- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
6-Year Data Support Fixed-Duration Ven-Obi for Untreated CLL
Long-term data support the safety and efficacy of venetoclax (Venclexta) and obinutuzumab (Gazyva) in chronic lymphocytic leukemia (CLL), though questions remain about which patients would benefit most from the regimen.
Patients with previously untreated chronic lymphocytic leukemia (CLL) and coexisting conditions who underwent 1-year fixed-duration therapy with venetoclax (Venclexta) and obinutuzumab (Gazyva) had encouraging rates of overall (OS) and progression-free survival (PFS) at 6 years, according to new data.1
The new report, published in the Blood, offers longer-term follow-up data from the phase 3 CLL14 trial, which was originally published in 2019.
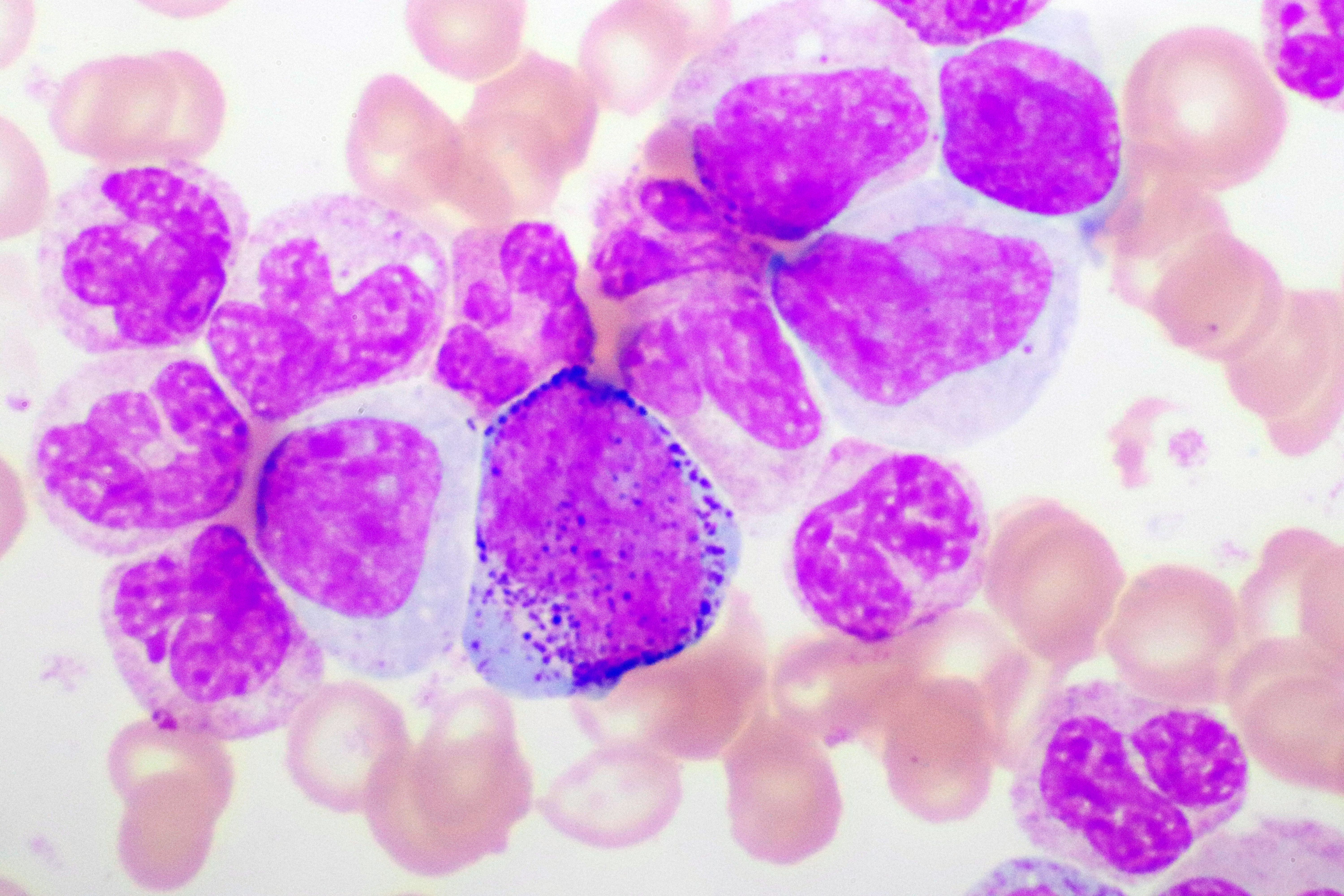
CLL cells magnified/stained | image credit: jarun011 - stock.adobe.com
Venetoclax is a BCL-2 inhibitor, and obinutuzumab is a CD20 antibody. The combination of the 2 therapies has been shown to lead to rapid remission and high rates of undetectable minimal residual disease (MRD) in patients with previously treated and untreated CLL, explained corresponding author Othman Al-Sawaf, MD, of the University of Cologne, in Germany, and colleagues.
“This approach provides the opportunity to discontinue treatment while maintaining treatment-free remissions of several years in many patients,” they wrote.
Yet, Al-Sawaf and colleagues added that the heterogeneity of CLL means outcomes after fixed-duration treatment may also vary over time. Thus, they said, careful study of the duration of remission following fixed-duration therapy is warranted.
The open-label CLL14 study compared fixed-duration venetoclax-obinutuzumab (Ven-Obi) with chemoimmunotherapy with chlorambucil (Leukeran) plus obinutuzumab (Clb-Obi).2 That study included 432 patients with previously untreated CLL and clinically relevant coexisting conditions who were split into 2 equal cohorts and underwent a dozen 28-day cycles of therapy. After a median follow-up of 28.1 months, patients in the Ven-Obi group had superior PFS compared to those in the Clb-Obi group. In addition, 76% of patients in the Ven-Obi group had undetectable MRD levels of <10−4, compared to just 35% of patients in the Clb-Obi group.
The new report updates those data with results at a median of 76.4 months. Al-Sawaf and colleagues found that Ven-Obi’s PFS advantage continued, with a median PFS of 76.2 months in the Ven-Obi group, compared to 36.4 months in the Clb-Obi group (HR, 0.40; 95% CI, 0.31-0.52; P < .0001). Similarly, the 6-year time-to-next-treatment (TTNT) was longer in the Ven-Obi group (65.2% vs 37.1%; HR, 0.44; 95% CI, 0.33-0.58; P < .0001).
“With all patients being off study treatment for >5 years, this, to the best of our knowledge, longest follow-up data confirms sustained remissions in >50% of patients treated with Ven-Obi with no additional toxicity reported,” the investigators wrote.
Among patients in the Ven-Obi arm of the trial, the investigators said the presence of del(17p), unmutated immunoglobulin heavy-chain variable region, and lymph node size of ≥5 cm were associated with shorter PFS, the authors reported.
In terms of overall survival, 78.7% of patients in the Ven-Obi arm were alive at 6 years, compared to 69.2% of patients in the Clb-Obi arm (HR, 0.69; 95% CI, 0.48-1.01; P = .052). The investigators also found that participants who received Ven-Obi had a significantly longer time until definitive deterioration in global health status and quality of life.
Al-Sawaf and colleagues said these new data confirm the long-term safety and efficacy of fixed-duration Ven-Obi in this patient group, as well as the efficacy of fixed-duration targeted therapy in general in patients with previously untreated CLL. However, they said a number of open questions remain, including which patients are best suited for fixed-duration Veb-Obi therapy, and which would do better on fixed-duration venetoclax plus ibrutinib (Imbruvica) or continuous Bruton tyrosine kinase inhibitors. They said a number of ongoing studies should help clarify that question and others.
In the meantime, they said these new data offer confirmation that fixed-duration Ven-Obi is a useful tool in CLL.
References:
- Al-Sawaf O, Robrecht S, Zhang C, et al. Venetoclax-obinutuzumab for previously untreated chronic lymphocytic leukemia: 6-year results of the randomized phase 3 CLL14 study. Blood. 2024;144(18):1924-1935. doi:10.1182/blood.2024024631
- Fischer K, Al-Sawaf O, Bahlo J, et al. Venetoclax and Obinutuzumab in Patients with CLL and Coexisting Conditions. N Engl J Med. 2019;380(23):2225-2236. doi:10.1056/NEJMoa1815281
