- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Top GLP-1 Agonists Balance Weight Loss Efficacy, Safety
For this review, the authors searched for randomized controlled trials published in MEDLINE, Embase, and Cochrane CENTRAL from inception through October 4, 2024.
Retatrutide, tirzepatide, and semaglutide—3 glucagon-like peptide-1 receptor agonists (GLP-1 RAs) or coagonists—came out on top of a new investigation that evaluated the efficacy and safety of 12 of the agents for weight loss among adults classified as overweight or obese and who did not have diabetes. Randomized controlled trials (RCTs) of each of these 3 drugs showed they were the top producers of body weight reduction compared with placebo, according to findings published online today in Annals of Internal Medicine.1
Accounting for 15,491 participants with overweight or obesity and 26 RCTs (23 studied subcutaneous formulations and 3, oral), only 1 included trial had a high risk of bias. The authors’ study population comprised 72% female patients, and their baseline mean body mass index (BMI) ranged from 30 kg/m2 to 41 kg/m2. The mean patient age ranged between 34 and 57 years. Of the agents commercially available for use for long-term weight management, trials of liraglutide accounted for the most patients (n = 3510), followed by semaglutide (n = 3247) and tirzepatide (n = 1896). The remaining 9 agents are primarily investigative: survodutide (n = 345), JNJ-64565111 (n = 295), beinaglutide (n = 286), retatrutide (n = 268), efpeglenatide (n = 235), orforglipron (n = 222), noiiglutide (n = 192), mazdutide (n = 186), and exenatide (n = 114); 4695 patients received a placebo. Exenatide is approved to treat type 2 diabetes in combination with diet and exercise.1,2
Safety results of this review are notable, in that few deaths were reported and most common AEs were GI related and transient. | Image Credit: © designua-stock.adobe.com
The primary study outcome was change in relative or absolute body weight from baseline to maximum follow-up, and secondary outcomes were changes in BMI, waist circumference, systolic blood pressure (SBP), and diastolic blood pressure (DBP), also from baseline to maximum follow-up.1 The median treatment period was 43 (range, 16-104) weeks.
At baseline, the following additional ranges were seen:
- Body weight: 87 to 115 kg
- Waist circumference: 102 to 121 cm
- SBP: 116 to 132 mm Hg
- DBP: 76 to 84 mm Hg
Agent-Related Weight Reduction vs Placebo
For the commercially available agents, a 15-mg dose of tirzepatide produced a 17.8% (95% CI, 16.3%-19.3%) weight loss vs 13.9% (95% CI, 11.0%-16.7%) with 2.4-mg subcutaneous semaglutide, 12.7% (95% CI, 11.3%-14.2%) with 50-mg oral semaglutide, and 5.8% (95% CI, 3.6%-8.0%) with liraglutide. Retatrutide produced the top 3 results among the investigative agents, leading to a 24.2% (95% CI, 21.8%-26.6%) weight loss at a dose of 12 mg weekly, a 23.9% (95% CI, 20.9%-26.8%) weight loss at a dose of 8 mg that was uptitrated quickly, and a 21.7% (95% CI, 19.0%-24.5%) weight loss at a standard dose of 8 mg weekly.
Among both groups, the shortest treatment duration was 16 weeks for liraglutide and beinaglutide, and the longest treatment duration was 104 weeks for semaglutide.
Risk and Safety
All of the evaluated agents were linked to decreases in BMI, waist circumference, and BP. Half of the trials included in the review reported changes to BMI, 19 demonstrated changes waist circumference, 19 trials showed improved SBP, and 18 trials showed improved DBP.
Few deaths were reported. There was 1 death each in trials of 3.0-mg liraglutide, 0.05- to 0.4-mg semaglutide, 2.4-mg semaglutide, and 1- to 12-mg retatrutide; 2 each in trials of 2.4-mg semaglutide; and 7 in a tirzepatide trial that evaluated doses ranging from 5 to 15 mg. There were low rates overall of serious adverse events (AEs; 0.0%-11.8%) and AEs necessitating treatment discontinuation (0.0%-26.1%).
The most common AEs were gastrointestinal (GI) related, and they included nausea, diarrhea, constipation, and vomiting. These were typically transient and classified as mild or moderate. Among the trials reporting them, rare AEs were pancreatitis (less than 2%), severe GI and biliary disorders (3.5% or less), and psychiatric disorders (15% or less), including insomnia and mood alterations.
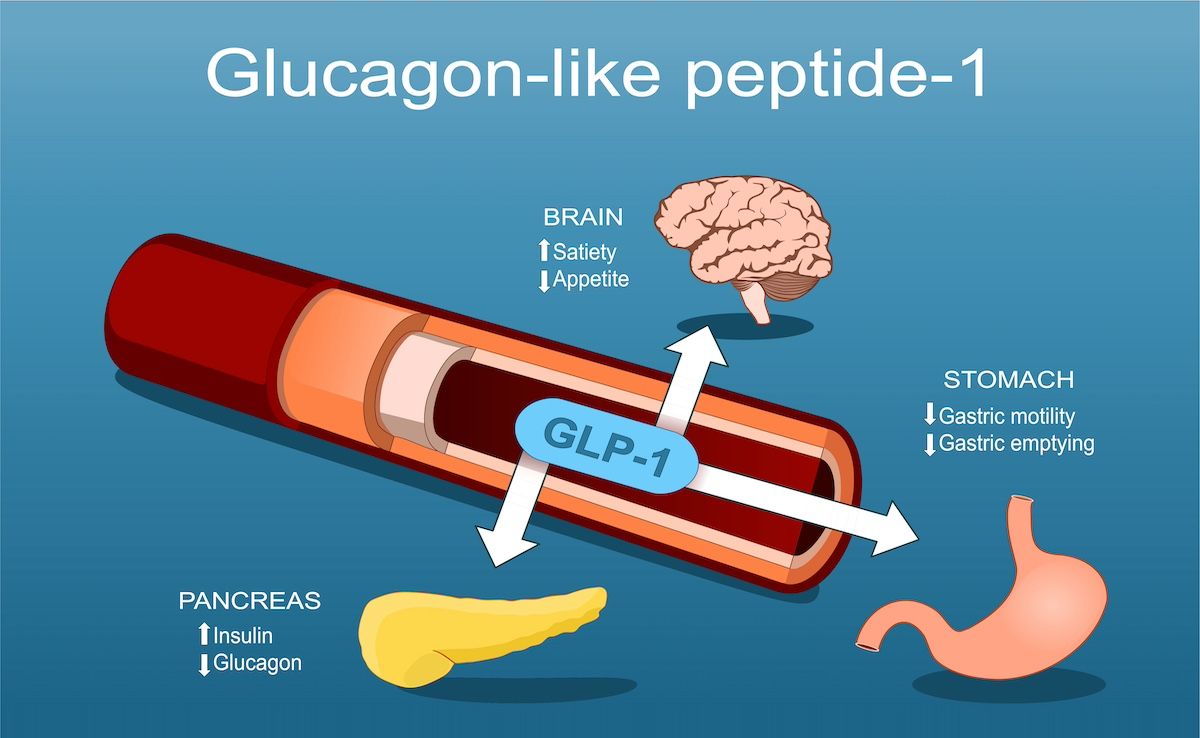
The investigators explained that GLP-1 RAs exert their changes via 3 principal mechanisms of action: they reduce appetite and increase satiety via the hypothalamus, slow gastric emptying, and enhance insulin regulation.3,4
Strengths of these findings are that the authors’ analyses did not include patients with comorbidities, namely metabolic disorders or cardiovascular disease.1 This population was considered healthy overall, besides the individuals having overweight or obesity.
Ongoing concerns associated with GLP-1 RA use are the potential for weight gain after stopping treatment and long-term adherence due to AEs—although the investigators noted that the most common GI AEs tend to diminish with longer use and are more pronounced during initial treatment.
References
1. Moiz A, Filion KB, Toutounchi H, et al. Efficacy and safety of glucagon-like peptide-1 receptor agonists for weight loss among adults without diabetes. Ann Intern Med. Published online January 6, 2025. Accessed January 6, 2025. doi:10.7326/ANNALS-24-01590
2. Exenatide (subcutaneous route). Mayo Clinic. Accessed January 6, 2025. https://www.mayoclinic.org/drugs-supplements/exenatide-subcutaneous-route/description/drg-20068401
3. Campbell JE, Drucker DJ. Pharmacology, physiology, and mechanisms of incretin hormone action. Cell Metab. 2013;17(6):819-837. doi:10.1016/j.cmet.2013.04.008
4. Drucker DJ. Mechanisms of action and therapeutic application of glucagon-like peptide-1. Cell Metab. 2018;27(4):740-756. doi:10.1016/j.cmet.2018.03.001
