- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Too Much, Too Fast: Providers Need More Time to Operationalize Medicare's New Radiation Oncology Model
CMS' new radiation oncology payment model is slated to begin on January 1, 2020, but the significant billing changes that the model requires will require more time.
This article was coauthored by Hannah Alphs Jackson, MD, MHSA, director of value-based care and assistant professor of surgery at Northwester Medicine.
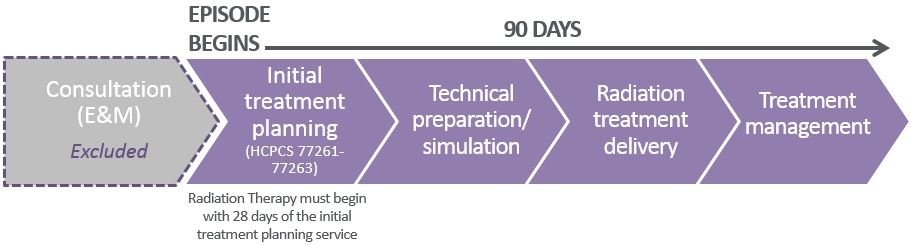
On July 10, 2019, CMS announced a new proposed mandatory payment model called the Radiation Oncology (RO) Model. The RO Model would establish a site-neutral prospective bundled payment for 90-day episodes of care for radiation therapy. Unlike other popular CMS bundled payment programs, such as the Oncology Care Model (OCM) and Bundled Payments for Care Improvement (BPCI), the RO Model will only include payments for services directly linked to radiation therapy while excluding payments for hospitalizations and post-acute services (Figure).
Figure: RO Model “Episode”
CMS explains in its proposed rule that the RO Model is designed to test whether a prospective payment model can incentivize the provision of high-value care—in this case, incentivizing the delivery of a shorter course of radiation therapy treatment with more radiation per fraction when clinically appropriate.
The RO Model is slated to start on January 1, 2020, with a potential delay to April 1, 2020. While designing a prospective bundled payment model is a considerable undertaking, implementing such a model is an entirely different ball game. Many commenters have called for a delay to the start date to allow providers to complete the necessary tasks required by many models, such as engaging clinical and operational stakeholders, analyzing data for improvement opportunities, hiring new staff, etc.
As a prospective payment model, the RO Model also includes significant billing changes. This article explores the time and process required to operationalize a prospective billing model, and ultimately shows that neither the January 2020 nor April 2020 start dates provide participants with sufficient time to complete the build.
Summary of New Billing Requirements
RO Model participants are required to bill 2 new Healthcare Common Procedure Coding System (HCPCS) codes that correlate to the prospective payments associated with the professional and technical components of care: (1) when a treatment planning service has been furnished and (2) when treatment has been delivered.
It’s important to note that, in many instances, 2 different entities will submit these 2 separate codes. “Professional participants” (a physician group practice of whom the treating radiation oncologist is a member) will bill the first code while “technical participants,” such as hospital outpatient departments or freestanding centers, will bill the second code. Only in instances in which both the professional and technical components are furnished through a freestanding radiation therapyRT center (“dual participant”) would one entity bill both codes.
Finally, CMS also requires participants to bill pre-existing HCPCS codes associated with radiation therapy with no-pay amounts throughout the entirety of the 90-day episode. This requirement will allow CMS to monitor utilization under the model.
The Process to Operationalize New Billing Requirements
While the process may vary slightly across organizations, most will have to undertake a similar process in order to operationalize these new proposed billing requirements. We estimate that the process could take 6 to 9 months to successfully implement. At a high level, the process includes the following steps (which has been taken directly from Northwestern Medicine [NM]’s comments to CMS):
- Establish front-end process to identify patients and claims for whom and to which the billing methodology must be applied.
- Build logic in Epic to appropriately bundle visits for all treatment plans to ensure accurate tracking and billing.
- Build logic in Epic to drop new prospective HCPCS codes.
- Build logic to zero out existing HCPCS codes.
- Establish back-end process for updating and posting zeroed out HCPCS codes.
At NM, claims are generated from an automatic field from the Epic Accounts Receivable (AR) System. Thus, in order to submit a zero-dollar claim, charges must be entered as $0 in the AR System. However, doing so would wreak havoc on internal cost tracking as items listed as $0 in the AR System would also be seen as $0 in internal cost accounting. Correcting these entries to ensure accurate budgets, profit and loss statements, and other financial documents would be extremely burdensome.
NM has identified one potential solution to avoid this back-end work: permit the original HCPCS payments to be listed in the “non-covered charges” claim column, while $0 would be entered in the “covered charges” column. This information, along with detailed billing instructions (type of claim form, necessary claim lines, etc), will hopefully be included in the final rule.
Additional Challenges
The following issues further complicate the operationalization of the proposed billing process (partially taken from NM’s comments to CMS):
- Coordination between technical and professional participants: In order to ensure that the appropriate codes are submitted with no-pay amounts, professional and technical participants must coordinate their processes. For example, if radiation therapy is first administered on day five of an episode, the technical participant’s billing team must know to only zero out claims for the subsequent 85 days. This unique logic must be established for each patient.
- Use of third-party billing companies: Many providers and health systems rely on external third-party vendors to complete their billing. RO Model participants will require time to determine how to best partner with these entities to ensure appropriate billing.
Conclusion
NM believes that, when done right, alternative payment models can help further incentivize the efficient delivery of high-quality care. In order for APMs to be successful, providers require sufficient time for planning and implementation. APMs featuring prospective payment carry a unique time-intensive challenges.
If CMS wants providers to execute a new billing system, it must give them the time to do so. At a minimum, the RO Model start date should be pushed back to October 1, 2020.
