- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Updates in Treatment of Adults With Chronic Cough
Abstract
Chronic cough is a severely debilitating condition that results in individuals coughing hundreds to thousands of times per day. Unfortunately, at the time of this writing, the majority of treatments currently available address acute cough and have minimal efficacy for chronic cough. There are no current FDA-approved pharmacologic treatments for chronic cough, resulting in a large, unmet need for patients. Recent advancements in the understanding of the chronic cough reflex and suspected neurobiology have led to the development of novel therapeutic targets to bridge this unmet treatment need. Current American College of Chest Physicians and European guidelines recommend a thorough workup but differ in individual pharmacologic treatment recommendations. All patients should be evaluated for red-flag symptoms and any underlying conditions that may explain the patient’s chronic cough. Historical treatments, such as opiates and neuromodulators, have been used with limited success. Emerging agents that target specific channel receptors have shown initial positive benefits concerning cough frequency, severity, and quality of life and may become available on the market as they have shown to be generally well tolerated without any safety concerns in clinical studies.
Am J Manag Care. 2020;26:S239-S245. https://doi.org/10.37765/ajmc.2020.88515
Introduction
Chronic cough is a severely debilitating condition that can result from multiple different etiologies. Historically, most treatments available to patients have been effective for the resolution of acute cough. Patients can purchase antitussives without a prescription and self-treat when needed. If self-treatment with over-the-counter therapy fails, patients may seek prescription medications for acute cough from their primary care physician, such as benzonatate or cough syrups with codeine.
However, patients whose cough persists beyond 8 weeks (refractory chronic cough [RCC] or unexplained chronic cough [UCC]) experience great irritation as they often cough in excess of hundreds to thousands of times daily.1 Pharmacologic treatment for chronic cough has limited efficacy, resulting in decreased quality of life (QOL) for many patients affected. Recent advances over the past decade have improved the understanding of the pathophysiology of chronic cough and the suspected neurobiological role leading to the development of novel therapeutic agents to help address this debilitating condition.
Chronic Cough Guidelines for Adult Patients
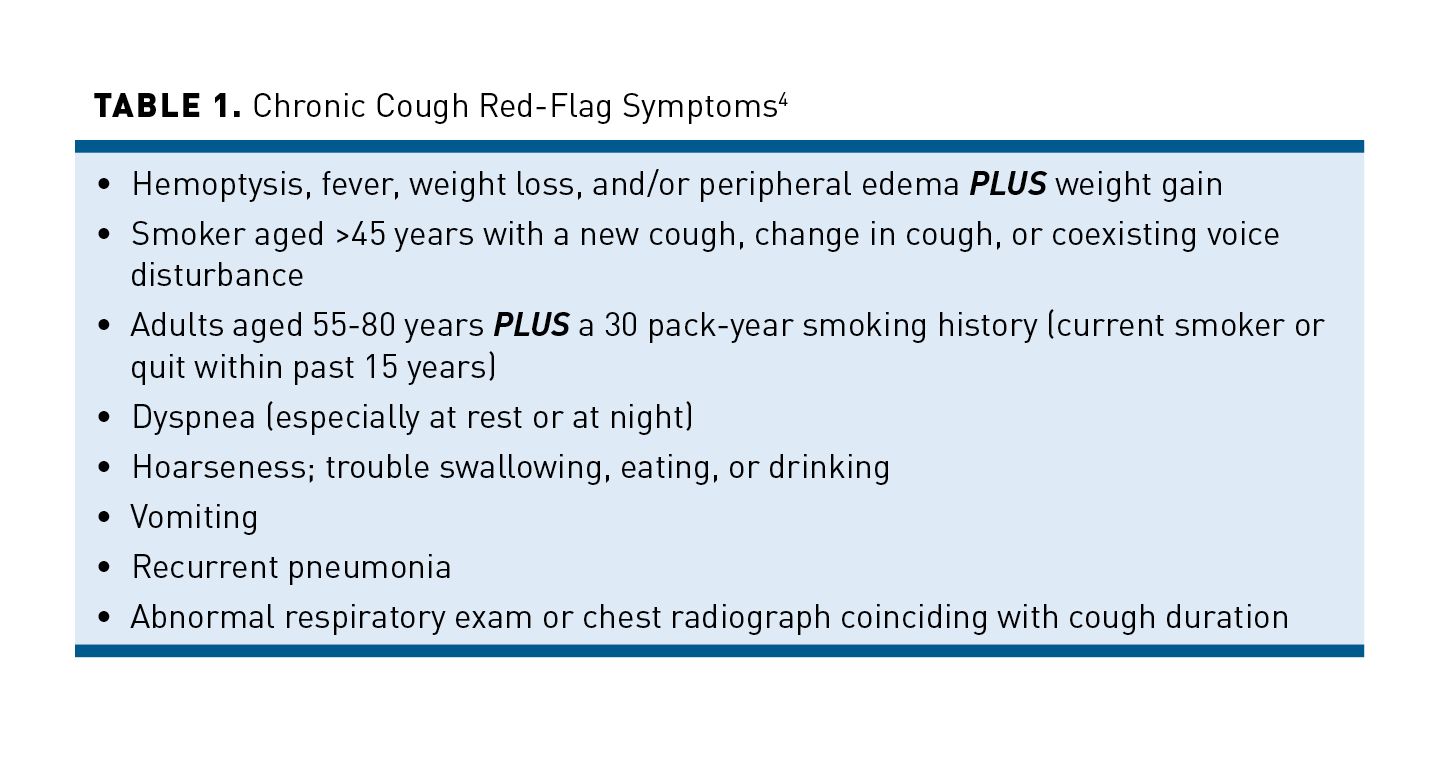
Currently, 2 major treatment guidelines address the medical management of RCC and UCC: those of the American College of Chest Physicians (ACCP or CHEST) and the European Respiratory Society (ERS).2,3 Both guidelines recommend a thorough history and physical when evaluating patients who present with chronic cough.2,3 A CHEST guideline and expert panel also recommend focusing on the identification of red-flag symptoms (see Table 14) and ruling out other conditions that either commonly or more rarely result in chronic cough.4
CHEST guidelines recommend that individuals with a known cause of their chronic cough have their therapy optimized for each diagnosis.2,3 Patients need to be assessed for adherence regularly, with frequent follow-up to monitor for barriers, efficacy of treatment, cough severity, and QOL. Education to avoid exposure to known environmental and occupational triggers should also be provided. A referral to a cough clinic should be considered in patients with RCC.2,3
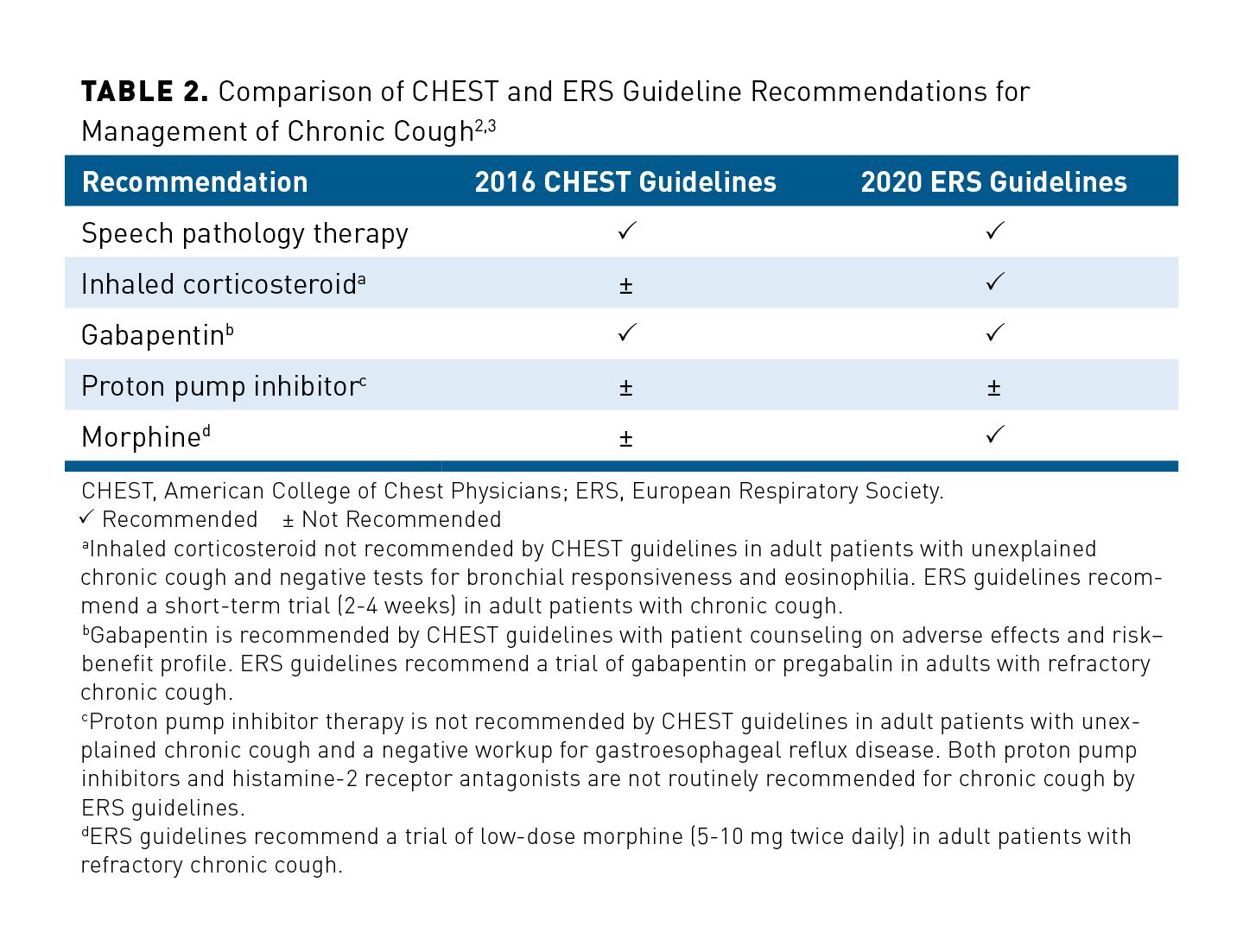
A comparison of CHEST and ERS guideline recommendations for the nonpharmacologic and pharmacologic treatment of chronic cough is outlined in Table 2.2,3 Both guidelines recommend a trial of speech pathology and gabapentin in patients with UCC and recommend against the use of proton pump inhibitors (PPIs) in the absence of gastroesophageal reflux disease (GERD). The guidelines differ in their recommendations of inhaled corticosteroids (ICS) and morphine.2,3 Current options for the management of RCC and UCC will be discussed in further detail in subsequent sections. Chronic cough management is often complex, requiring an individualized treatment plan. Therefore, treatment options discussed below include a summary of efficacy and tolerability data to guide clinical decision making.
Nonpharmacologic Treatment of Chronic Cough
Current CHEST guidelines recommend a trial of multimodality speech pathology therapy in patients with UCC.2 This recommendation was based on positive cough severity, randomized control trial data.5,6 Results of a systematic review by Chamberlain et al found 2 to 4 sessions of speech pathology that included education, cough suppression techniques, breathing exercises, laryngeal hygiene, and counseling resulted in decreased cough frequency, improved cough severity, and positive benefits on cough-related QOL.6
Speech pathology typically begins with measuring symptoms, assessing laryngeal physiology, and determining whether the individual is a good candidate for speech pathology treatment for chronic cough (SPTCC).7 The exact mechanism for chronic cough improvement after SPTCC is not fully elucidated. Individuals who present with a nonproductive cough; abnormal laryngeal sensations, such as tickle, itch, tightness, dryness, or globus; coughs triggered by nontussive stimuli, including perfumes, cold air, or talking; and low doses of tussive stimuli, such as chemical fumes or smoke, seem to improve the most from SPTCC. The desired outcomes for SPTCC include a reduced urge to cough, improved coping skills, decreased anxiety and depression, and reduced laryngeal constriction.7
Treatment of the Most Common Causes of Chronic Cough
Upper Airway Cough Syndrome (UACS)
Previously called postnasal drip syndrome, UACS is the most common cause of chronic cough in adults and should be addressed first when managing this condition.8,9 Patients may require further workups, such as allergy testing (allergic rhinitis) and computed tomography of the sinuses (sinusitis), as indicated on an individual patient basis.8,9
The etiology of UACS will dictate the selection of treatment for affected patients. Managing exposure to environmental irritants, such as perfumes or pollution, and any other offending agents, including pollen, dust, or mites, is a standard first-line nonpharmacologic therapy approach.8,9 Sinusitis can be managed via saline lavage, nasal corticosteroids, antihistamines, and antibiotics as needed.8,9 If the cause of chronic cough is unknown, then initiation of a decongestant (eg, pseudoephedrine, phenylephrine) plus a first-generation antihistamine (eg, chlorpheniramine) may be started initially.10 Other therapies, such as intranasal corticosteroids (eg, fluticasone), saline lavage, nasal anticholinergics (eg, ipratropium), and antihistamines (eg, cetirizine, fexofenadine, loratadine), may also be considered. Typically, clinical improvement is expected within days to weeks, with a maximum of 2 months for resolution of UACS.9,10
Angiotensin-Converting Enzyme (ACE) Inhibitor-Induced Cough
ACE inhibitor-induced cough is a common cause among individuals on ACE inhibitor therapy.10 Upon discontinuation, the ACE inhibitor-induced cough typically resolves within 1 week to 3 months. Angiotensin receptor blockers (ARBs) are commonly prescribed as a replacement for patients who experience ACE inhibitor-induced coughs. Depending on the clinical circumstance, providers may choose to restart ACE inhibitor therapy, and the reoccurrence of cough may not occur in some patients.10,11
Asthma
Asthma is another common cause of chronic cough, and treatment should begin with patient education on smoking cessation and the avoidance of potential triggers.9,10 Asthma treatment should then follow guidelines from the Global Initiative for Asthma (GINA) cycle of asthma care.12,13 The GINA control-based cycle of asthma care starts with the assessment of a patient’s symptom control and risk factors, inhaler technique and adherence, and patient preferences. Treatment should be adjusted, taking into consideration modifiable risk factors, current asthma medications, and any nonpharmacologic strategies being employed. Then, the patient’s response to the treatment plan is reviewed, addressing aspects including symptoms, exacerbations, adverse effects (AEs), patient satisfaction, and lung function, and the process continues with assessment.10,12
Pharmacologic treatment usually consists of a bronchodilator (eg, albuterol) and an ICS (eg, budesonide). Leukotriene receptor antagonists (eg, montelukast, zafirlukast) are also sometimes added. Severe or refractory cough usually will require an oral corticosteroid (eg, prednisone, methylprednisolone) for 5 to 10 days.10
Chronic Obstructive Pulmonary Disease (COPD)
COPD frequently causes a chronic cough, but, unlike asthma, patients typically do not have undiagnosed COPD. Because symptoms of asthma and COPD can overlap, it is important to use spirometry to aid in the diagnosis, so proper treatment can be administered.
Treatment of COPD should follow the stepwise approach recommended by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines.14 Pharmacologic agents usually include an inhaled bronchodilator, inhaled anticholinergic, and ICS. A short course (5-7 days) of an oral corticosteroid (plus or minus antibiotics) may be used for acute management of exacerbations.14
Gastroesophageal Reflux Disease (GERD)
GERD has been associated with chronic cough in research, but treatment is considered controversial as the pathophysiology of cough related to GERD is highly complex.10,15 The 2016 CHEST and expert panel guideline recommend individuals suspected to have reflux-cough syndrome first begin with diet modification to lose weight in patients who are overweight or obese, elevating the head of the bed, and avoiding meals within 3 hours of bedtime.15
Among individuals with reported acid reflux and regurgitation, antacid agents, such as histamine-2 receptor antagonists (H2 RAs), PPIs, alginate, and calcium carbonate, are recommended to alleviate symptoms.15 PPI therapy is not recommended by CHEST among those who have chronic cough without acid reflux or regurgitation, as treatment is considered unlikely to be effective. Gastroesophageal symptoms typically respond within 4 to 8 weeks but may take up to 3 months. Chronic cough that persists beyond the 3-month antacid therapy trial should be further evaluated; additional diagnostic tests, such as esophageal manometry and/or pH-metry, should be conducted as indicated.15
Nonasthmatic Eosinophilic Bronchitis (NAEB)
NAEB is another common cause of chronic cough that is characterized by unresponsiveness to bronchodilators.10 Avoidance of inhaled allergens due to occupational exposure should be considered first when there is a known cause. ICS are usually effective for NAEB, and oral corticosteroids can be considered after failure of high-dose ICS.10,16
Traditional Pharmacologic Agents for Chronic Cough
Nonprescription Products
The majority of products sold without a prescription for cough relief (eg, dextromethorphan, guaifenesin, diphenhydramine, and, in some states, low-dose codeine) are not considered more effective than placebo when studied in randomized clinical trials for cough suppression.17,18 These agents are readily available, inexpensive, and typically safe when used appropriately per nonprescription product labeling. Therefore, they are commonly used to address acute and chronic cough among patients who self-treat. However, none of these agents is indicated for chronic cough, so patients should be referred to their provider for further workup.
Opiates
Codeine and morphine are the most used opiate antitussives.19 Codeine has been used for more than 200 years to treat cough, including tuberculosis-induced cough. It has a rapid onset of action, and responders are easily identified from nonresponders within 1 to 2 weeks of initiation. Approximately 50% of patients with chronic cough will have a suboptimal cough suppression. Further, additional limitations, such as individual variability with codeine metabolism (CYP2D6) and potential safety concerns, are important considerations. Patients who are poor metabolizers (little to no CYP2D6 activity) will have a decreased response to codeine. AEs, such as constipation and nausea, are common with codeine treatment.19 The efficacy of codeine is not well supported in clinical trials. Results of a trial by Smith and colleagues that investigated the use of 60 mg codeine phosphate daily did not find it to be more effective than placebo for reducing objective or subjective cough frequency or severity in individuals with COPD and cough.20 Additional studies are needed to fully ascertain the utility of codeine in patients with chronic cough.
Morphine is an alternative opiate to codeine that is typically reserved for the most severe intractable coughs and is not recommended in current CHEST guidelines.2,19 In contrast with codeine, morphine does not exhibit the CYP2D6 variability in metabolism and is approximately 10 times more potent.19 Due to safety risks including respiratory depression, drowsiness, addiction, and accidental overdose, patients should be closely monitored. The efficacy and tolerability of morphine (5-10 mg) extended-release was evaluated in a 4-week randomized, placebo-controlled, crossover study (N = 27) in patients with chronic cough.21 Those who were treated with morphine reported a significant difference in the Leicester Cough Questionnaire (LCQ) score compared with placebo (mean difference, 2; P <.02) and daily cough severity score (range, 0; mean difference, –3.4 ± 1.8; P <.01). Although treatment was generally well tolerated and most effects were observed within the first week, 18 of 27 enrolled patients continued on to the extension study, and two-thirds opted to double their dose due to inadequate control of their cough during the core study.19,21
Neuromodulator Agents
Gabapentin inhibits α2δ subunits on voltage-gated calcium channels and is approved for the treatment of seizures and neuropathic pain within the United States.22 It is now also considered a possible therapeutic option in patients with chronic cough based on improved understanding of chronic cough pathophysiology.23,24 The efficacy of gabapentin was evaluated in a 10-week randomized controlled trial (N = 62) in patients with RCC, and results indicated that gabapentin (1800 mg/day) significantly improved LCQ scores compared with placebo (P = .004). It also decreased cough severity scores (P = .029) and objective cough frequency (P = .028) by week 8. Once treatment was discontinued, the antitussive effects were not sustained.23 Current CHEST guidelines recommend a trial of gabapentin as long as patients are educated on the potential for AEs and the risk−benefit profile along with a reassessment of risk−benefit at 6 months before continuing therapy.2
Pregabalin is a structural derivative of γ-aminobutyric acid and binds α2δ subunits on voltage-gated calcium channels.25 Like gabapentin, pregabalin has also been evaluated for efficacy in RCC. A 14-week study evaluated pregabalin as adjunctive treatment to speech pathology therapy and demonstrated a significant improvement in LCQ scores (P = .024) and decreased cough severity (P = .002) compared with just speech pathology alone.26
Both gabapentin and pregabalin are associated with AEs, such as drowsiness, confusion, fatigue, and blurred vision, which have led to discontinuation.23,26 It has also been proposed that both gabapentin and pregabalin may just alter the perception of cough versus controlling cough.23,26 Therefore, additional randomized controlled trials are required to fully ascertain the utility of these agents in the treatment of chronic cough.
The tricyclic antidepressant amitriptyline is FDA approved for depression and is also frequently used for the treatment of anxiety, neuropathic pain, and potentially for chronic cough.27,28 At the time of this writing, no placebo-controlled randomized clinical trials are evaluating the efficacy of amitriptyline in the treatment of chronic cough. A small randomized trial (N = 28) evaluated the efficacy of amitriptyline 10 mg in patients with post-viral vagal neuropathy cough.29 Amitriptyline was shown to be significantly more effective compared with the combination of codeine/guaifenesin in complete cough response and cough-specific QOL at 10 days.29 A major limitation of this study was that neither objective cough frequency nor any safety outcomes were measured. Additional research is required to fully elucidate the role of amitriptyline in the treatment of chronic cough.
Novel Emerging Agents for Chronic Cough
The lack of efficacy of traditional antitussive agents combined with an improved understanding of the neurobiology of the cough reflex has led to an increased focus on the development of new agents to address this treatment gap.30,31 The new chronic cough agents target specific receptors or channels in the peripheral sensory neurons with the goal of reduced central nervous system AEs and control of hypersensitivity while reserving the protective cough response.32
Transient Receptor Potential Receptor Vanilloid-1 (TRPV1) Antagonists
The TRPV1 channel was the first therapeutic target evaluated for chronic cough.32 TRPV1 channels are present in both peripheral neurons and nonneuronal cells.19 They are activated by hot temperatures (>43 °C), acidic pH, or inflammatory mediators and recognize capsaicin.33 Two subsequent clinical trials in patients with chronic cough did not demonstrate that TRPV1 antagonists were clinically beneficial in the treatment of chronic cough.34,35 SB-705498, a highly selective and potent competitive antagonist for TRPV1 receptors, has shown to significantly affect the capsaicin cough reflex but had almost no effect on objective cough frequency, cough severity scores, or CQLQ scores.35 XEN-D0501, which is significantly more potent than SB-705498 in vivo, exhibited similar results and failed to significantly reduce cough frequency in patients with chronic cough compared with placebo (P = .41).34
Transient Receptor Potential Ankyrin-1 (TRPA1) Antagonist
TRPA1 is an environmental-sensing member of the transient receptor potential channel family.19 This channel family is activated by cold temperature (<17 °C), cigarette smoke, cinnamaldehyde, acrolein, and other various cough irritants.36 Cold air is a common trigger observed clinically among patients with chronic cough, leading to optimism for this potential therapeutic target.37-39 An early-phase clinical trial investigating the potent TRPA1 antagonist GRC 17536 did not demonstrate a clinical benefit compared with placebo in patients with RCC.40 At the current time of writing, there are no other TRPA1 antagonist clinical trials underway within the United States.
P2X3 Antagonists
P2X3 receptors play an important role in the activation of sensory neurons integral to the cough reflex (Aδ-fibres and C-fibres).41 Combined with an increased understanding of afferent sensitization in airway dysfunction among patients with chronic cough, P2X3 receptor antagonists are being investigated as a potential therapeutic option.1
Gefapixant
Gefapixant (MK-7264/AF-219) is a novel, first-in-class, nonnarcotic, selective antagonist of the P2X3 receptor currently in clinical trials evaluating its safety and efficacy for treatment of chronic cough.41 Phase 1 and 2 clinical trials evaluated more than 300 patients and demonstrated positive results for decreased mean daytime cough frequency, 24-hour cough frequency, and awake cough frequency.42-44 Phase 1 trials used a significantly higher dose of gefapixant (600 mg), resulting in major taste disturbances due to inhibition of the P2X2/3 channels.43 Subsequent dose-finding studies found an optimal dose of 30 mg to 50 mg twice daily.43 Gefapixant was generally well tolerated in all phase 2 trials with no major safety concerns. Dose-dependent dysgeusia was the most common AE and should subside with discontinuation of gefapixant.41
Following the positive results from phase 1 and 2 trials, investigation of the utility of gefapixant was continued into phase 3 clinical trials. Two parallel, double-blind, randomized, placebo-controlled trials (ClinicalTrial.gov Identifiers: NCT03449134 [COUGH-1], NCT03449147 [COUGH-2]) were conducted to assess the efficacy and safety of gefapixant (15 mg or 45 mg twice daily) in patients with chronic cough.41,45-47 The primary efficacy outcomes included 24-hour cough frequency (at week 24), percentage of at least 1 AE during treatment and follow-up (up to 54 weeks), and percentage of participants who discontinued due to an AE (up to 52 weeks). The results of COUGH-1 and COUGH-2 were presented virtually at the European Respiratory Society International Congress in August 2020. Reported results found a statistically significant reduction in 24-hour cough frequency versus placebo at 12 weeks (COUGH-1) (18.45%, P = .041) and 24 weeks (COUGH-2) (14.64%, P = .031) in patients treated with gefapixant 45 mg twice daily.47 Gefapixant 15 mg twice daily treatment arms did not meet the primary efficacy end point in either study. AEs reported were consistent with previous trials (dysgeusia occurring at a higher incidence with gefapixant 45 mg twice daily), and discontinuations of study drugs due to AEs were more frequent in the gefapixant 45 mg treatment arms compared to the gefapixant 15 mg and placebo arms.
BAY1817080, BLU-5937, and S-600918
Three additional P2X3 antagonists, BAY1817080, BLU-5937, and S-600918, are newer agents under investigation that are highly selective and may cause less dysgeusia compared with gefapixant. Each is discussed further in the following paragraphs (ClinicialTrials.gov identifiers NCT03310645, NCT03979638, and NCT04110054, respectively).48-50
The results from the BAY1817080 phase 1/2a double-blind, placebo-controlled, randomized, 2-way crossover trial (NCT03310645) was presented at the American Thoracic Society International conference virtually in August 2020.51 Reported results found BAY1817080 caused AEs in 41% to 49% of patients, with the majority being mild. Taste-disturbance AEs were dose dependent and occurred in 5% to 21% of patients. The 24-hour cough frequency counts were decreased with higher BAY1817080 doses compared with placebo (50 mg, P = .054; 200 mg, P = .004; 750 mg, P = .002). Cough frequency counts also decreased from baseline by 17% (P = .025) and patient-reported cough severity was significantly improved compared with placebo.51
The BLUE-5937 (RELIEF) trial was a phase 2, randomized, double-blind, placebo-controlled, crossover, dose-escalation study.49 Individuals received two 16-day treatment periods with 4 escalating doses or matching placebo at 4-day intervals. The two 16-day treatment periods were separated by a 10- to 14-day washout period, with a 14-day follow-up period. The trial was terminated early in June 2020 due to the impact of the novel coronavirus 2019 (COVID-19) pandemic on clinical trial activities. There were 68 patients enrolled in the trial, and 52 completed the dosing trial.49 Topline results from the RELIEF trial are expected to be released sometime in 2020.52
The trial evaluating S-600918 is a phase 2b trial that is actively recruiting patients to determine the optimal dose of S-600918 in patients with RCC via a change in baseline in 24-hour cough frequency compared with placebo. The investigators expect to enroll 372 participants who will receive 50 mg, 150 mg, or 300 mg of S-600918, or placebo for 28 days. The anticipated study completion date is May 25, 2021.50
Neurokinin-1 Receptor (NK-1) Antagonists
NK-1 and substance P (SP) are suspected of playing an important role in the induction and maintenance of cough reflex hypersensitivity.53,54 This is evidenced by the increased SP concentrations in biological fluids and an increased cough response with inhaled SP in patients with idiopathic pulmonary fibrosis and acute cough.55-60
Evidence for the utility of NK-1 receptor antagonists first came from a randomized, double-blind, placebo-controlled, crossover pilot study (N = 20) evaluating aprepitant in patients with lung cancer-associated cough. Statistically significant improvements in cough frequency, cough severity, and QOL were observed.61
Recently, a phase 2, open-label, pilot study (VOLCANO-1) was conducted to evaluate efficacy and safety of orvepitant, a selective, centrally acting NK-1 receptor antagonist, in 13 patients with RCC.61-63 Orvepitant demonstrated a statistically significant decrease in objective daytime cough frequency at week 4 (P <.001). The decreased cough frequency occurred early with a measurable improvement by week 1 (P = .001) and was sustained after discontinuation of orvepitant at week 8 (P = .020). Orvepitant also significantly improved severity scores and QOL, with a favorable safety profile.63
VOLCANO-2 was a phase 2b, placebo-controlled trial (N = 275) conducted over 12 weeks in patients with RCC and a baseline awake cough frequency of at least 10 coughs/hour (ClinicalTrials.gov identifier NCT02993822).64,65 The primary cough frequency end point was not significant; however, an improved efficacy trend was observed among patients taking 30 mg orvepitant and a higher cough frequency (≈66.7 coughs/hour) compared with placebo (P = .066). The most common AEs included headache, dizziness, fatigue, and somnolence.65,66
Other Agents Considered for Chronic Cough Treatment
Several other agents, such as esomeprazole, erythromycin, and ipratropium bromide, have been evaluated by CHEST guidelines for patients with chronic cough.2 However, due to various factors including small sample size, lack of results replication, and lack of efficacy, among others, they are not currently recommended for the treatment of chronic cough.2 Multiple other therapies are in various stages of investigation for their utility in the treatment of chronic cough, including TRPV4 antagonists, voltage-gated sodium channel blockers, γ-aminobutyric acid (GABA) B receptor agonists, nicotinic acetylcholine receptor α7-subunit agonists, and inhaled sodium cromoglycate.19
Conclusions
In summary, RCC and UCC are disabling conditions that historically lacked effective treatment options. Any patient who presents with RCC or UCC must be thoroughly worked up (including a detailed medical and medication history), evaluated for any red-flag symptoms, and asssessed by a differential diagnosis for common and uncommon causes of chronic cough before a treatment approach is developed. If a specific etiology is discovered, that condition should be optimally treated first before treating the chronic cough. Current guidelines recommend nonpharmacologic and pharmacologic treatments based on individual patient circumstances and should follow a guideline/protocol process. Traditional treatments, such as speech therapy, opiates, and neuromodulators, have had limited success in improving cough frequency, severity, and QOL in patients affected. As a result, increased research has focused on the development of novel therapeutic targets based on an increased understanding of the neurobiology associated with the cough reflex. These new agents have demonstrated positive benefits for reducing cough frequency, severity, and QOL while being generally well tolerated in clinical trials. Therefore, it is likely that some of these agents may become available for treating patients and may help improve their QOL.
Author affiliation: Phung C. On, PharmD, BCPS, is assistant professor of pharmacy practice, Massachusetts College of Pharmacy and Health Sciences; and a clinical pharmacy specialist—transitions of care, Boston Health Care for the Homeless Program, both in Boston, MA.
Funding source: This activity is supported by an educational grant from Merck Sharp & Dohme Corp.
Author disclosure: Dr On has no relevant financial relationships with commercial interests to disclose.
Authorship information: Substantial contributions to concept and design; supervision; and drafting of the manuscript.
Address correspondence to: phung.on1@mcphs.edu
Medical writing and editorial support: Brittany Hoffmann-Eubanks, PharmD, MBA
REFERENCES
1. Smith JA, Woodcock A. Chronic cough. N Engl J Med. 2016;375(16):1544-1551. doi: 10.1056/NEJMcp1414215
2. Gibson P, Wang G, McGarvey L, Vertigan AE, Altman KW, Birring SS; CHEST Expert Cough Panel. Treatment of unexplained chronic cough: CHEST guideline and expert panel report. Chest. 2016;149(1):27-44. doi: 10.1378/chest.15-1496
3. Morice AH, Millqvist E, Bieksiene K, et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J. 2020;55(1):1901136. doi: 10.1183/13993003.01136-2019
4. Irwin RS, French CL, Chang AB, Altman KW; CHEST Expert Cough Panel. Classification of cough as a symptom in adults and management algorithms: CHEST guideline and expert panel report. Chest. 2018;153(1):196-209. doi: 10.1016/j.chest.2017.10.016
5. Vertigan AE, Theodoros DG, Gibson PG, Winkworth AL. Efficacy of speech pathology management for chronic cough: a randomised placebo controlled trial of treatment efficacy. Thorax. 2006;61(12):1065-1069. doi: 10.1136/thx.2006.064337
6. Chamberlain S, Birring SS, Garrod R. Nonpharmacological interventions for refractory chronic cough patients: systematic review. Lung. 2014;192(1):75-85. doi: 10.1007/s00408 013-9508-y
7. Vertigan AE, Haines J, Slovarp L. An update on speech pathology management of chronic refractory cough. J Allergy Clin Immunol Pract. 2019;7(6):1756-1761. doi: 10.1016/j.jaip.2019.03.030
8. Pratter MR, Bartter T, Akers S, DuBois J. An algorithmic approach to chronic cough. Ann Intern Med. 1993;119(10):977-983. doi: 10.7326/0003-4819-119-10-199311150-00003
9. Kaplan AG. Chronic cough in adults: make the diagnosis and make a difference. Pulm Ther. 2019;5(1):11-21. doi: 10.1007/s41030-019-0089-7
10. Michaudet C, Malaty J. Chronic cough: evaluation and management. Am Fam Physician. 2017;96(9):575-580.
11. Dicpinigaitis PV. Angiotensin-converting enzyme inhibitor-induced cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl 1):169s-173s. doi: 10.1378/chest.129.1_suppl.169S
12. Reddel HK, Bateman ED, Becker A, et al. A summary of the new GINA strategy: a roadmap to asthma control. Eur Respir J. 2015;46(3):622-639. doi: 10.1183/13993003.008532015
13. Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2020. Accessed September 8, 2020. ginasthma.org
14. Global Initiative for Chronic Obstructive Lung Disease. 2020 GOLD Reports. Published 2020. Accessed June 22, 2020. goldcopd.org/gold-reports/
15. Kahrilas PJ, Altman KW, Chang AB, et al; CHEST Expert Cough Panel. Chronic cough due to gastroesophageal reflux in adults: CHEST guideline and expert panel report. Chest. 2016;150(6):1341-1360. doi: 10.1016/j.chest.2016.08.1458
16. Brightling CE. Cough due to asthma and nonasthmatic eosinophilic bronchitis. Lung. 2010;188(suppl 1):S13-S17. doi: 10.1007/s00408-009-9163-5
17. Dicpinigaitis PV, Morice AH, Birring SS, et al. Antitussive drugs--past, present, and future. Pharmacol Rev. 2014;66(2):468-512. doi: 10.1124/pr.111.005116
18. Dicpinigaitis PV. Clinical perspective - cough: an unmet need. Curr Opin Pharmacol. 2015;22:24-28. doi: 10.1016/j.coph.2015.03.001
19. Song WJ, Chung KF. Pharmacotherapeutic options for chronic refractory cough. Expert Opin Pharmacother. 2020;21(11):1345-1358. doi: 10.1080/14656566.2020.1751816
20. Smith J, Owen E, Earis J, Woodcock A. Effect of codeine on objective measurement of cough in chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2006;117(4):831-835. doi: 10.1016/j.jaci.2005.09.055
21. Morice AH, Menon MS, Mulrennan SA, et al. Opiate therapy in chronic cough. Am J Respir Crit Care Med. 2007;175(4):312-315. doi: 10.1164/rccm.200607-892OC
22. Neurontin. Prescribing information. Pfizer, Inc; 2020. Accessed September 9, 2020. labeling.pfizer.com/ShowLabeling.aspx?format=PDF&id=630
23. Ryan NM, Birring SS, Gibson PG. Gabapentin for refractory chronic cough: a randomised, double-blind, placebo-controlled trial. Lancet. 2012;380(9853):1583-1589. doi: 10.1016/s0140-6736(12)60776-4
24. Chung KF, McGarvey L, Mazzone SB. Chronic cough as a neuropathic disorder. Lancet Respir Med. 2013;1(5):414-422. doi: 10.1016/s2213-2600(13)70043-2
25. Halum SL, Sycamore DL, McRae BR. A new treatment option for laryngeal sensory neuropathy. Laryngoscope. 2009;119(9):1844-1847. doi: 10.1002/lary.20553
26. Vertigan AE, Kapela SL, Ryan NM, Birring SS, McElduff P, Gibson PG. Pregabalin and speech pathology combination therapy for refractory chronic cough: a randomized controlled trial. Chest. 2016;149(3):639-648. doi: 10.1378/chest.15-1271
27. Thour A, Marwaha R. Amitriptyline. In: StatPearls. StatPearls Publishing. Updated July 10, 2020. Accessed September 9, 2020. ncbi.nlm.nih.gov/books/NBK537225/
28. Bowen AJ, Nowacki AS, Contrera K, et al. Short- and long-term effects of neuromodulators for unexplained chronic cough. Otolaryngol Head Neck Surg. 2018;159(3):508-515. doi: 10.1177/0194599818768517
29. Jeyakumar A, Brickman TM, Haben M. Effectiveness of amitriptyline versus cough suppressants in the treatment of chronic cough resulting from postviral vagal neuropathy. Laryngoscope. 2006;116(12):2108-2112. doi: 10.1097/01.mlg.0000244377.60334.e3
30. Mazzone SB, Chung KF, McGarvey L. The heterogeneity of chronic cough: a case for endotypes of cough hypersensitivity. Lancet Respir Med. 2018;6(8):636-646. doi: 10.1016/s2213-2600(18)30150-4
31. Canning BJ, Chang AB, Bolser DC, Smith JA, Mazzone SB, McGarvey L. Anatomy and neurophysiology of cough: CHEST guideline and expert panel report. Chest. 2014;146(6):1633-1648. doi: 10.1378/chest.14-1481
32. Song WJ, Morice AH. Cough hypersensitivity syndrome: a few more steps forward. Allergy Asthma Immunol Res. 2017;9(5):394-402. doi: 10.4168/aair.2017.9.5.394
33. Lee LY, Ni D, Hayes D Jr, Lin RL. TRPV1 as a cough sensor and its temperature-sensitive properties. Pulm Pharmacol Ther. 2011;24(3):280-285. doi: 10.1016/j.pupt.2010.12.003
34. Belvisi MG, Birrell MA, Wortley MA, et al. XEN-D0501, a novel transient receptor potential vanilloid 1 antagonist, does not reduce cough in patients with refractory cough. Am J Respir Crit Care Med. 2017;196(10):1255-1263. doi: 10.1164/rccm.201704-0769OC
35. Khalid S, Murdoch R, Newlands A, et al. Transient receptor potential vanilloid 1 (TRPV1) antagonism in patients with refractory chronic cough: a double-blind randomized controlled trial. J Allergy Clin Immunol. 2014;134(1):56-62. doi: 10.1016/j.jaci.2014.01.038
36. Birrell MA, Belvisi MG, Grace M, et al. TRPA1 agonists evoke coughing in guinea pig and human volunteers. Am J Respir Crit Care Med. 2009;180(11):1042-1047. doi: 10.1164/rccm.200905-0665OC
37. Hilton E, Marsden P, Thurston A, Kennedy S, Decalmer S, Smith JA. Clinical features of the urge-to-cough in patients with chronic cough. Respir Med. 2015;109(6):701-707. doi: 10.1016/j.rmed.2015.03.011
38. Vertigan AE, Gibson PG. Chronic refractory cough as a sensory neuropathy: evidence from a reinterpretation of cough triggers. J Voice. 2011;25(5):596-601. doi: 10.1016/j.jvoice.2010.07.009
39. Won HK, Kang SY, Kang Y, et al. Cough-related laryngeal sensations and triggers in adults with chronic cough: symptom profile and impact. Allergy Asthma Immunol Res. 2019;11(5):622-631. doi: 10.4168/aair.2019.11.5.622
40. Morice AH. TRPA1 receptors in chronic cough. Pulm Pharmacol Ther. 2017;47:42-44.
doi: 10.1016/j.pupt.2017.05.004
41. Muccino D, Green S. Update on the clinical development of gefapixant, a P2X3 receptor antagonist for the treatment of refractory chronic cough. Pulm Pharmacol Ther. 2019;56:75-78. doi: 10.1016/j.pupt.2019.03.006
42. Abdulqawi R, Dockry R, Holt K, et al. P2X3 receptor antagonist (AF-219) in refractory chronic cough: a randomised, double-blind, placebo-controlled phase 2 study. Lancet. 2015;385(9974):1198-1205. doi: 10.1016/s0140-6736(14)61255-1
43. Smith JA, Kitt MM, Butera P, et al. Gefapixant in two randomised dose-escalation studies in chronic cough. Eur Respir J. 2020;55(3):1901615. doi: 10.1183/13993003.01615-2019
44. Smith JA, Kitt MM, Morice AH, et al; Protocol 012 Investigators. Gefapixant, a P2X3 receptor antagonist, for the treatment of refractory or unexplained chronic cough: a randomised, double-blind, controlled, parallel-group, phase 2b trial. Lancet Respir Med. 2020;8(8):775-785. doi: 10.1016/s2213-2600(19)30471-0
45. Phase 3 Study of Gefapixant (MK-7264) in Adult Participants With Chronic Cough (MK-7264-027). ClinicalTrials.gov identifier: NCT03449134. Updated August 25, 2020. Accessed September 9, 2020. clinicaltrials.gov/ct2/show/NCT03449134
46. A Study of Gefapixant (MK-7264) in Adult Participants With Chronic Cough (MK-7264-030). ClinicalTrials.gov identifier: NCT03449147. Updated August 26, 2020. Accessed September 9, 2020. clinicaltrials.gov/ct2/show/NCT03449147
47. Merck’s gefapixant (45 mg twice daily) significantly decreased cough frequency compared to placebo at week 12 and 24 in patients with refractory or unexplained chronic cough. Business Wire; September 8, 2020. Accessed September 17, 2020. merck.com/news/mercks-gefapixant-45-mg-twice-daily-significantly-decreased-cough-frequency-compared-to-placebo-at-week-12-and-24-in-patients-with-refractory-or-unexplained-chronic-cough/
48. Repeat Doses of BAY 1817080 in Healthy Males & Proof of Concept in Chronic Cough Patients. ClinicalTrials.gov identifier: NCT03310645. Updated July 18, 2019. Accessed September 9, 2020. clinicaltrials.gov/ct2/show/NCT03310645
49. A Dose Escalation Study of BLU-5937 in Unexplained or Refractory Chronic Cough (RELIEF). ClinicalTrials.gov identifier: NCT03979638. Updated September 2, 2020. Accessed September 9, 2020. clinicaltrials.gov/ct2/show/NCT03979638
50. Evaluation of S-600918 in Adults With Refractory Chronic Cough. ClinicalTrials.gov identifier: NCT04110054. Updated August 7, 2020. Accessed September 9, 2020. clinicaltrials.gov/ct2/show/NCT04110054
51. Morice AH, Smith J, McGarvey L, et al. Safety and efficacy of BAY 1817080, a P2X3 receptor antagonist, in patients with refractory chronic cough (RCC). Am J Respir Crit Care Med. 2020;201(A7648). Accessed September 9, 2020. atsjournals.org/doi/abs/10.1164/ajrccm-conference.2020.201.1_MeetingAbstracts.A7648
52. BELLUS Health announces completion of dosing in phase 2 RELIEF trial with BLU-5937 for the treatment of refractory chronic cough. News release. Business Wire; April 6, 2020. Accessed June 22, 2020. businesswire.com/news/home/20200406005773/en
53. Ujiie Y, Sekizawa K, Aikawa T, Sasaki H. Evidence for substance P as an endogenous substance causing cough in guinea pigs. Am Rev Respir Dis. 1993;148(6 Pt 1):1628-1632. doi: 10.1164/ajrccm/148.6_Pt_1.1628
54. Morice AH, Lowry R, Brown MJ, Higenbottam T. Angiotensin-converting enzyme and the cough reflex. Lancet. 1987;2(8568):1116-1118. doi: 10.1016/s0140-6736(87)91547-9
55. Katsumata U, Sekizawa K, Inoue H, Sasaki H, Takishima T. Inhibitory actions of procaterol, a beta-2 stimulant, on substance P-induced cough in normal subjects during upper respiratory tract infection. Tohoku J Exp Med. 1989;158(1):105-106. doi: 10.1620/tjem.158.105
56. Hope-Gill BD, Hilldrup S, Davies C, Newton RP, Harrison NK. A study of the cough reflex in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2003;168(8):995-1002. doi: 10.1164/rccm.200304-597OC
57. Lim KG, Rank MA, Kita H, Patel A, Moore E. Neuropeptide levels in nasal secretions from patients with and without chronic cough. Ann Allergy Asthma Immunol. 2011;107(4):360-363. doi: 10.1016/j.anai.2011.07.010
58. Bae YJ, Moon KA, Kim TB, et al. The role of nitrosative stress in the pathogenesis of unexplained chronic cough with cough hypersensitivity. Am J Rhinol Allergy. 2012;26(1):e10-e14. doi: 10.2500/ajra.2012.26.3730
59. Patterson RN, Johnston BT, Ardill JE, Heaney LG, McGarvey LP. Increased tachykinin levels
in induced sputum from asthmatic and cough patients with acid reflux. Thorax. 2007;62(6):491-495. doi: 10.1136/thx.2006.063982
60. Otsuka K, Niimi A, Matsumoto H, et al. Plasma substance P levels in patients with persistent cough. Respiration. 2011;82(5):431-438. doi: 10.1159/000330419
61. Harle A, Blackhail F, Molassiotis A, et al. Neurokinin-1 receptor antagonism for the treatment of cough in lung cancer. Eur Respir J. 2016;48:PA3547.
62. Di Fabio R, Alvaro G, Braggio S, et al. Identification, biological characterization and pharmacophoric analysis of a new potent and selective NK1 receptor antagonist clinical candidate. Bioorg Med Chem. 2013;21(21):6264-6273. doi: 10.1016/j.bmc.2013.09.001
63. Smith J, Allman D, Badri H, et al. The neurokinin-1 receptor antagonist orvepitant is a novel antitussive therapy for chronic refractory cough: results from a phase 2 pilot study (VOLCANO-1). Chest. 2020;157(1):111-118. doi: 10.1016/j.chest.2019.08.001
64. A Dose-ranging Study of Orvepitant in Patients With Chronic Refractory Cough. ClinicalTrials.gov identifier: NCT02993822. Updated March 13, 2020. Accessed September 9, 2020. clinicaltrials.gov/ct2/show/NCT02993822
65. Smith J, Ballantyne E, Kerr M, et al. The neurokinin-1 receptor antagonist orvepitant improves chronic cough symptoms: results from a phase 2b trial. Published 2019. Accessed June 22, 2020. nerretherapeutics.com/wp-content/uploads/2019/09/ers-2019-poster.pdf
66. NeRRe Therapeutics announces positive findings from phase 2b study with orvepitant in chronic cough. News release. NeRRe Therapeutics; June 7, 2019. Accessed June 22, 2020. nerretherapeutics.com/nerre-therapeutics-announces-positive-findings-from-phase-2b-study-with-orvepitant-in-chronic-cough
