- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
US Continues to Have Worse Health Outcomes Than Comparable Countries
Even though the US spent far more on healthcare in 2013 than other comparable high-income countries, it has the lowest life expectancy and some of the worst health outcomes, according to a study by The Commonwealth Fund.
Even though the US spent far more on healthcare in 2013 than other comparable high-income countries, it has the lowest life expectancy and some of the worst health outcomes, according to a study by The Commonwealth Fund.
Researchers David Squires, MA, and Chloe Anderson, MSW, used health data from the Organization for Economic Cooperation and Development and other sources to asses US healthcare system spending, supply, utilization, and prices, and healthcare outcomes relative to other countries: Australia, Canada, Denmark, France, Germany, Japan, Netherlands, New Zealand, Norway, Sweden, Switzerland, and the United Kingdom.
The US spent an average of $9086 per person annually with a life expectancy of 78.8 years, while the next highest-spending country, Switzerland, only spent $6325 per person with a life expectancy of 82.9 years. While America had one of the lowest mortality rates for cancer, its rates of chronic conditions, obesity, and infant mortality were higher than other high-income countries.
“Time and again, we see evidence that the amount of money we spend on health care in this country is not gaining us comparable health benefits,” Commonwealth Fund President David Blumenthal, MD, said in a statement. “We have to look at the root causes of this disconnect and invest our health care dollars in ways that will allow us to live longer while enjoying better health and greater productivity.”
According to the data, part of the reason why the US has such higher healthcare spending is because prices for healthcare a “notably higher” in comparison to the other countries analyzed. For instance, the average price of a bypass surgery was more than $30,000 higher than in the second-highest country, Australia ($75,245 vs $42,130).
Public and Private Spending
While a lot of attention is paid to the high out-of-pocket costs facing consumers in the US, the average $1074 spent on healthcare for things like copayments, prescription drugs, and deductibles came second to the $1630 spent by the average Swiss resident. However, for other private spending, such as private insurance premiums, the US spent far more: $3442 per capita compared with $654 in Canada, the second-highest spending country.
Although the other countries studied all had universal healthcare and the US was the only country that did not, public spending in the US was still third highest. In 2013, public spending amounted to $4197 per capita in the US compared with $4981 in Norway and $4495 in the Netherlands. Only a third of US residents were covered by public spending in 2013, meanwhile the United Kingdom covered every resident and spent only $2802 per capita.
Poor Population Health
A 2014 study found that 68% of US adults age 65 years or older had at least 2 chronic conditions, but the rate was significantly lower in the other countries analyzed, ranging from 33% in the United Kingdom to 56% in Canada. The US had the highest rate of obesity at 35.3% with New Zealand second at 30.6% and Japan having the lowest rate with 3.7%. The median for the countries studied was 28.3%.
One thing the authors considered was that heavy tobacco use in the US in the 1960s and 1970s may still be contributing to relatively worse health outcomes among older US adults even though the US had one of the lowest smoking rates in 2013. The large number of uninsured also potentially contributed to the United States performing so much poorly on determinants of health.
Social Services
Compared with the other countries, the US spent a small amount of social services, such as retirement and disability benefits, employment programs, and supportive housing. In the US, these services account for just 9% of gross domestic product, while France, Sweden, Switzerland, and Germany devoted roughly twice as large a share of their economy to social services.
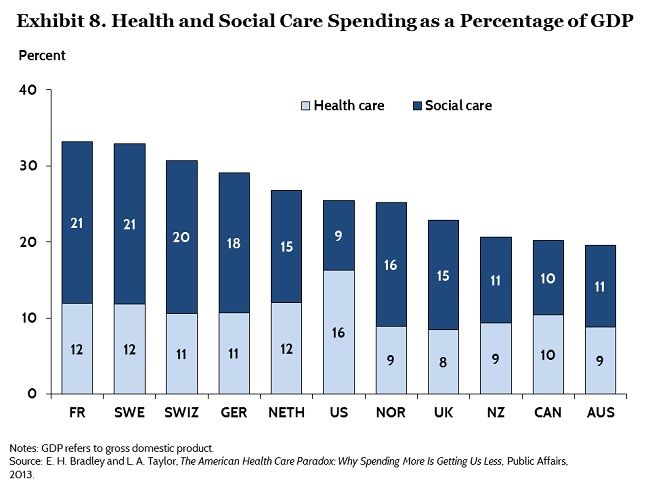
According to the researchers, the imbalance between spending on social services and healthcare spending may contribute to poor health outcomes as evidence suggests social services play an important role in “shaping health trajectories and mitigating health disparities.”
The emergence of new care models that reward providers for value-based care could create a case for health providers to invest in social services or other nonclinical interventions, according to the report.
“Over the long term, such a strategy could potentially alter the current balance between health and social services spending,” the authors concluded.
