- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
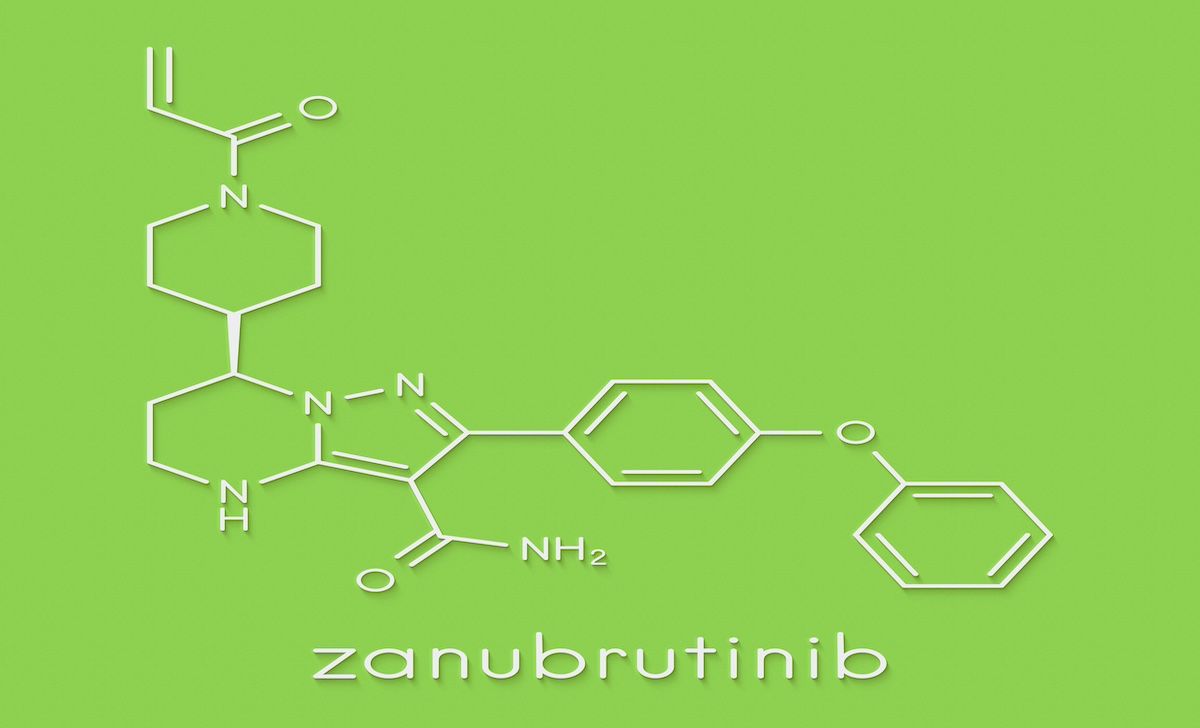
Zanubrutinib Safer Than Ibrutinib in Patients With B-Cell Malignancies
A post-hoc analysis showed that zanubrutinib resulted in fewer adverse events compared with ibrutinib.
An analysis of a large clinical trial safety database found that zanubrutinib 160 mg taken twice dailyled to fewer off-target effects compared with ibrutinib 420 mg taken once daily, according to a study in Haematologica.1
Researchers also corroborated a previous pooled safety analysis that found that zanubrutinib monotherapy was generally well tolerate and associated with significantly lower rates of cardiovascular toxicities, including atrial fibrillation/flutter and hypertension compared with ibrutinib.
“The first-in-class [Bruton tyrosine kinase inhibitor] ibrutinib has drastically improved treatment of numerous B-cell malignancies, but cardiac arrhythmias and their associated outcomes are a frequently cited concern and are possibly due to off-target inhibition of kinases such as TEC and CSK,” the authors wrote. “Such toxicities can limit the duration and, consequently, the benefit of treatment.”
Treatment-emergnt adverse events led to fewer deaths in patients who received zanubrutinib vs ibrutinib, and there was 1 patient death related to zanubrutinib vs 7 related to ibrutinib | Image Credit: molekuul.be-stock.adobe.com
Researchers combined updated data from 6 clinical trials with 779 subjects with 4 additional studies, for a total of 1550 subjects, to further evaluate the effects of zanubrutinib. They also used 2 of these 10 studies to analyze the safety profiles of 425 patients who underwent zanubrutinib therapy compared with 422 patients receiving ibrutinib.
For the zanubrutinib-only analysis, patients had a median age of 66.2 years, and roughly two-thirds were male. Most patients had chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) (60.5%), and approximately two-thirds had relapsed/refractory disease (68.9%). Nearly half (45%) of patients received zanubrutinib for 36 months or longer, with a median of 34.4 months. Slightly more than half (56.5%) of patients remained on zanubrutinib as of the data cutoff.
In the analysis comparing zanubrutinib with ibrutinib, median treatment duration was 32.6 months vs 25.7 months, respectively. More patients were on zanubrutinib vs ibrutinib treatment for 36 months or longer (29.4% vs 25.4%). Zanubrutinib-treated patients were also more likely to still be on treatment at data cutoff than those treated with ibrutinib (69.9% vs 45.0%).
Treatment-emergent adverse events (TEAEs) recorded as treatment related were reported in 79.4% of patients. TEAEs leading to treatment discontinuation were reported in 13.6% of patients in the total pooled zanubrutinib population. In the comparative analysis, TEAEs leading to treatment discontinuation were less common with zanubrutinib vs ibrutinib (14.1% vs 22.0%). Infections were the most common complication that led to treatment discontinuation in both the pooled zanubrutinib (4.5%) and the comparative analysis populations (zanubrutinib, 5.4%; ibrutinib, 6.6%). In the comparative analysis, ibrutinib-treated patients were more likely than zanubrutinib-treated patients to experience cardiac disorder that resulted in discontinuation (4.3% vs 0.5%).
Across all 10 trials, no zanubrutinib-treated patients discontinued due to hypertension.
Deaths attributed to TEAEs occurred in 7.3% of patients in the pooled zanubrutinib population and 8.7% and 10.2% of patients treated with zanubrutinib and ibrutinib, respectively, in the comparative analysis. Cardiac disorder TEAEs leading to death occurred in 7 patients treated with ibrutinib vs 1 patient treated with zanubrutinib.
Zanubrutinib was first approved by the FDA in 2019.2 Low treatment discontinuation rates and long-term tolerability are key considerations, especially in patients with B-cell malignancies such as CLL/SLL who are older than 65 years and have other comorbidities, according to the study.
“In this analysis, zanubrutinib remained well tolerated, consistent with the previous analysis, with no emergence of new safety signals, even at a median treatment duration of approximately 3 years,” the authors wrote. “In the comparative analysis, zanubrutinib exhibited a more favorable safety profile than ibrutinib, as demonstrated by the longer median treatment duration and lower frequency of TEAEs, including cardiac disorders, that led to treatment discontinuation or death. These analyses support zanubrutinib as an appropriate long-term treatment option for patients with B-cell malignancies.”
References
1. Brown J, Ghia P, Jurczak W, et al. Characterization of zanubrutinib safety and tolerability profile and comparison with ibrutinib safety profile in patients with B-cell malignancies: post-hoc analysis of a large clinical trial safety database. Haematologica. 2024;109(7):2277-2283 doi:10.3324/haematol.2023.283846
2. Brukinsa FDA approval history. Drugs.com. Accessed July 10, 2024. https://www.drugs.com/history/brukinsa.html
