- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Type 2 Diabetes in the US Managed Care Setting: The Burden of Disease and Rationale for an Oral Glucagon-like Peptide-1 Receptor Agonist
Abstract
Diabetes affects an estimated 34 million US adults, with type 2 diabetes (T2D) accounting for 90% to 95% of cases. The downstream consequences of uncontrolled T2D are substantial, including an increased risk of microvascular complications (eg, renal impairment, retinopathy, and peripheral neuropathy), cardiovascular disease, impaired quality of life, and death. Overall, diabetes places a significant strain on the US health care system, with 7.8 million hospitalizations annually among patients with diabetes, and $237 billion in direct medical costs. Injectable glucagon-like peptide-1 receptor agonists (GLP-1RAs) have been available for T2D for over a decade, and are recommended, in particular, for patients with a compelling need to minimize hypoglycemia risk, curtail weight gain, or promote weight loss, and for patients with established cardiovascular disease. Despite being associated with high glucoselowering efficacy, weight loss, and a low risk of hypoglycemia, injectable GLP-1RAs are relatively underutilized, and are associated with suboptimal adherence and persistence. These challenges may relate in part to the injectable route of administration, given that injection-related concerns have been linked with a failure to intensify T2D therapy in a timely manner (ie, therapeutic inertia), and are cited by patients as a barrier to initiating and persisting with injectable treatments. The approval of the first tablet formulation of a GLP-1RA for T2D, oral semaglutide, has the potential to address these challenges. In this context, we review the burden of T2D in the United States, the role of GLP-1RAs, the challenges of therapeutic inertia and poor adherence, and the rationale for an oral GLP-1RA, focusing on considerations for managed care.
Am J Manag Care. 2020;26:S325-S334. https://doi.org/10.37765/ajmc.2020.88552
For author information and disclosures, see end of text.
Introduction
Diabetes represents a major and growing challenge. In 2018, 34 million US adults were estimated to have diabetes (both diagnosed and undiagnosed)1; this number is predicted to increase to approximately 40 million by 2030.2 Type 2 diabetes (T2D), which accounts for more than 90% of cases, is a chronic progressive disease characterized by pancreatic β-cell failure, impaired insulin production, insulin resistance, and deteriorating metabolic control.1,3 The downstream consequences of uncontrolled T2D include cardiovascular disease (CVD) and microvascular complications, resulting in substantial morbidity and mortality.4 Overall, diabetes imposes a significant burden on health care resources and costs.5
Glucagon-like peptide-1 receptor agonists (GLP-1RAs) mimic native glucagon-like peptide-1 in stimulating insulin secretion and decreasing glucagon secretion, with both effects occurring in a glucose-dependent manner.6 The approval of the first tablet formulation of a GLP-1RA for the treatment of T2D, oral semaglutide,7 creates a need to revisit the role of this class of therapies in managed care. This manuscript summarizes the impact of T2D in the United States, discusses the positioning of GLP-1RAs in the treatment pathway, explores the roles of therapeutic inertia and adherence in the underutilization of injectable GLP-1RAs, and describes the rationale for an oral GLP-1RA.
The Burden and Economic Impact of T2D in the United States
Diabetes Epidemiology
The National Diabetes Statistics Report from the Centers for Disease Control and Prevention provides estimates of the incidence of diabetes.1 Although the estimates are for diabetes overall, they largely reflect the epidemiology of T2D.1 The age-adjusted incidence of newly diagnosed cases of diabetes in the United States increased from 6.2 per 1000 adults in 2000 to 8.4 per 1000 in 2008, and has since gradually declined.1 As of the latest data (2018), the age-adjusted incidence of diabetes was estimated at 6.7 per 1000 adults, and the crude estimate was 1.5 million new cases a year.1
Despite the decline in the incidence of diabetes in the United States, prevalence remains high but has plateaued since 2009.1,8 Current estimates suggest that 26.9 million adults had diagnosed diabetes in 2018, and an additional 7.3 million adults had undiagnosed diabetes, which together represents 13% of all US adults.1 The high prevalence, despite declining incidence, is likely due to patients living longer following diagnosis, owing to reductions in cardiovascular (CV) morbidity and mortality.8
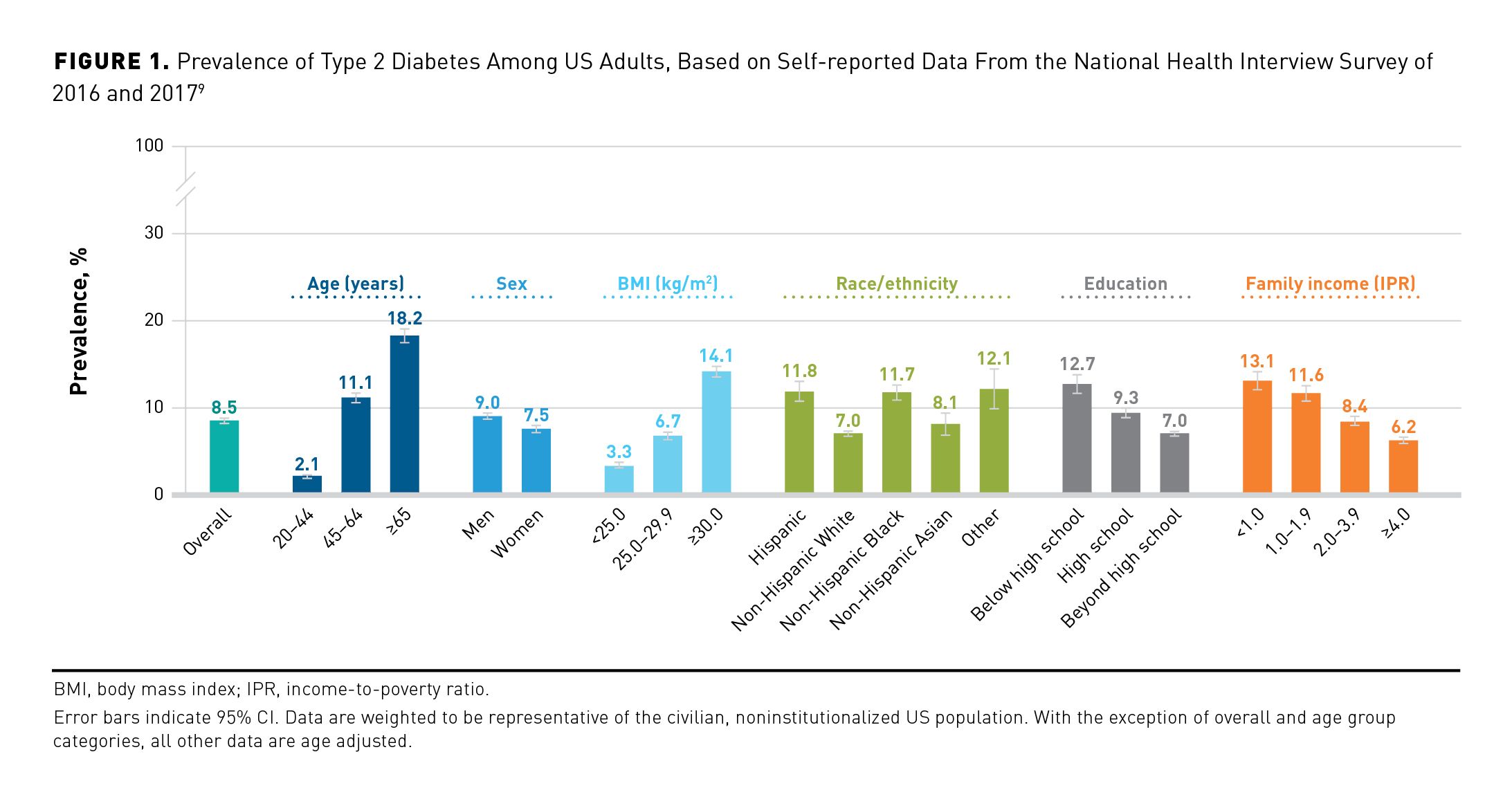
Epidemiological data from more than 58,000 US adults responding to the National Health Interview Survey of 2016 and 2017 indicate that the prevalence of diagnosed T2D (Figure 19): is higher in men than women; increases with age, affecting 18% of those at least 65 years old; increases with body mass index (BMI), affecting 14% of those with a BMI of at least 30 kg/m2; varies according to race/ethnicity; and is higher among those of lower education and income levels.9 In this survey, the prevalence of T2D was found to be higher among non-Hispanic Black and Hispanic populations than among non-Hispanic White or non-Hispanic Asian populations.9
Nearly 90% of adults with diagnosed T2D in the United States were overweight or had obesity (BMI ≥ 25 kg/m2),1 consistent with excess weight being a leading risk factor for T2D.10 Intensive lifestyle programs assisting patients to increase physical activity and reduce caloric intake are important for preventing progression from prediabetes to T2D and improving patient outcomes.11,12
Burden of T2D for Patients
Diabetes approximately doubles the risk of coronary heart disease and ischemic stroke.13 Consequently, CVD is the leading cause of death among patients with T2D,14 as discussed in another article in this supplement.15
Microvascular complications of T2D include chronic kidney disease (CKD), diabetic retinopathy, and diabetic peripheral neuropathy, each of which has the potential to seriously impact patients’ lives.16 CKD can progress to end-stage renal disease (ESRD), the requirement for dialysis, and the need for a kidney transplant.16 Approximately 37% of adults with T2D in the United States are estimated to have mild renal impairment, 18% have moderate-to-severe renal impairment, and less than 1% are estimated to have ESRD.17 Although the prevalence of ESRD among patients with diabetes is low, diabetes is the leading cause of ESRD in the United States, accounting for more than 58,000 new cases in 2017.18 Another complication is diabetic retinopathy, which was reported to affect 8.6% of US adults aged 45 and older with diagnosed diabetes,19 and is a leading cause of new cases of blindness among working-age adults.1,20 In addition, diabetic peripheral neuropathy and peripheral arterial disease can result in foot ulcers, and ultimately amputations.16 In 2016, 130,000 adults with diabetes were hospitalized for lower-extremity amputations.1
T2D is associated with impairment of patients’ health-related quality of life (HRQOL), affecting mental and physical functioning, and social interactions. HRQOL is related to diabetes duration, diabetes-related complications, higher BMI levels, insulin use, and comorbid depression.21-23 Both microvascular and macrovascular complications impact HRQOL in T2D.24,25 CV events were associated with a significant decrease in HRQOL, which was greatest in the initial post-event period.25
Hypoglycemia—episodes of abnormally low blood glucose that are associated with use of insulin or insulin secretagogues such as sulfonylureas—is another key concern in T2D, and can lead to symptoms ranging from tremors, sweating, and confusion, to seizures and death.26 In 2016, there were 235,000 emergency department (ED) visits and 57,000 hospitalizations for hypoglycemia among adults with diabetes in the United States.1 Hypoglycemia was reported to significantly impair both the mental and physical component summary of the Medical Outcomes Study 36-Item Short Form Survey, with severe hypoglycemia (ie, episodes requiring external assistance) having the greatest impact (mental and physical component summaries were 5.6 and 3.6 points lower, respectively, in a survey of patients with T2D and severe hypoglycemia episodes vs those with no hypoglycemia in the prior 3 months [scores can range from 0 to 100; higher indicates better HRQOL]).27 Hypoglycemia can result in greater work impairment,28 and can negatively impact social functioning.27 In the previously mentioned survey, absenteeism and presenteeism (assessed over the preceding 7 days) were 5.7% and 17.7%, respectively, in patients with no hypoglycemia, but were 15.3% and 31.2%, respectively, among patients who experienced severe hypoglycemia in the 3 months prior.27 As a consequence, primarily of microvascular and macrovascular complications,5 diabetes was reported as the seventh most common cause of death in the United States in 2017.1 From 2007 to 2017, diabetes was an underlying or contributing cause of death for 2.7 million US adults, representing 9.6% of all deaths during this period.29
Diabetes also places substantial financial burden on patients. Medical Expenditure Panel Survey data suggest that US patients with diabetes spend $353 more annually on out-of-pocket (OOP) costs than those without diabetes, mostly owing to prescription drug costs.30 Among Medicare beneficiaries at least 65 years old, the presence of diabetes increased OOP costs by $237 per year, representing a 21% increase in OOP spending on health care (including inpatient, outpatient, and prescription drug spending) versus absence of diabetes.31
Burden of Type 2 Diabetes on Health Care Systems
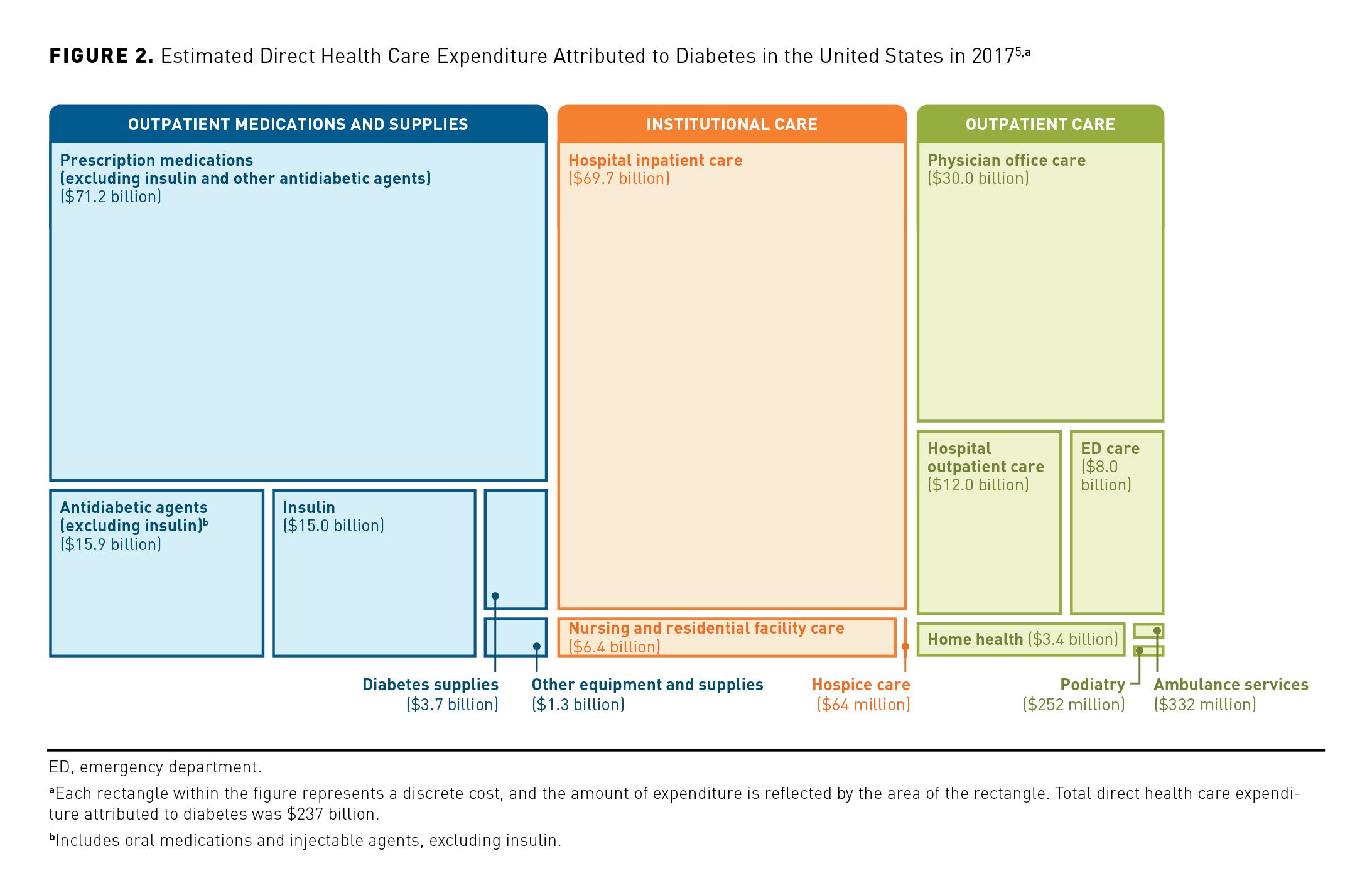
The substantial impact of T2D on patients drives a significant burden for health care systems. The American Diabetes Association (ADA) estimated that the direct medical costs of diabetes in the United States were $237 billion in 2017, representing a 26% increase from 2012.5 Key contributors included hospital inpatient costs ($70 billion), physician office-based care costs ($30 billion), and the cost of outpatient medications attributable to diabetes ($102 billion) (Figure 2).5 In 2016, there were 16 million ED visits among adults with diabetes listed as a diagnosis in the United States, and 7.8 million hospital discharges.1 The economic burden of uncontrolled diabetes is compounded by indirect productivity loss related to work impairment (eg, absenteeism, presenteeism, and inability to work), and lost labor productivity due to premature death.5,32 Estimates from 2017 suggested indirect costs totaling $90 to $250 billion per year,5,32 with the large variation due to differences in the range of indirect costs and analysis methodologies.32
Globally, CVD has been estimated to account for 20% to 49% of the total costs associated with T2D treatment.33 Microvascular complications were reported to increase total annual medical costs by 66% in a managed care setting, compared with those without such complications.34 Furthermore, lost productivity costs in the United States due to diabetes-attributed renal, cerebrovascular, or CV death were estimated to total $11.4 billion in 2017.5
Hypoglycemic episodes increase the cost of T2D, with severe hypoglycemia having the greatest impact, through impaired work productivity, higher health care resource utilization, and more ED visits and hospitalizations (see previous section).27,28 In 2016, 235,000 ED visits (10.2 per 1000 adults with diabetes) were for hypoglycemia.1 A study of patients with T2D experiencing severe episodes of hypoglycemia relative to those without hypoglycemia in the prior 3 months, reported significant increasing trends for the average number of health care professional visits (8.06 vs 5.99 visits), ED visits (0.64 vs 0.29), and hospitalizations (0.41 vs 0.15) over a 6-month period.27 Annual direct health care resource utilization costs among patients who experienced severe hypoglycemia in the prior 3 months were at least twice as much as in those without such events.27 Although non-severe hypoglycemia episodes have little effect on direct health care costs,27 they may increase indirect costs associated with lost work productivity, as demonstrated in 1 study that reported a 33% increase relative to those without hypoglycemia.28
Poor glycemic control in T2D increases the risk of complications and death.4,35,36 The magnitude of the burden of T2D morbidity and mortality on patients and the health care system in the United States underscores the importance of appropriate use of effective therapies to control T2D and minimize the risk of complications—while avoiding hypoglycemia—and reduce health care costs.
The Role of GLP-1RAs in the Treatment Intensification Pathway
Clinical Profile of Injectable GLP-1RAs
Injectable GLP-1RAs have been available for use in the United States for over a decade, with 6 agents developed (1 of which [albiglutide] is no longer available, and 2 of which [exenatide and semaglutide] have 2 formulations available).6 Despite differences in dosing regimens, efficacy, and tolerability among GLP-1RAs,6 collectively they are associated with high glucose-lowering efficacy and weight loss.11,35 Gastrointestinal disorders (such as nausea) are the most commonly reported adverse effects with GLP‑1RAs.6,35 The mechanisms causing such effects are uncertain, but may relate to delayed gastric emptying.37 There is evidence to suggest that semaglutide directly activates areas of the hindbrain and hypothalamus, and indirectly modulates other areas, such as the lateral parabrachial nucleus, involved in regulating appetite and satiety (which also play a role in the weight-reducing effects of GLP-1RAs) and nausea.37,38 Subsequent articles in this supplement explore the efficacy and safety of GLP‑1RAs further, with a focus on oral semaglutide.15,39 In addition, GLP-1RAs have been investigated in CV outcomes trials in patients with T2D, and several are now indicated for the prevention of CV events in adults with T2D and established CVD, as reviewed separately in this supplement.15
A key advantage of GLP-1RAs is their low risk of hypoglycemia (unlike insulin and insulin secretagogues),11,35 arising from their glucose-dependent mechanism of action. GLP‑1RAs stimulate insulin secretion and inhibit glucagon secretion at normal or elevated glucose levels, but not at low glucose levels, allowing glucagon to exert a counterregulatory action and avoid hypoglycemia.6,40
Treatment Guidelines for Type 2 Diabetes
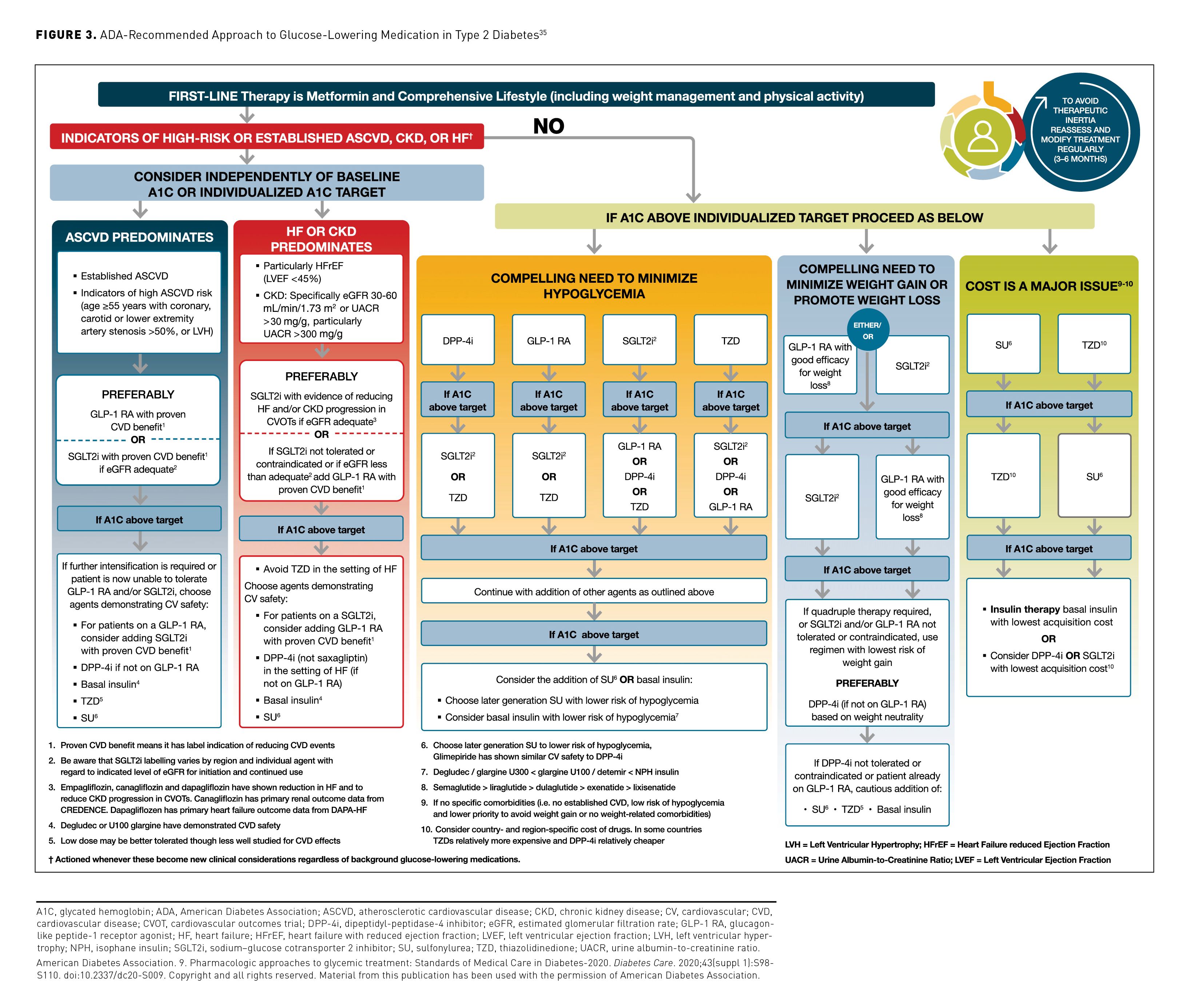
The latest Standards of Medical Care in Diabetes from the ADA and American Association of Clinical Endocrinologists/American College of Endocrinology (AACE/ACE) recommend glycated hemoglobin (A1C) targets less than 7.0% (ADA) or 6.5% or less (AACE/ACE).11,41 After initial lifestyle modification and first-line pharmacotherapy (typically metformin), patients with uncontrolled T2D should receive add-on therapy, with treatment selection dependent on individual circumstances.11,35 Based on ADA Standards of Medical Care (Figure 335), patients without indicators of high-risk or established atherosclerotic CVD (ASCVD), CKD, or heart failure (HF) should receive add-on therapy with:
- a dipeptidyl-peptidase-4 inhibitor (DPP-4i), GLP-1RA, sodium–glucose cotransporter 2 inhibitor (SGLT2i), or thiazolidinedione, if needing to minimize hypoglycemia;
- a GLP-1RA (that has been shown to induce weight loss) or an SGLT2i, if needing to minimize weight gain or promote weight loss; or
- a sulfonylurea or thiazolidinedione, if cost is a concern.35
Patients who have indicators of high-risk or established ASCVD, CKD, or HF should receive one of the following, regardless of their A1C level:
- a GLP-1RA or SGLT2i (if estimated glomerular filtration rate is adequate) with proven CVD benefit if ASCVD predominates; or
- an SGLT2i (that has been shown to reduce HF or CKD progression) if HF or CKD predominate, or a GLP-1RA with proven CVD benefit if an SGLT2i is not appropriate.35
Three injectable GLP-1RAs are indicated for reducing the risk of major adverse CV events in patients with T2D and established CVD (dulaglutide, liraglutide, and semaglutide) or multiple CV risk factors (dulaglutide).15,42-44
The majority (89.0%) of all adults with diabetes in the United States have been reported as overweight (27.6%), having obesity (45.8%) or extreme obesity (15.5%),1 and CVD was estimated to affect 32.2% of patients with T2D.45 Therefore, GLP-1RA therapy is likely to be appropriate for many patients early in their treatment pathway, based on the ADA algorithm.35 The current ADA Standards of Medical Care notes the availability of an oral GLP-1RA (oral semaglutide) and does not differentiate between oral and injectable GLP-1RAs within the overall algorithm for glucose-lowering medication in T2D. In patients with indicators of high-risk or established ASCVD, CKD, or HF, use is based on proven CVD benefit (Figure 3).35
Patients with T2D should be assessed every 3 to 6 months to avoid delays in intensifying treatment, with additional medications added as needed to achieve glycemic control.11,35 Although insulin may ultimately be required for many patients, it has undesirable effects, including increased risk of hypoglycemia and weight gain, and it is typically recommended after other agents.11,35 Of note, the ADA recommends that injectable GLP-1RAs be considered for most patients prior to insulin.35 Insulin initiation should be considered earlier if symptoms of hyperglycemia are present, or if A1C level is higher than 10%; a switch to non-insulin therapies may be possible once the glucotoxicity has been resolved.35 Challenges can arise when real-world care diverges from treatment guidelines, leading to suboptimal patient outcomes, as discussed below.
The Impact of Therapeutic Inertia and Low Adherence in T2D
The Importance of Early Glycemic Control
Early glycemic control after diagnosis is associated with improved long-term outcomes in patients with newly diagnosed T2D, a concept known as metabolic “legacy” or “memory,”4,36 with the legacy effect on the long-term risk of microvascular and macrovascular complications extending beyond the initial period of glycemic control.4,36,41 A large study of more than 30,000 newly diagnosed managed care patients with T2D assessed the legacy effect over the course of 10 years’ follow-up. Patients with A1C levels between 7.0% and less than 8.0% during the first year after diagnosis had significantly greater risk of microvascular complications (HR, 1.39; 95% CI, 1.23-1.58), macrovascular events (HR, 1.29; 95% CI, 1.20-1.38), and death (HR, 1.29; 95% CI, 1.10-1.51), versus those with A1C levels less than 6.5% during the first year.4 However, data from the 2014 National Health and Nutrition Examination Survey suggest that approximately half of patients with diabetes in the United States do not have A1C levels less than 7.0%, and one-third have not achieved individualized A1C targets.46 Potential barriers to early glycemic control include inertia and low patient adherence to treatment regimens.36,47-49 Personal experience also suggests that other barriers encountered include a lack of resources, and as a result, limited time to discuss treatments with each patient.
Inertia
Inertia in T2D relates to lack of timely adherence to guideline recommendations (ie, clinical inertia), and more specifically the failure to intensify or deintensify T2D therapy in a timely manner (ie, therapeutic inertia).50 Such inertia can occur in primary care or specialist settings at any stage of therapy,47 and has been reported within managed care populations in the United States.51 Failure to intensify treatment within 6 months of an A1C level of at least 7% was reported in 63% and 86% of patients with T2D receiving 2 oral glucose-lowering agents in 2 separate US studies.48,52 Furthermore, it was reported that 44% did not receive intensification even after their A1C level reached 9% or higher (Figure 4).48 The time to intensification after an above-target A1C measurement is typically 1 to 5 years in patients treated with more than 1 oral antidiabetic drug.47 Therapeutic inertia was associated with worse glycemic control after 12 months’ follow-up (mean A1C reductions of 0.59% vs 0.25% with and without intensification, respectively; P < .001).52
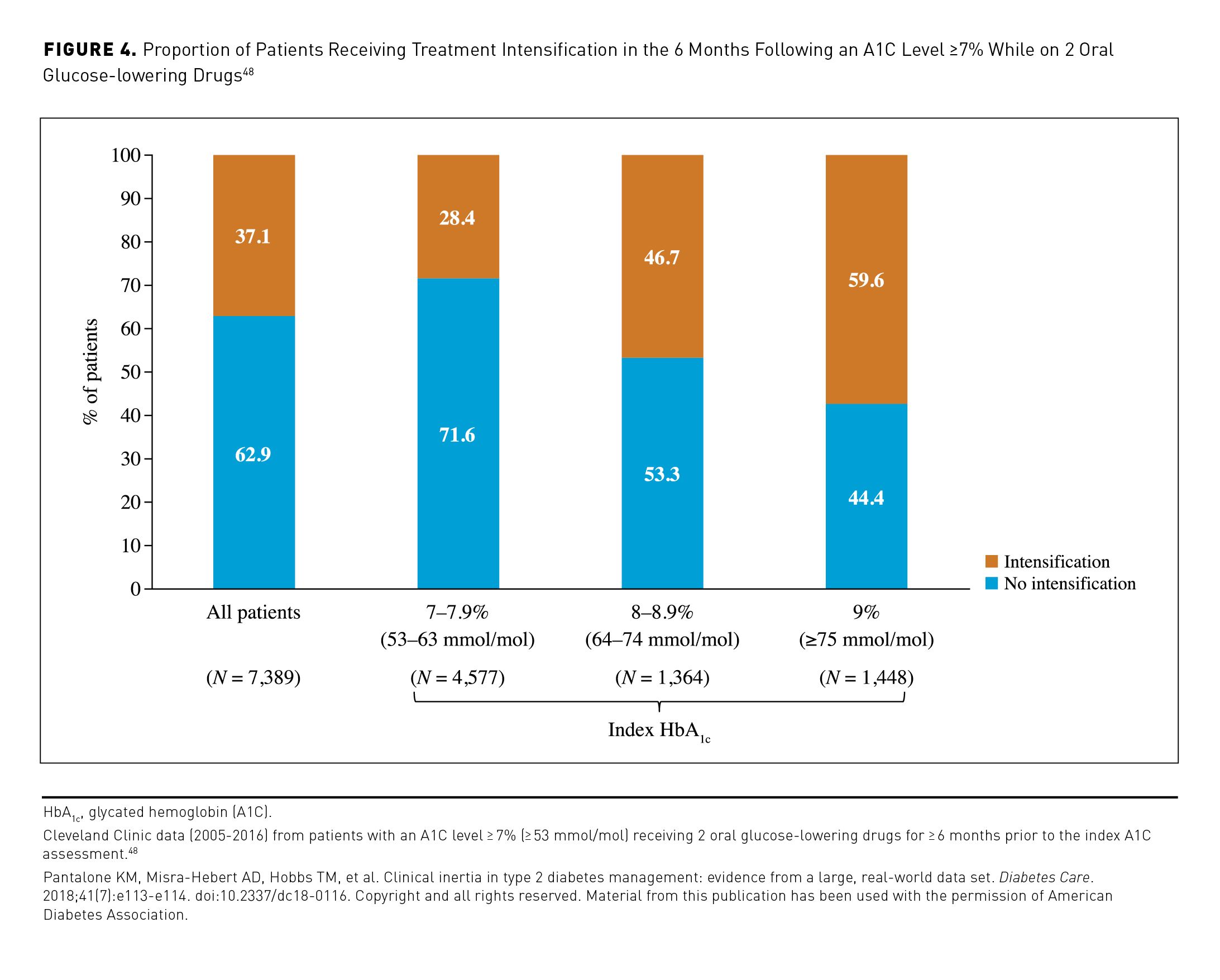
Health economic data suggest that clinical and therapeutic inertia increase economic burden.53,54 Diabetes-related outpatient costs increased by 60% over an 18-month period when ADA guideline recommendations for monitoring and intensification were not followed.54 Modeling analyses suggest that a delay in intensification following an A1C level of 9.0% or higher results in a $1.8- to $14.3-billion increase in diabetes-related complications costs, and $5.6 to $45.9 billion in lost productivity costs over 1 to 5 years.53
Reasons for inertia include patient-related factors (eg, resistance to changes in treatment regimen potentially due to denial, concerns relating to starting injection-based therapies, or cost of treatment) and physician-related factors (eg, lack of time or sufficient support and difficulties in navigating guidelines and algorithms).55,56 Health care system factors causing inertia include medication preauthorization requirements, formulary coverage variation, lack of planning, poor communication between health care providers, failure to adopt multidisciplinary approaches to care, and inadequate patient support or education.55
Clinical inertia with injectable therapy can stem from patient opposition. A study among patients with T2D not currently using insulin therapy found that approximately 30% of them were unwilling to start insulin. The leading barriers included a desire to try all other options first (90% of patients), reluctance to accept that their diabetes had progressed (84%), reluctance to inject in public (43%), and fear of needle pain (39%).57 Failure to transition to injectables in a timely manner can also be due to concerns over cost, adherence to the dosing requirements, and potential overestimation of injection-related pain and fear.47,55,56,58
Patient Adherence
Poor patient adherence (how closely a patient complies with a prescribed treatment regimen) and persistence (how long they continue taking the treatment) to treatment are major challenges in T2D,49 including for injectable therapies such as insulin59 and GLP-1RAs.60 For insulin, adherence rates vary substantially between studies (30%-86%), as reviewed in detail by Guerci et al.59 At 12 months after initiation of 3 injectable GLP-1RAs, a claims analysis reported adherence rates between 32% and 51% and persistence rates ranging from 34% to 55%. A variation in rates potentially arose from differences between agents in dosing regimen convenience, delivery device ease-of-use, effectiveness, and safety.60
Suboptimal adherence and lack of persistence with injectables is associated with poor glycemic control,60,61 and increased health care resource use and medical costs.61 For example, analysis of claims data during 1 year of follow-up showed that adherence versus nonadherence to liraglutide was associated with significantly greater A1C reductions (0.81% vs 0.42%, respectively; P < .001), fewer ER visits (13 vs 18 per 100 patients, respectively; P = .030) and lower diabetes-related medical costs ($2743 vs $4149, respectively; P = .018).61 In a separate database study, persistence with basal insulin was associated with lower diabetes-related medical care costs than nonpersistence ($3239 vs $3667 after 1 year [P = .015] and $3082 vs $3998 after 2 years [P < .01], respectively).62
Factors that influence adherence in T2D include: patients’ perceptions of treatment efficacy; hypoglycemia incidence; treatment convenience/complexity; treatment cost; patient beliefs over treatment risks versus benefits; and patient trust in physicians.63 The route of administration could impact these factors. A survey of US adults prescribed insulin or GLP-1RAs for T2D revealed that across these therapies: 19% to 39% of patients were disappointed when first prescribed an injectable, believing it reflected a personal failure to manage their diabetes; 31% to 52% were nervous about using the injectable correctly; and 4% to 28% felt the injectable medication was being used by their physician as a threat to make the patient take better control of their diabetes.64 In this survey, the most commonly reported barrier to continuing treatment was injection-related concerns, including needle pain (13% of patients), injection nervousness (11%), and needle fear (10%), with injection concerns a contributing factor to discontinuation in 20% of patients who stopped taking the injectable.64
To maximize the potential benefits of GLP-1RAs, overcome inertia, and improve patient adherence in managed care requires a multidisciplinary approach, with nurses, dieticians, behavioral health clinicians, pharmacists, and physicians working in partnership.55 Programs providing diabetes self-management education and support (DSMES) are critical,55,57 and the ADA recommends that payers support such programs to improve patient outcomes and reduce health care costs.12 DSMES efforts should facilitate shared decision-making, positively manage patient expectations of therapy, and incorporate treatment targets that reflect the patient’s personal goals.12,56,57
The Rationale for an Oral GLP-1RA in T2D
GLP-1RAs are relatively underutilized in the United States, accounting for just 7% of second-line prescriptions (after metformin) in 2016, with sulfonylureas (46%), DPP-4is (20%), and insulin (17%) more commonly used.65 This is despite being associated with high glycemic efficacy, weight loss, a neutral effect on hypoglycemia risk, potential CV benefits, and being recognized by the ADA guidelines and AACE/ACE consensus statement for early use in the treatment paradigm following metformin.11,35 The lack of an oral GLP-1RA formulation may have tempered uptake. In addition, there are a variety of agents in this class, each with its own unique profile, dosing device, and administration requirements.6,35 This may have led to a lack of clinician comfort with prescribing these agents due to poor familiarity with product formulation and dosing, place in therapy, cost, and safety. There may also be challenges when resources to support initiation of an injectable are limited.56
Oral semaglutide became the first GLP-1RA to be approved for glycemic control in adults with T2D in September 2019 in the United States, and subsequently in 2020 in the European Union, United Kingdom, and Japan.66-68 A long-term study (SOUL; NCT03914326) is ongoing to assess a potential CV benefit with oral semaglutide. Oral semaglutide aligns with patient preferences for oral administration, avoids the stigma associated with injections, has the potential to alleviate therapeutic inertia, and could lead to earlier use of GLP-1RAs in the treatment paradigm.69 In this context, the subsequent articles in this supplement review the efficacy, safety, and clinical evidence for oral semaglutide, its potential impact on the clinical and economic burden of T2D, and implications for use in the managed care setting.
Acknowledgments
This article was supported by Novo Nordisk Inc; the company was provided with the opportunity to perform a medical accuracy review. Under the direction of the authors, medical writing and editorial support was provided by Nicole Cash of Axis, a division of Spirit Medical Communications Group Limited (funded by Novo Nordisk Inc).
Author affiliations: Jefferson Health (TD); TriHealth Physician Partners (MH).
Funding source: Financial support for this work was provided by Novo Nordisk Inc.
Author disclosures: Dr Dougherty has no relevant financial relationships with commercial interests to disclose. Dr Heile has served as a speaker for and holds stock in Novo Nordisk Inc.
Authorship information: Drafting of the manuscript (TD, MH); critical revision of the manuscript for important intellectual content (TD, MH); responsibility for content (TD, MH).
Address correspondence to: Michael Heile, MD, FAAFP, 6331 Glenway Ave, Cincinnati, OH 45211. Email: Michael_Heile@trihealth.com. Phone: +1 513 389 1400.
References
1. Centers for Disease Control and Prevention. National diabetes statistics report, 2020: estimates of diabetes and its burden in the United States. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; 2020. Accessed April 7, 2020. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
2. Lin J, Thompson TJ, Cheng YJ, et al. Projection of the future diabetes burden in the United States through 2060. Popul Health Metr. 2018;16(1):9. doi:10.1186/s12963-018-0166-4
3. DeFronzo RA, Ferrannini E, Groop L, et al. Type 2 diabetes mellitus. Nat Rev Dis Primers. 2015;1:15019. doi:10.1038/nrdp.2015.19
4. Laiteerapong N, Ham SA, Gao Y, et al. The legacy effect in type 2 diabetes: impact of early glycemic control on future complications (The Diabetes & Aging Study). Diabetes Care. 2019;42(3):416-426. doi:10.2337/dc17-1144
5. American Diabetes Association. Economic costs of diabetes in the U.S. in 2017. Diabetes Care. 2018;41(5):917-928. doi:10.2337/dci18-0007
6. Nauck MA, Meier JJ. Are all GLP-1 agonists equal in the treatment of type 2 diabetes? Eur J Endocrinol. 2019;181(6):R211-R234. doi:10.1530/EJE-19-0566
7. FDA approves first oral GLP-1 treatment for type 2 diabetes. News release. U.S. Food & Drug Administration. September 20, 2019. Accessed April 20, 2020. https://www.fda.gov/news-events/press-announcements/fda-approves-first-oral-glp-1-treatment-type-2-diabetes
8. Benoit SR, Hora I, Albright AL, Gregg EW. New directions in incidence and prevalence of diagnosed diabetes in the USA. BMJ Open Diabetes Res Care. 2019;7(1):e000657. doi:10.1136/bmjdrc-2019-000657
9. Xu G, Liu B, Sun Y, et al. Prevalence of diagnosed type 1 and type 2 diabetes among US adults in 2016 and 2017: population based study. BMJ. 2018;362:k1497. doi:10.1136/bmj.k1497
10. Eckel RH, Kahn SE, Ferrannini E, et al; American Diabetes Association, European Association for the Study of Diabetes. Obesity and type 2 diabetes: what can be unified and what needs to be individualized? Diabetes Care. 2011;34(6):1424-1430. doi:10.2337/dc11-0447
11. Garber AJ, Handelsman Y, Grunberger G, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm - 2020 Executive Summary. Endocr Pract. 2020;26(1):107-139. doi:10.4158/CS-2019-0472
12. American Diabetes Association. 5. Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(suppl 1):S48-S65. doi:10.2337/dc20-S005
13. Emerging Risk Factors Collaboration; Sarwar N, Gao P, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375(9733):2215-2222. doi:10.1016/S0140-6736(10)60484-9
14. American Diabetes Association. 10. Cardiovascular disease and risk management: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(suppl 1):S111-S134. doi:10.2337/dc20-S010
15. Lingvay I, Taddei-Allen P, Dougherty T. Cardiovascular outcomes, safety, and tolerability with oral semaglutide: insights for managed care. Am J Manag Care. 2020;26(suppl 16):S344-S355. doi:10.37765/ajmc.2020.88555
16. American Diabetes Association. 11. Microvascular complications and foot care: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(suppl 1):S135-S151. doi:10.2337/dc20-S011
17. Wang T, Xi Y, Lubwama R, et al. Chronic kidney disease among US adults with type 2 diabetes and cardiovascular diseases: a national estimate of prevalence by KDIGO 2012 classification. Diabetes Metab Syndr. 2019;13(1):612-615. doi:10.1016/j.dsx.2018.11.026
18. United States Renal Data System (USRDS). US renal data system 2019 annual data report: epidemiology of kidney disease in the United States: executive summary. National Institutes of Health, National Institutes of Diabetes and Digestive and Kidney Diseases; 2019. Accessed May 13, 2020. https://www.usrds.org/media/2371/2019-executive-summary.pdf
19. Cha AE, Villarroel MA, Vahratian A. Eye disorders and vision loss among U.S. adults aged 45 and over with diagnosed diabetes, 2016-2017. National Center for Health and Statistics; 2019. NCHS Data Brief, No. 344. Accessed July 15, 2020. https://www.cdc.gov/nchs/data/databriefs/db344-h.pdf
20. International Diabetes Federation. IDF Diabetes Atlas. 9th edition. International Diabetes Federation; 2019. Accessed April 25, 2020. https://www.diabetesatlas.org/en/
21. Trikkalinou A, Papazafiropoulou AK, Melidonis A. Type 2 diabetes and quality of life. World J Diabetes. 2017;8(4):120-129. doi:10.4239/wjd.v8.i4.120
22. Jing X, Chen J, Dong Y, et al. Related factors of quality of life of type 2 diabetes patients: a systematic review and meta-analysis. Health Qual Life Outcomes. 2018;16(1):189. doi:10.1186/s12955-018-1021-9
23. Kamradt M, Krisam J, Kiel M, et al. Health-related quality of life in primary care: which aspects matter in multimorbid patients with type 2 diabetes mellitus in a community setting? PLoS One. 2017;12(1):e0170883. doi:10.1371/journal.pone.0170883
24. Shao H, Yang S, Fonseca V, et al. Estimating quality of life decrements due to diabetes complications in the United States: the Health Utility Index (HUI) diabetes complication equation. Pharmacoeconomics. 2019;37(7):921-929. doi:10.1007/s40273-019-00775-8
25. Briggs AH, Bhatt DL, Scirica BM, et al. Health-related quality-of-life implications of cardiovascular events in individuals with type 2 diabetes mellitus: a subanalysis from the Saxagliptin Assessment of Vascular Outcomes Recorded in Patients with Diabetes Mellitus (SAVOR)-TIMI 53 trial. Diabetes Res Clin Pract. 2017;130:24-33. doi:10.1016/j.diabres.2016.12.019
26. Seaquist ER, Anderson J, Childs B, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care. 2013;36(5):1384-1395. doi:10.2337/dc12-2480
27. Pawaskar M, Iglay K, Witt EA, et al. Impact of the severity of hypoglycemia on health - related quality of life, productivity, resource use, and costs among US patients with type 2 diabetes. J Diabetes Complications. 2018;32(5):451-457. doi:10.1016/j.jdiacomp.2018.01.012
28. Meneghini LF, Lee LK, Gupta S, et al. Association of hypoglycaemia severity with clinical, patient-reported and economic outcomes in US patients with type 2 diabetes using basal insulin. Diabetes Obes Metab. 2018;20(5):1156-1165. doi:10.1111/dom.13208
29. Kim D, Li AA, Cholankeril G, et al. Trends in overall, cardiovascular and cancer-related mortality among individuals with diabetes reported on death certificates in the United States between 2007 and 2017. Diabetologia. 2019;62(7):1185-1194. doi:10.1007/s00125-019-4870-9
30. Hu R, Shi L, Pierre G, et al. Diabetes and medical expenditures among non-institutionalized U.S. adults. Diabetes Res Clin Pract. 2015;108(2):223-234. doi:10.1016/j.diabres.2015.02.016
31. Fong JH. Out-of-pocket health spending among Medicare beneficiaries: which chronic diseases are most costly? PLoS One. 2019;14(9):e0222539. doi:10.1371/journal.pone.0222539
32. Shrestha SS, Honeycutt AA, Yang W, et al. Economic costs attributable to diabetes in each U.S. State. Diabetes Care. 2018;41(12):2526-2534. doi:10.2337/dc18-1179
33. Einarson TR, Acs A, Ludwig C, Panton UH. Economic burden of cardiovascular disease in type 2 diabetes: a systematic review. Value Health. 2018;21(7):881-890. doi:10.1016/j.jval.2017.12.019
34. Pelletier EM, Shim B, Ben-Joseph R, et al. Economic outcomes associated with microvascular complications of type 2 diabetes mellitus: results from a US claims data analysis. Pharmacoeconomics. 2009;27(6):479-490. doi:10.2165/00019053-200927060-00004
35. American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(suppl 1):S98-S110. doi:10.2337/dc20-S009
36. Khunti K, Seidu S. Therapeutic inertia and the legacy of dysglycemia on the microvascular and macrovascular complications of diabetes. Diabetes Care. 2019;42(3):349-351. doi:10.2337/dci18-0030
37. Filippatos TD, Panagiotopoulou TV, Elisaf MS. Adverse effects of GLP-1 receptor agonists. Rev Diabet Stud. 2014;11(3-4):202-230. doi:10.1900/RDS.2014.11.202
38. Gabery S, Salinas CG, Paulsen SJ, et al. Semaglutide lowers body weight in rodents via distributed neural pathways. JCI Insight. 2020;5(6):e133429. doi:10.1172/jci.insight.133429
39. Rodbard HW, Dougherty T, Taddei-Allen P. Efficacy of oral semaglutide: overview of the PIONEER clinical trial program and implications for managed care. Am J Manag Care. 2020;26(suppl 16):S335-S343. doi:10.37765/ajmc.2020.88554
40. Ahrén B. Glucagon-like peptide-1 receptor agonists for type 2 diabetes: a rational drug development. J Diabetes Investig. 2019;10(2):196-201. doi:10.1111/jdi.12911
41. American Diabetes Association. 6. Glycemic targets: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(suppl 1):S66-S76. doi:10.2337/dc20-S006
42. Ozempic. Prescribing information. Novo Nordisk Inc; 2020. Accessed April 31, 2020. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/209637s003lbl.pdf
43. Trulicity. Prescribing information. Eli Lilly & Co; 2020. Accessed April 13, 2020. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/125469s033lbl.pdf
44. Victoza. Prescribing information. Novo Nordisk Inc; 2019. Accessed April 13, 2020. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/022341s031lbl.pdf
45. Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol. 2018;17(1):83. doi:10.1186/s12933-018-0728-6
46. Carls G, Huynh J, Tuttle E, et al. Achievement of glycated hemoglobin goals in the US remains unchanged through 2014. Diabetes Ther. 2017;8(4):863-873. doi:10.1007/s13300-017-0280-5
47. Khunti K, Gomes MB, Pocock S, et al. Therapeutic inertia in the treatment of hyperglycaemia in patients with type 2 diabetes: a systematic review. Diabetes Obes Metab. 2018;20(2):427-437. doi:10.1111/dom.13088
48. Pantalone KM, Misra-Hebert AD, Hobbs TM, et al. Clinical inertia in type 2 diabetes management: evidence from a large, real-world data set. Diabetes Care. 2018;41(7):e113-e114. doi:10.2337/dc18-0116
49. McGovern A, Tippu Z, Hinton W, et al. Comparison of medication adherence and persistence in type 2 diabetes: a systematic review and meta-analysis. Diabetes Obes Metab. 2018;20(4):1040-1043. doi:10.1111/dom.13160
50. Khunti K, Davies MJ. Clinical inertia – time to reappraise the terminology? Prim Care Diabetes. 2017;11(2):105-106. doi:10.1016/j.pcd.2017.01.007
51. Ruiz-Negrón N, Wander C, McAdam-Marx C, et al. Factors associated with diabetes-related clinical inertia in a managed care population and its effect on hemoglobin A1c goal attainment: a claims-based analysis. J Manag Care Spec Pharm. 2019;25(3):304-313. doi:10.18553/jmcp.2019.25.3.304
52. Buysman EK, Fan T, Blauer-Peterson C, Miller-Wilson LA. Glycaemic impact of treatment intensification in patients with type 2 diabetes uncontrolled with oral antidiabetes drugs or basal insulin. Endocrinol Diabetes Metab. 2018;1(3):e00019. doi:10.1002/edm2.19
53. Ali SN, Dang-Tan T, Valentine WJ, Hansen BB. Evaluation of the clinical and economic burden of poor glycemic control associated with therapeutic inertia in patients with type 2 diabetes in the United States. Adv Ther. 2020;37(2):869-882. doi:10.1007/s12325-019-01199-8
54. Mehta RR, Edwards AM, Rajpathak S, et al Effects of conformance to type 2 diabetes guidelines on health care resource utilization, clinical outcomes, and cost: a retrospective claims analysis. J Clin Transl Endocrinol. 2020;19:100215. doi:10.1016/j.jcte.2020.100215
55. Okemah J, Peng J, Quiñones M. Addressing clinical inertia in type 2 diabetes mellitus: a review. Adv Ther. 2018;35(11):1735-1745. doi:10.1007/s12325-018-0819-5
56. Santos Cavaiola T, Kiriakov Y, Reid T. Primary care management of patients with type 2 diabetes: overcoming inertia and advancing therapy with the use of injectables. Clin Ther. 2019;41(2):352-367. doi:10.1016/j.clinthera.2018.11.015
57. Allen NA, Zagarins SE, Feinberg RG, Welch G. Treating psychological insulin resistance in type 2 diabetes. J Clin Transl Endocrinol. 2016;7:1-6. doi:10.1016/j.jcte.2016.11.005
58. Yoshioka N, Ishii H, Tajima N, Iwamoto Y; DAWN Japan group. Differences in physician and patient perceptions about insulin therapy for management of type 2 diabetes: the DAWN Japan study. Curr Med Res Opin. 2014;30(2):177-183. doi:10.1185/03007995.2013.855187
59. Guerci B, Chanan N, Kaur S, Jasso-Mosqueda JG, Lew E. Lack of treatment persistence and treatment nonadherence as barriers to glycaemic control in patients with type 2 diabetes. Diabetes Ther. 2019;10(2):437-449. doi:10.1007/s13300-019-0590-x
60. Mody R, Huang Q, Yu M, et al. Adherence, persistence, glycaemic control and costs among patients with type 2 diabetes initiating dulaglutide compared with liraglutide or exenatide once weekly at 12-month follow-up in a real-world setting in the United States. Diabetes Obes Metab. 2019;21(4):920-929. doi:10.1111/dom.13603
61. Buysman EK, Liu F, Hammer M, Langer J. Impact of medication adherence and persistence on clinical and economic outcomes in patients with type 2 diabetes treated with liraglutide: a retrospective cohort study. Adv Ther. 2015;32(4):341-355. doi:10.1007/s12325-015-0199-z
62. Kalirai S, Duan R, Liu D, Reed BL. Economic impact of treatment duration and persistence with basal insulin in previously insulin-naive users. J Manag Care Spec Pharm. 2017;23(3):327-336. doi:10.18553/jmcp.2017.23.3.327
63. Polonsky WH, Henry RR. Poor medication adherence in type 2 diabetes: recognizing the scope of the problem and its key contributors. Patient Prefer Adherence. 2016;10:1299-1307. doi:10.2147/PPA.S106821
64. Spain CV, Wright JJ, Hahn RM, et al. Self-reported barriers to adherence and persistence to treatment with injectable medications for type 2 diabetes. Clin Ther. 2016;38(7):1653-1664.e1. doi:10.1016/j.clinthera.2016.05.009
65. Montvida O, Shaw J, Atherton JJ, Stringer F, Paul SK. Long-term trends in antidiabetes drug usage in the U.S.: real-world evidence in patients newly diagnosed with type 2 diabetes. Diabetes Care. 2018;41(1):69-78. doi:10.2337/dc17-1414
66. Rybelsus. Prescribing information. Novo Nordisk Inc; 2020. Accessed April 13, 2020. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/213182s000,213051s001lbl.pdf
67. Rybelsus. Annex I: summary of product characteristics. Novo Nordisk Inc; 2020. Accessed June 13, 2020. https://www.ema.europa.eu/en/documents/product-information/rybelsus-epar-product-information_en.pdf
68. Rybelsus approved in Japan for the treatment of type 2 diabetes. Company announcement. Novo Nordisk Inc. June 29, 2020. Accessed July 22, 2020.
https://ml-eu.globenewswire.com/Resource/Download/46a404a8-4e2b-41d5-a5fa-fa36cfae964f
69. Bucheit JD, Pamulapati LG, Carter N, et al. Oral semaglutide: a review of the first oral glucagon-like peptide 1 receptor agonist. Diabetes Technol Ther. 2020;22(1):10-18. doi:10.1089/dia.2019.0185