
- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
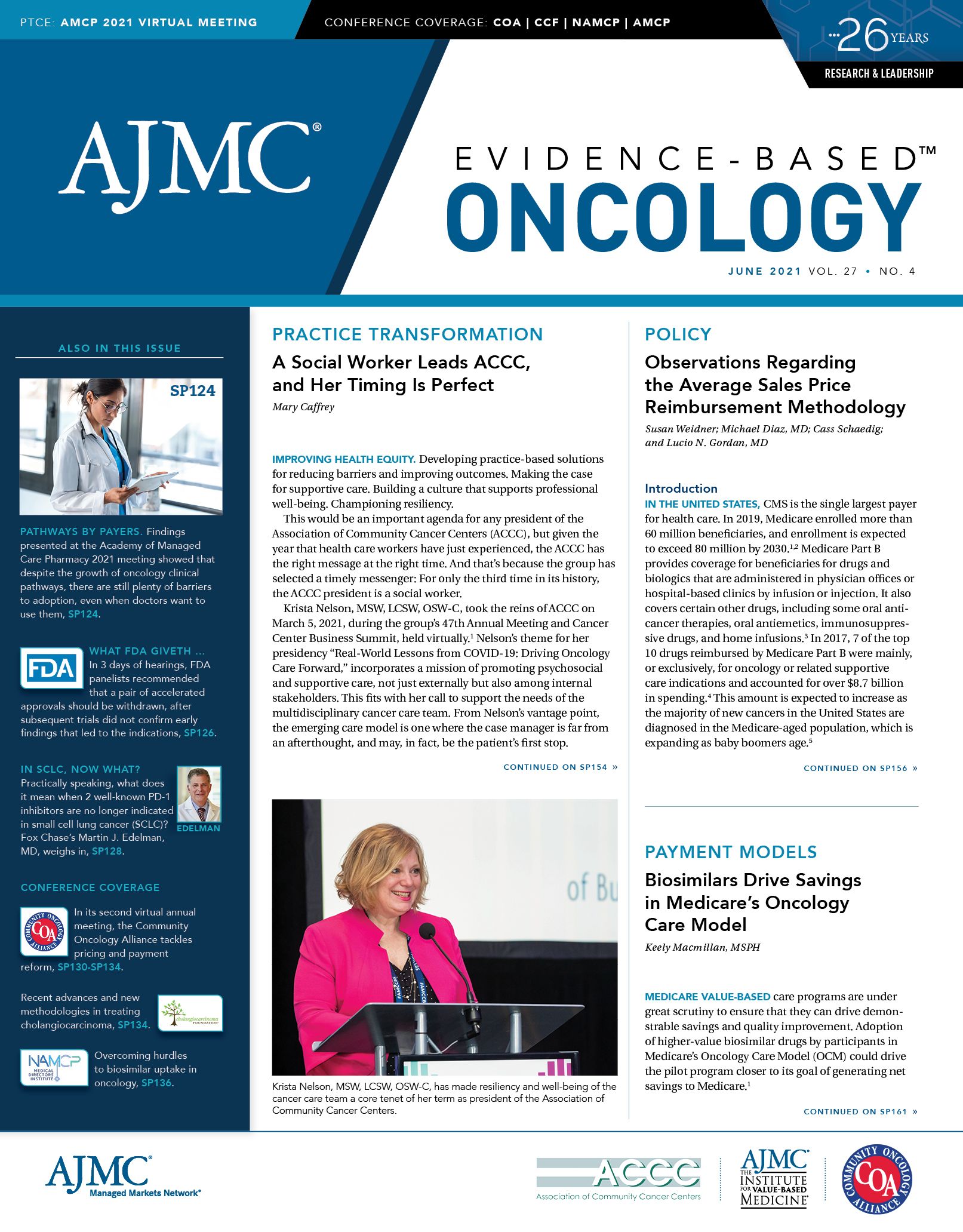
A Social Worker Leads ACCC, and Her Timing Is Perfect
Improving health equity. Developing practice-based solutions for reducing barriers and improving outcomes. Making the case for supportive care. Building a culture that supports professional well-being. Championing resiliency.
This would be an important agenda for any president of the Association of Community Cancer Centers (ACCC), but given the year that health care workers have just experienced, the ACCC has the right message at the right time. And that's because the group has selected a timely messenger: For only the third time in its history, the ACCC president is a social worker.
Krista Nelson, MSW, LCSW, OSW-C, took the reins of ACCC on March 5, 2021, during the group's 47thAnnual Meeting and Cancer Center Business Summit, held virtually.1 Nelson's theme for her presidency "Real-World Lessons from COVID-19: Driving Oncology Care Forward," incorporates a mission of promoting psychosocial and supportive care, not just externally but also among internal stakeholders. This fits with her call to support the needs of the multidisciplinary cancer care team. From Nelson's vantage point, the emerging care model is one where the case manager is far from an afterthought, and may, in fact, be the patient's first stop.
Nelson spoke with Evidence-Based Oncology™ (EBO) about her goals as ACCC president and why her timing couldn’t be better. This interview is edited for clarity.
EBO: Your year as ACCC president comes at a time of unprecedented stress on the health care system due to the pandemic. Why is this the right time for a person with a social work background to lead the organization?
NELSON: As clinical social workers, we’re trained in systems, we’re collaborators, and we’re really good listeners. Right now, the suffering is so great within our community—meaning our community of providers, the people who are taking care of patients with cancer. Our workforce needs attention, and a social work perspective brings this to light. Our values as social workers teach us the dignity of the human person: to challenge injustice, and to be present with the people we work with and those we serve. I think the role of the social worker is perfect to lead ACCC at this time.
EBO: One of the agenda items you listed is working on resiliency in the cancer care workforce. Can you discuss specifically you how you want to address the issue of resiliency?
NELSON: First, I will say that resiliency is multifaceted. It’s the role of the person, and the organization, and the community. Often, we put the burden on the person [when] people are not coping well [or] are having a hard time. And I’d be remiss if I didn’t say it’s OK to be having a hard time right now. This work is really hard: It was hard before COVID-19, and it’s even harder now. People are being pulled in so many [different] ways.
At ACCC, we’re working to, first, listen to the experts—the people who are living it. [We’re] reaching out to our various communities, and hearing best practices of what people are doing: how they’re helping support their team, the changes they’re making, and how they’re addressing [issues]. One way we’re doing that is by offering coffee chats: I’m having these virtual smaller group meetings to hear how ACCC can improve the care of the provider, and therefore improve the care of the patient.
Second, we’re creating a meditation series for people within the ACCC community, and that’s something I’m passionate about. Just even taking a mindful pause can really help with resilience in our teams.
What are the other things? We’re creating business case studies to show the value of supportive care for our patients. The truth is, if we provide avenues for more supportive care for our patients and remove barriers on the provider side, then the providers will not have such a heavy burden, because a team of people is supporting the patients.
EBO: Obviously, the pandemic has affected cancer care in countless ways. What are some specific challenges you’re hearing about today that you weren’t hearing about a year ago?
NELSON: First, the staffing shortages. There have been furloughs all through this experience, and the workforce has been through [a lot] of stress. It’s hard to find new people to replace those who have left because of stress and burnout.
What we hear the most now are concerns about screening delays and the impact this will have—we’re anticipating that patients may be diagnosed with more advanced cancer.
There’s also the financial landscape, and [the need for] mitigating the losses that the health care system experienced during [a period] of not having surgeries [and other procedures]. I think we are gaining ground, but that’s going to take time. And [the financial losses] have this downstream effect of supportive services being cut or limited. For patients, it’s probably one of the most challenging times they’ve ever experienced.
Another exciting but challenging opportunity has been telemedicine. Here, we are talking on video instead of face to face, and I think that’s the new world of how we’re working with our patients—and looking at the reimbursement issues of telehealth is really important. It’s especially important when we think about how we’re supporting our more rural communities, and making sure we’re removing barriers [to ensure] that everyone has access to quality cancer care. I think I’ve said this before, but it’s about really listening to the membership: People are doing creative things out there, and we want to hear what we can learn from them.
EBO: Let’s follow up on your point about the delays in screening. Almost from the very beginning of the pandemic, experts predicted this—and that these delays would lead to downstream delays in cancer diagnoses. Does ACCC have any specific initiatives that they’ll work on this year on this issue?
NELSON: One of our greatest strengths is that we do work within our communities, including something unique ACCC has called Innovator Awards. In the past 3 years, we’ve heard from many innovative programs around cancer screening, including ways to address health equity and injustices in cancer treatment and care. [From there], we solicit learnings from within the community and invite our members to hear those—through podcasts, through meetings, through publications. It’s really a way to share the best practices in the community. Our past president published an article in USA Today about the ways to stress the importance of cancer screening in the lung cancer population—and not to stop because of COVID-19.2 Number 1, however, is the responsibility to just get the word out to patients in our community that screening is safe, and that it’s important. I think that is the best place to start.
EBO: You also mentioned the health equity issue, which has been an ongoing theme at ACCC even before the pandemic. Would you like to discuss progress in this area, or plans for things that you’d like to do over the next year?
NELSON: Number 1, for ACCC and providers—I hope— the community is changing how we look in the lens that we see through. We need to be looking for opportunities for inclusion, We need to be educating ourselves. ACCC has an amazing collaboration going right now with the American Society of Clinical Oncology, and we’re looking at implicit bias training and a research assessment tool, both of which are designed to address barriers to patients participating in clinical trials, specifically for Black and Latino patients.3 We’re really looking at ways we can collaborate in innovative ways to work with our communities to improve access to clinical care for these patients.
EBO: Will this initiative produce data that you’ll report on, maybe in 2 years?
NELSON: Absolutely.
EBO: So, to conclude, how you see the role of the social worker in the cancer care team evolving, say, over the next 3 to 5 years?
NELSON: The role of the oncology social worker has always been central, but maybe not the most visible out in the community. But some amazing innovative models are happening right now.
Both the University of Washington and the University of Texas at Austin have programs—I believe the Austin program is called CaLM—that are reinventing how we look at cancer care. They recognize that the person as a whole is the central reason why we’re here.4 It’s why we’re providing
cancer care, and the programs make sure that that person has wraparound services, and the social worker is more central in that role.
It’s really looking at, “How does this person access care? Do they have any barriers? How are they coping? Are they interested in fertility?” It’s looking at all these things, plus—can they pay their rent? All these things are important in cancer care, and but sometimes they aren’t as visible.
EBO: Are ongoing studies showing how this approach will affect patient outcomes compared with the more traditional approach?
NELSON: Absolutely. A lot of work is being done on the research side. Unfortunately, there’s not as much funding for that research. But yes, it is being done in in smaller groups.
I think one of the barriers to this model of care is the soft money to fund supportive care for patients. You know, the dietitians, the physical therapists, speech therapists: We know they—and social workers—are essential to be able to support a patient through cancer treatment, and they don’t necessarily charge for their services. So, we’re looking at how we can demonstrate the value of this, because this will also help support our patients in the long run.
References
1. Association of Community Cancer Centers names new president, Krista Nelson, MSW, LCSW, OSW-C, FAOSW. News release. Association of Community Cancer Centers; March 5, 2021. Accessed May 10, 2021. https://www.accc-cancer.org/home/news-media/press-releases/
news-template/2021/03/05/association-of-community-cancer-centersnames-new-president-krista-nelson-msw-lcsw-osw-c-faosw
2. Oyer RA. Don’t skip your lung cancer screenings during COVID-19. Future of Personal Health. USA Today (insert). November 11, 2020. Accessed May 11, 2021. https://www.futureofpersonalhealth.com/lunghealth/
dont-skip-your-lung-cancer-screenings-during-covid-19/
3. Unger JM, Hershman DL, Till C, et al. “When offered to participate”: a systematic review and meta-analysis of patient agreement to participate in cancer clinical trials. J Natl Cancer Inst. 2021;113(3):244-257. doi:10.1093/jnci/djaa155
4. CaLM care team. The University of Texas at Austin: UT Health Austin. Accessed May 10, 2021. https://uthealthaustin.org/clinics/cancer/calm-care-team
Exploring Racial, Ethnic Disparities in Cancer Care Prior Authorization Decisions
October 24th 2024On this episode of Managed Care Cast, we're talking with the author of a study published in the October 2024 issue of The American Journal of Managed Care® that explored prior authorization decisions in cancer care by race and ethnicity for commercially insured patients.
Listen
Exploring Racial, Ethnic Disparities in Cancer Care Prior Authorization Decisions
October 24th 2024On this episode of Managed Care Cast, we're talking with the author of a study published in the October 2024 issue of The American Journal of Managed Care® that explored prior authorization decisions in cancer care by race and ethnicity for commercially insured patients.
Listen
2 Commerce Drive
Cranbury, NJ 08512
AJMC®
All rights reserved.
