- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Walkability and Redlining: How Built Environments Impact Health and Perpetuate Disparities
Built environments can shape how active an individual is, while policy decisions made decades ago impact health disparities today. To address these critical social determinants of health, experts are calling for increased cooperation between urban planners and the public health field.
In the world of real estate, location is everything, serving as a major driving force behind both rent prices and mortgage rates.
But a growing body of research highlights that when it comes to health outcomes, location may also affect disease risk, and where you reside can impact how you live.
It’s no secret that exposure to air and water pollution leads to poor health outcomes, nor would it come as a surprise that proximity to health services can enhance or worsen the quality and quantity of care individuals receive.
However, taking a more granular approach, new studies analyzing effects of geographic-specific features underscore the contribution of built environments and housing policies to health disparities seen throughout the United States.
Although this newly focused attention is making its way into the mainstream—with increasing numbers of partnerships formed between city planners and public health experts—the consequences of systems enacted decades ago are becoming apparent today, and preventive measures enacted tomorrow may do little to resolve past harms.
Walkability as a Social Determinant of Health
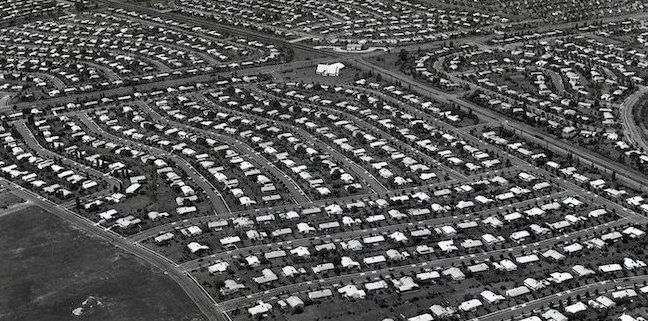
Starting in the 1950s, urban design practices in North America led to the development of “car-oriented, suburban areas, characterized by low population density (urban sprawl), the separation of residential developments from retail, commercial, and business areas, and street designs that lack pedestrian infrastructure,” wrote authors in a recently published review.1
As such, these postwar built environments (eg, Levittown, Pennsylvania, or New York) made walking and biking potentially dangerous and impractical primary forms of transportation. According to researchers, these decisions eventually yielded downstream health effects, as exhibited by metabolic health assessments of those living in highly walkable areas compared with individuals residing in areas with low walkability.
Walkability was defined as “the extent to which a neighborhood encourages and supports walking as a means of transportation.” For example, residents in suburban regions may not have amenities within walking distance of their homes and may have to drive to visit the grocery store or pharmacist.
Taken together, data showed that on average, “individuals who live in highly walkable neighborhoods have increased levels of physical activity and lower body weights than those living in less walkable areas.”
In other words, dense, walkable urban layouts were associated with improved metabolic health compared with regions that were less walkable and more car-oriented, researchers concluded, suggesting policies aimed at increasing walkability could lead to tangible health benefits.
Levittown, Pennsylvania
One analysis included in the review revealed that between 2001 and 2012 in Ontario, Canada, higher neighborhood walkability was associated with a stable prevalence of overweight and obesity, and decreasing diabetes incidence. By 2012, all 3 rates were significantly lower compared with less walkable areas, where levels of obesity continued to rise.2
But geographic and population density alone does not account for this association, as destinations also influence the advantages of neighborhood walkability, explained Gillian Booth, MD, MSc, of the Department of Medicine at University of Toronto in an interview with The American Journal of Managed Care® (AJMC®).
Booth is a scientist at the MAP Centre for Urban Health Solutions within the Li Ka Shing Knowledge Institute of St. Michael’s Hospital in Toronto, and coauthor of the aforementioned studies.
Factors outside of design, density, and destinations affect neighborhood-specific health outcomes, and can even negate the benefits of living in highly walkable areas, she stressed.
Based on their research, Booth and colleagues found those living in areas with low levels of traffic-related air pollution reaped greater benefits from walkability with regard to hypertension and diabetes risk.
“But if there [were] really high concentrations of air pollution, the benefit of walkability was completely eliminated, because air pollution itself is a risk factor for diabetes,” she said. “It’s not enough to just build [environments] right.”
Apart from pollution, additional influences can sway the extent to which individuals take advantage of walkability and the neighborhood’s capacity to enact environment-level improvements. Safety, sidewalk conditions, crime rate, and transportation options all function to encourage or dissuade walking, regardless of a space’s design.
“We always have to think about where people live and the neighborhood environment as a whole, and what makes the neighborhood healthy and what doesn’t,” Booth said. “There’s a lot of interest now into, not only how do we make healthier designs, but about how do we make more equitable decisions in terms of where to invest.”
Redlining and Housing Discrimination
More than 40% of the American population is currently obese and more than 37 million Americans already have diabetes. Not only are these crises self-perpetuating—obesity is a key risk factor for diabetes—but stark racial and economic disparities exist within these figures.
The prevalence of diabetes has substantially increased over the past 2 decades in the United States, and the risk of receiving a diabetes diagnosis is 77% higher for African Americans and 66% higher for Hispanics compared with White Americans.
Higher percentages of poverty have also been associated with higher obesity rates, resulting from factors like low individual income and food insecurity.
Despite evidence showing structural racism—including discriminatory housing practices enacted throughout the 20th century—has yielded undue influence on diabetes disparities, a paucity of studies exists examining discrimination’s shaping of resource distribution and opportunities across neighborhoods and the resulting impact on cardiovascular health, authors wrote in PNAS.3
Redlining was a practice that became institutionalized by the federal Home Owners’ Loan Corporation (HOLC) security maps created in the 1930s, wrote Mahasin Mujahid PhD, MS, FAHA, an associate professor of epidemiology at UC Berkeley School of Public Health, and colleagues.
Areas were color coded based on high concentrations of Black, immigrant, and working-class residents and subsequently deemed “hazardous and excessively risky for investment.”
The grades prevented residents in these “undesirable” neighborhoods, especially Black residents, from accessing mortgage financing and home ownership, leading to years of systematic disinvestment, and contributing to inequities in the quality of the physical and social environments in which historically marginalized populations reside in greater proportions, researchers explained.
As a result, these predominantly Black neighborhoods were more susceptible to negative impacts of programs like urban renewal and deindustrialization, leading to low prevalence of home ownership, uneven economic development, displacement of residents, community disintegration, and lack of access to education and economic opportunities.
Using data from the Multi-Ethnic Study of Atherosclerosis, Mujahid and colleagues assessed modern-day cardiovascular health of residents living in historically redlined neighborhoods, and compared findings with those residing in non-redlined, wealthier areas.
A total of 4779 participants from 6 sites across the United States were included in the analysis. Of these, 26.7% were Black, 23.9% were Hispanic, 13.3% were Chinese, and 35.1% were White; 18.9% of participants lived in historically redlined/hazardous areas (based on HOLC grades), 44.2% lived in declining neighborhoods, and 36.9% lived in so-called "desirable" neighborhoods.
Although cardiovascular health (CVH) scores were not consistently lowest in historically redlined neighborhoods, researchers found:
- A higher proportion of Black (22.9%), Hispanic (23.8%), and Chinese (26.0%) participants lived in historically redlined areas, compared with White participants (10.4%)
- Ideal CVH and CVH behaviors were highest in Chinese and lowest in Black and Hispanic participants
- The Ideal CVH factors summary score was highest in White and lowest in Black participants
- The lowest social environment scores were among Black (mean = 1.02) and Hispanic (mean = 0.68) participants residing in historically redlined areas
- The best social environments were among Chinese (mean = 1.11) and White participants (mean = 1.25) residing in historically “A: best” neighborhoods
- HOLC grades were associated with all 3 CVH summary measures: overall CVH, health factors, and health behaviors, as well as with 2 individual indicators of CVH (blood pressure and body mass index), among Black participants, with no association for Hispanic, Chinese, or White participants
“This research found an association between living in a historically redlined neighborhood and present-day CVH for Black residents only,” Mujahid said in an email to AJMC®.
Black Americans currently have the highest cardiovascular disease mortality rate in the country compared with any other racial/ethnic group. Living in a historically redlined area could expose residents to more stressors, which can biologically manifest as cortisol, increasing body mass index. Cumulative stress exposure can also lead to physiological wear and tear (ie, weathering) leading to hypertension.
With regard to walkability, Mujahid noted that due to disinvestment in redlined neighborhoods, “you can expect fewer sidewalks, fewer parks, and fewer places for people to safely play, exercise, and gather.”
“We also know that majority-minority communities are surveilled and stopped by police more often than majority White neighborhoods, so this may be another way in which racial residential segregation keeps people living in redlined areas from safely spending time and getting exercise outside,” she said.
Planning Plus Public Health
The findings outlined in these investigations emphasize a fact that many in the urban planning field have been championing for years—improving social determinants of health cannot be achieved in a silo.
Striking the ideal neighborhood health balance is challenging and may require monetary investments, along with local and federal government intervention. But being aware of the counter force of gentrification is crucial, Mujahid stressed, noting intentional investments are needed to ensure new resources and opportunities are available for long-term and socially vulnerable residents.
In November 2021, the US Senate passed the bipartisan Infrastructure Investment and Jobs Act (IIJA), a $1 trillion bill aimed at rebuilding the nation’s roads, funding new climate resilience initiatives, and addressing, in part, past decisions that contribute to present-day health disparities.
“For the transportation world, I kind of feel like this is huge, because we’ve been talking about equity without really always doing equity for a long time,” said Leigh Ann Von Hagen, AICP, PP, a planning practitioner, managing director and adjunct professor with the Alan M. Voorhees Transportation Center, and a founder of the Planning Healthy Communities Initiative at the Edward J. Bloustein School of Planning and Public Policy at Rutgers University.
One facet of the IIJA includes a census tract mapping element, where planners looking to receive a Rebuilding American Infrastructure with Sustainability and Equity (RAISE) grant would highlight areas of persistent poverty and historically disadvantaged communities.
By providing the mapping tool to identify these areas, the US Department of Transportation (DOT) and Federal Highway Administration are helping to set the tone for future investments, Von Hagen explained in an interview with AJMC®.
Often, planning decisions are made outside of public health, but inherently address those issues. Transportation improvement is one example, she said, because, “that's a public health goal, even if it's not stated as a public health goal. Because if you are walking or bicycling, you're by definition doing something that's active transportation, and that tends to have healthier outcomes, if it's safe.”

Despite the potential of the IIJA serving as a “game changer,” numerous hurdles exist to implementing improvements at the local level, not least of which is the time it takes to make these meaningful changes and overcoming bureaucratic systems separating states from counties from municipalities.
Even if the best applications receive federal funds, local municipalities may not have the manpower to oversee the project’s implementation from beginning to end, while underserved communities may not have the staffing or capacity to apply for grants in the first place.
On the flip side, wealthier communities are better resourced, and could hire a staffer to write grants or even outsource the task to consultants.
Oversight capacity, resident buy-in, expendable resources, and time are thus all necessary for successful implementation, Von Hagen noted.
Citing the example of improving safety along school routes, Von Hagen explained that despite a comprehensive public engagement process, the years between introduction and implementation can prove burdensome, as parents who may contribute to the process initially may see their children graduate and move on before a project is ever finished.
Improving efficiency, creating a steady funding stream, incorporating public health officials in decisions, and ensuring a point-person for projects in underserved communities could all help expedite interventions in built environments, and improve health outcomes along the way, she said.
Looking Long-Term
Like many other fields, the COVID-19 pandemic has taken a toll on partnerships forged between planning experts and public health, as the latter has been stretched thin to deal with the ongoing public health emergency.
Prioritizing addressing social determinants of health remains top of mind for Von Hagen, who questioned if the country has learned its lesson that better funding and staffing for public health is needed.
“If anything, COVID-19 also showed us the cracks became bigger for lack of housing issues, transportation issues, all of that became a wider gap,” she said. “As planners, we really need our public health partners to help drive home the importance of this topic.”
The occasional direct integration of health data into decision making is taking place through the use of CDC Health Impact Assessments or initiatives like Health in All Policies, whereby both the economic and humanistic toll of proposed legislation or projects can be included in the conversation.
But weighing initiatives’ health consequences is not required for professionals outside of the health field, Von Hagen said, adding the DOT is just now getting around to including equity in its decision-making process.
Addressing diabetes and obesity once they manifest is important, but if the floodgates keep opening upstream, patient-by-patient interventions can only do so much with regard to long-term disease prevention, explained Booth.
“We have to tackle it at all stages. [Diabetes] is one of the biggest drivers of health care costs in every country,” she said. Changing the built environment and implementing policy takes time, “but I think we have to make those changes because what we’ve been doing is perpetuating the problem.”
References
1. Howell NA, Booth GL. The weight of place: built environment correlates of obesity and diabetes. Endocr Rev. Published online February 24, 2022. doi:10.1210/endrev/bnac005
2. Creatore MI, Glazier RH, Moineddin R, et al. Association of neighborhood walkability with change in overweight, obesity, and diabetes. JAMA. 2016;315(20):2211-2220. doi:10.1001/jama.2016.5898
3. Mujahid MS, Gao X, Tabb LP, and Lewis TT. Historical redlining and cardiovascular health: the multi-ethnic study of atherosclerosis. Proc Natl Acad Sci USA. Published online December 13, 2021. doi:10.1073/pnas.2110986118
