45. November 2001. http://www.hschange.org/CONTENT/389/389.pdf. Accessed September 14, 2008.
15. Shrank WH, Ettner SL, Glassman P, Asch SM. A bitter pill: formulary variability and the challenge to prescribing physicians. J Am Board Fam Pract. 2004;17(6):401-407.
Building Trust: Public Priorities for Health Care AI Labeling
January 27th 2026A Michigan-based deliberative study found strong public support for patient-informed artificial intelligence (AI) labeling in health care, emphasizing transparency, privacy, equity, and safety to build trust.
Read More
Ambient AI Tool Adoption in US Hospitals and Associated Factors
January 27th 2026Nearly two-thirds of hospitals using Epic have adopted ambient artificial intelligence (AI), with higher uptake among larger, not-for-profit hospitals and those with higher workload and stronger financial performance.
Read More
Motivating and Enabling Factors Supporting Targeted Improvements to Hospital-SNF Transitions
January 26th 2026Skilled nursing facilities (SNFs) with a high volume of referred patients with Alzheimer disease and related dementias may work harder to manage care transitions with less availability of resources that enable high-quality handoffs.
Read More
Specialty and Operator Status Influence Electronic Health Record Use Variation
January 22nd 2026Operators demonstrated specialty-specific differences in electronic health record efficiency, timeliness, and after-hours use, highlighting how workflow and training shape documentation behaviors across medical disciplines.
Read More

