
- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
The Role of Managed Care Professionals in the Management of Neovascular Age-Related Macular Degeneration and Diabetic Macular Edema
To claim CE credit for this activity, please visit
http://www.pharmacytimes.org/AMD-DME-suppl
ABSTRACT
Managed care professionals play a significant role in the management of neovascular age-related macular degeneration (nAMD) and diabetic macular edema (DME) through formulary management and drug utilization strategies. These strategies are designed to improve access to affordable care and minimize medical costs to both patients and payers. Preserving vision in patients with nAMD and DME is key to improving clinical outcomes and reducing the risk of comorbid conditions, such as depression. With the approval of new intravitreal treatment options, managed care professionals must stay up to date with evidence-based guidelines as well as the addition of cost-effective treatments to drug formularies to better manage health care resources and improve patient outcomes.
Am J Manag Care. 2023;29(suppl 6):S90-S95. https://doi.org/10.37765/ajmc.2023.89385
Introduction
Age-related macular degeneration (AMD) occurs when a part of the retina called the macula degenerates with age. AMD can either be classified as dry or wet. The dry form is associated with fat-like deposits under the macula, whereas the wet form is caused by the growth of new, atypical blood vessels beneath the retina.1 The latter is commonly referred to as neovascular AMD (nAMD) and is responsible for approximately 90% of blindness among people with AMD.2 Diabetic macular edema (DME) is a vision-threatening condition that occurs when blood vessels in the retina leak fluid into the macula.3
The burden of nAMD and DME is significant for patients, payers, and society.4 Decreases in visual acuity (VA), health-related quality of life (QOL), and work productivity are known patient burdens. As visual function declines, independence and the ability to perform basic everyday tasks lessens, which negatively influences mental health.5 The consequences associated with nAMD and DME have a substantial bearing on economic- and patient-related outcomes, which results in considerable use of health care resources.6,7
Prevalence
Understanding AMD and DME populations is key to evaluate disease burden and the resources required to meet patients’ needs. An estimated 20 million people in the United States are living with some form of AMD.2 Because aging is the greatest risk factor, the prevalence of AMD has been increasing in recent years, and this trend is expected to continue.8 The prevalence of DME is increasing as well. In a cross-sectional study utilizing Medicare and Medicaid claims from 2009 to 2018, the prevalence of DME in adults increased significantly from 1.0% to 3.3%.9 Though often thought of as a disease associated with older age, DME is also prevalent in adults aged younger than 65 years. In a 10-year retrospective claims review of the IBM MarketScan Database, adults with diabetes aged 18 to 64 years were evaluated to determine trends in prevalence and treatment of DME in the United States. The annual prevalence of people living with diabetes who had any form of DME increased significantly from 0.7% in 2009 to 2.7% in 2018.10 During the same period, the annual prevalence of patients with DME who received anti-vascular endothelial growth factor (VEGF) intravitreal injections increased significantly from 8% to 34%.10 Taken together, the prevalence rates of AMD and DME are rising in the general adult population, and simulation analyses project this trend to continue over the next 20 years.8,11 It is vital that managed care professionals are aware of population-based analyses to ensure available resources are benefiting the maximum number of people with vision-threatening eye disease.
Cost Burden
The cost of vision-threatening eye disease is significant. The reported mean annual cost of treating patients with nAMD is approximately $24,520, and 63.5% of those costs are related to outpatient care. Annual costs are driven primarily by anti-VEGF treatments and injection frequency, which increase with disease severity.12 In a 2016 study that evaluated the annual societal costs of patients with nAMD, investigators observed a significant cost difference in patients who had nAMD ($39,910) compared with those who did not ($6116). Patients with no light perception incurred mean annual costs exceeding $82,000, which revealed a strong relationship between worsening disease and increased societal ophthalmic costs.13
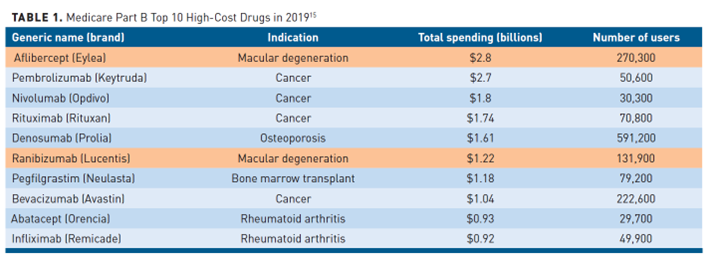
The use of anti-VEGF treatments for vision-threatening eye disease continues to increase. Among privately insured and Medicare Advantage enrollees from 2006 to 2015, the most used anti-VEGF agents to treat various forms of ophthalmic disease were bevacizumab, ranibizumab, and aflibercept. Nearly 80% of anti-VEGF injections were used to treat AMD and diabetic retinal diseases, including DME.14 With numerous biosimilar products poised to enter the US market, these numbers are anticipated to change. Despite their overall efficacy, anti-VEGF treatments are expensive (Table 1).15 In 2020, the global anti-VEGF market for ophthalmic diseases was valued at more than $7 billion, and it is projected to exceed $11 billion by 2026. Anti-VEGF injections rank among Medicare’s costliest drugs, with fee-for-service spending surpassing $5.2 billion in 2019.16 Bevacizumab is frequently cited as the most-used anti-VEGF medication to treat retinal diseases, which is likely related to cost.14,17 The average cost of bevacizumab to treat nAMD and DME is approximately $70 per dose, while the average sales price for aflibercept and ranibizumab in 2019 was $1877 and $1717 per dose, respectively.16
Additionally, there is geographic variation regarding the rate of intravitreal injections across all 50 US states. For example, the mean rate of injections in 2013 for Medicare beneficiaries aged 65 years and older was 19 per 1000. Wyoming had the lowest rate at 4 per 1000 beneficiaries, and the highest rate was observed in Utah at 28 per 1000, a 7-fold difference.17 The study investigators noted a significant correlation between the rate of intravitreal injections and the cost per injection (R = 0.49; P <.001), which suggests that states with higher injection rates were more likely to use higher-cost anti-VEGF therapies. The reasons for geographic variation in the rate of injections administered and the cost per injection are likely multifactorial and may be related to the supply of ophthalmologists who perform the procedure, inconsistent availability of repackaged or compounded bevacizumab, financial incentives to utilize specific agents, and physician or patient preference.17
Quality of Life
Understanding QOL outcomes is an integral part of the management of patients with vision-threatening eye disease. Long-term maintenance of driving vision is a key QOL outcome for patients with nAMD and DME and requires an understanding of real-world treatment patterns, clinical effects of anti-VEGF therapy, and VA assessments. Most US states require a minimum Snellen VA score of 20/40 in the better-seeing eye to obtain an unrestricted individual driver’s license; a minimum score of 20/40 in both eyes is required for a commercial driver’s license in all but 3 US states.18 A 2021 retrospective analysis characterized the likelihood of maintaining driving vision over 4 years after initiating anti-VEGF treatments in patients with nAMD and DME. After 4 years, 73% and 61% of patients with DME or nAMD, respectively, had maintained driving vision. Patients who received 9 or more injections in year 1 had a 38% (nAMD) and 44% (DME) decreased risk of losing driving vision at 4 years compared with those receiving 6 injections or fewer, which suggests the number of injections in year 1 predict long-term driving vision maintenance.19 According to results from the American Society of Retina Specialists (ASRS) survey, the greatest unmet needs in patients with nAMD and DME are pharmacologic agents with improved durability and decreased overall treatment burden.20 The ranibizumab port delivery system showed potential as a once-every-24-week treatment option to reduce treatment burden, but the drug was voluntarily recalled in 2022 due to a failed seal on the refillable system.21
The management of patients with nAMD and DME is costly financially, and the provision of high-quality care also demands a significant amount of time from physicians, staff, patients, and caregivers. The average duration of a patient’s health care visit for the treatment of nAMD is 90 minutes, but it can exceed 4 hours. However, the burden is even more significant when factoring in costs such as patient and caregiver time. Patients report the average time commitment for an nAMD appointment requiring an intravitreal injection to be 11.7 hours, which includes preappointment preparation (16 minutes), waiting time (37 minutes), treatment (43 minutes), travel (66 minutes), and post-injection recovery (average, 9 hours).22
A recent study further evaluated the cost of travel to retinal clinics as well as patient and caregiver time spent in transit. A 3-year cost-savings analysis compared the use of faricimab-svoa, aflibercept, and ranibizumab for the treatment of AMD.23 Medication costs were estimated utilizing wholesale acquisition cost. The frequency of injections was derived from product labeling, which included 12 injections per year for ranibizumab and 8 injections for aflibercept in year 1 followed by 6.5 injections per year in years 2 and 3. Because the administration frequency of faricimab-svoa allows for a flexible dosing schedule, study investigators weighted the number of injections per year as 6.79 injections in year 1 followed by 4.02 injections per year in years 2 and 3. The study used the following proxies to estimate transportation costs and patient/caregiver time spent for clinic appointments: $0.58 for each mile driven (Veterans Affairs reimbursement rate for qualified patients) and $15 per hour (federal minimum wage). Based on projected injection frequency over 3 years and wholesale acquisition cost, faricimab-svoa was determined to be less expensive than aflibercept and ranibizumab by $6359 and $37,709, respectively. When taking drug cost, travel distance, and patient/caregiver time into consideration, the total cost of care for each intravitreal injection was $72,079 for ranibizumab, $39,946 for aflibercept, and $33,265 for faricimab-svoa.23 These results suggest that long-acting intravitreal therapies have a significant impact on total cost of care. When making individual patient decisions, providers and payers may need to take into consideration travel-related indirect costs that patients and caregivers incur.
Some limitations to this study should be noted. Because this study is a theoretical evaluation of drug costs related to patients’ time and travel, estimations of nominal costs and assumptions of time and travel were utilized rather than cost and claims data. As a result, it may be difficult to apply the cost calculations used in the study across all health systems. This study also used FDA-approved on-label dosing regimens to compare aflibercept, ranibizumab, and faricimab-svoa.Additional studies exploring the impact of real-world anti-VEGF dosing regimens are needed to further understand the potential cost differences among these therapies.
Optimizing Patient Outcomes
The patient-specific selection of an anti-VEGF therapy should not be based on cost alone. There is often significant interpatient variability in treatment response to anti-VEGF therapies, which is dependent on a variety of factors, including the patient’s age, VA, lesion characteristics, and lesion duration.24 The selection of treatment is made even more complex by insurance mandates and the number of different anti-VEGF treatments with diverse pharmacokinetic profiles.20
In addition, there has been the recent emergence of biosimilars. As managed care organizations consider biosimilars for their drug formularies, there is a need to evaluate their interchangeability. An ophthalmic biosimilar is considered interchangeable if it elicits the same clinical result as its reference product and can be switched back and forth with no adverse effects. Ranibizumab-eqrn is currently the only biosimilar deemed interchangeable for DME and nAMD, which allows substitution without intervention by the prescribing clinician, subject to state pharmacy laws.
The American Academy of Ophthalmology (AAO) recently expressed caution about the use of bevacizumab-bvzr and bevacizumab-awwb for ophthalmic conditions. Both biosimilars are used in the oncology space, and select payers were including these on formularies, suggesting they may be used for ophthalmic conditions. However, neither biosimilar has been studied for ophthalmic conditions, and not all of their inactive ingredients have been adequately evaluated for use in the eye. The AAO recognizes the value biosimilars bring to society but maintains the stance that sufficient safety and efficacy data must emerge before these agents are routinely recommended for ophthalmic use.25 Taken together, it is important to have a comprehensive drug formulary that allows retina specialists to tailor treatment to meet individual patient needs.
Bevacizumab is often used as first-line treatment for vision-threatening eye disease, but drug preference varies among patients and retina specialists.17,26,27 In addition, there is currently no standard regimen for injection frequency. To optimize patient compliance and reduce costs, various flexible-dosing strategies are used in clinical practice. In the as-needed (PRN) approach, the retina specialist administers intravitreal injections when disease activity is observed on ophthalmologic exam or optical coherence tomography results. The treat-and-extend (T&E) regimen involves fixed treatment intervals followed by a stepwise escalation or de-escalation in the treatment interval based on the presence or absence of disease activity.28 In a 2021 survey of ASRS retina specialists, 59.6% of respondents noted that they preferred T&E or PRN regimens because patients were unable to or did not want to maintain a fixed treatment regimen. Another 23% of respondents stated that these regimens have become the standard of care.20
A major factor in successful anti-VEGF therapy is initiating the treatment as soon as possible, as early intervention has been shown to preserve vision and increase QOL.29 For example, a cost-utility analysis was performed that compared bevacizumab, ranibizumab, and aflibercept in the treatment of nAMD. The main outcome measurements included cost-utility ratios (CUR), cost, and quality-adjusted life-years (QALYs) gained over an 11-year period. Data showed both bevacizumab and ranibizumab were associated with an 11-year gain of 1.399 QALYs, while aflibercept conferred an 11-year gain of 1.38 QALYs. The mean ophthalmic cost perspective CUR was $11,033/QALY for bevacizumab, $79,600/QALY for ranibizumab, and $44,801/QALY for aflibercept. Early initiation of treatment was critical in preserving vision, as anti-VEGF therapies were 144% to 153% more cost-effective when given early rather than late.29 These numbers emphasize the importance of identifying and treating new cases of nAMD as early as possible.
The efficacy of anti-VEGF therapies has been proven in randomized, controlled clinical trials. However, lack of adherence and undertreatment in real-world settings remain significant barriers to optimizing patient outcomes. Results of a recent systematic review of real-world data showed that approximately 50% of patients with nAMD stopped treatment within 24 months, and nonadherence occurred in 32% to 95% of patients. Condition-related factors, such as worse VA at baseline, were associated with increased nonadherence, whereas patients whose vision improved more than 3 lines were more likely to be adherent. Social and patient-related factors that played a significant role in poor adherence and undertreatment included transportation, travel distance, fear or discomfort with injections, and desire to stop treatment if there was no notable improvement in vision.30 The majority of patients stopped treatment within the first 6 to 12 months, which indicates their decision whether or not to continue therapy is made early. This presents an opportunity for managed care and specialty pharmacists to further educate patients about the importance of treatment and consistent monitoring.
Managed Care Considerations
A major challenge for managed care pharmacists is optimizing patient outcomes through cost-effective drug utilization. An additional layer of complexity is that a medical prescriber’s drug choices are sometimes not aligned with ideal cost-effective decision making. For instance, self-reporting by physicians indicates that the 2 most common reasons for prescribing medications based on nonscientific data are patient demand and clinical experience with a medication that suggests it to be the best treatment option, despite evidence-based literature indicating otherwise.31 Several strategies are often implemented by managed care organizations to control drug utilization; these may include step therapies, fee schedule management, and mandated utilization through specialty pharmacies to contain costs.
Step therapy is a drug utilization management tool used by managed care organizations that requires treatment with a payer-preferred medication to fail before another therapy will be covered for patients.32 In the ophthalmic space, the presumption with step therapy is that the safety and efficacy of less expensive anti-VEGF agents are comparable to more expensive ones. By adhering to the more cost-effective treatments, patient care will not be compromised. The Centers for Medicare & Medicaid Services (CMS) prohibited step therapy in Medicare Advantage plans for Part B drugs from 2012 to 2018 but removed the ban in 2019, which has allowed Medicare Advantage plans increased leverage to negotiate drug prices.32,33 The AAO has challenged the CMS step therapy mandate, indicating that these drug utilization strategies are dangerous to patients because of the potential for disease flares, complete loss of response, adverse effects, and negative immune responses.33 Despite pushback from the AAO, there are studies with off-label compounded bevacizumab that support a step therapy approach in patients with retinal diseases.
Bevacizumab is preferred by many payers before an alternative anti-VEGF therapy can be tried.34 A recent study evaluated the effectiveness of bevacizumab as step therapy in patients with moderate vision loss and center-involved DME. Patients were randomly assigned in a 1:1 ratio to received either 2 mg of intravitreal aflibercept or 1.25 mg of intravitreal bevacizumab with a switch to 2 mg of aflibercept if the eye met step protocol criteria.34 The primary outcome was the mean change in VA over a 2-year study period. Changes in retinal anatomy were also assessed and included as secondary outcomes. A total of 312 eyes underwent randomization (bevacizumab-first group, n = 154 eyes; aflibercept monotherapy, n = 158). At 2 years, 70% of eyes in the bevacizumab-first group were switched to aflibercept. The mean improvement in VA was similar in both treatment groups (15 vs 14 letters in aflibercept and bevacizumab-first groups, respectively; adjusted difference, 0.8 letters; 95% CI, −0.9 to 2.5; P = .37). Mean changes in central retinal subfield thickness favored aflibercept at 24 and 52 weeks, but the percentage of eyes at 2 years with a central subfield thickness below thresholds for DME were similar in both treatment groups (aflibercept group, 60%; bevacizumab-first group, 55%; adjusted difference, 4 percentage points; 95% CI, −12 to 20).34 These findings show favorable results of treating patients with moderate vision loss and DME with bevacizumab as a first-line drug utilization strategy.
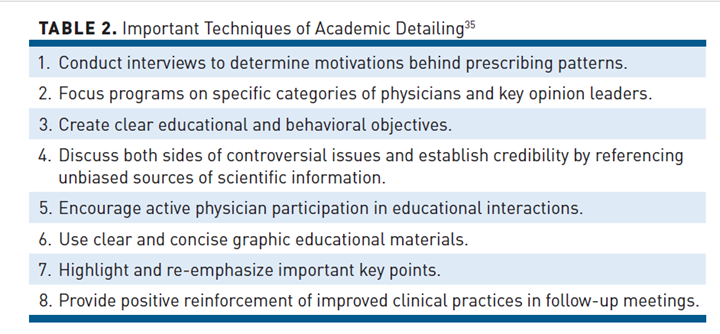
Another method that has been used with some success is academic detailing, which involves targeted instruction by trained personnel to health care providers to help them utilize best practices.35 Key components of academic detailing are highlighted in Table 2.35 Aflibercept and ranibizumab represented the first and sixth highest drug spend for Medicare Part B in 2019, despite bevacizumab being widely considered first-line treatment for nAMD and DME.26,36 As a result, managed care organizations must ensure that drugs are being prescribed as rationally as possible. Academic detailing in these circumstances can be an effective managed care intervention. In 2018, a low-cost alternative program implemented a new fee schedule methodology for bevacizumab, ranibizumab, and aflibercept for a regional health plan that consisted of 2.7 million members. The new fee schedule increased the reimbursement of bevacizumab from the previous market rate to provide a dollar margin comparable to ranibizumab and aflibercept. Pharmacists provided academic detailing to provider groups through data and clinical analytics, which highlighted the concept of collaboration around value-based care. After 2 years of implementation, the new fee schedule shifted an increase in market share of bevacizumab by 17.5%, reduced brand market share by 11.4%, and saved the plan approximately $2.74 million per year.37 These data demonstrate that pharmacist-led academic detailing can improve physician prescribing behaviors for high-cost ophthalmic drugs.
It is important for managed care pharmacists to understand real-world anti-VEGF treatment patterns in different populations to appropriately evaluate patient outcomes and cost. A retrospective analysis provided valuable insight regarding treatment frequency and health care resource utilization associated with ranibizumab and aflibercept among treatment-naïve and previously treated patients with nAMD or DME. Study results showed injection frequency and cost were not different between treatment-naïve patients with nAMD who received ranibizumab when compared with aflibercept at 12 months (5.62 vs 5.54; P = 0.52; and $11,351 vs $10,702; P = .06) or 24 months (7.86 vs 8.37; P = .16; and $16,286 vs $16,666; P = .69).38 Conversely, in patients with nAMD who were previously treated with anti-VEGF therapy, injection frequency was significantly lower in ranibizumab-treated patients over 24 months (7.98 vs 9.63; P = .03), although treatment costs were comparable over the same time ($16,303 vs $19,361; P = .13). In treatment-naïve patients with DME, ranibizumab was associated with significantly fewer injections and lower costs than aflibercept over 12 months (3.33 vs 3.87; P = .001; and $4136 vs $7656; P = .001). Despite nonsignificant differences in injection frequency, previously treated patients with DME showed similar cost-savings as treatment-naïve patients at 12 months ($4606 vs $9190; P = .02).38 This study is important for a few reasons. It shows that aflibercept may be a more cost-effective treatment option than ranibizumab in both treatment-naïve and previously treated patients with DME over 12 months. For payers, this information is critical because they need to assess the impact of different anti-VEGF treatment regimens on their drug budgets. Lastly, the study results show that real-world treatment patterns often do not reflect FDA-approved dosing schedules, which is cause for concern because fewer treatments may contribute to worse vision outcomes and increased costs.
Although most budget impact models use manufacturer-recommended anti-VEGF treatment regimens to predict the financial consequences of adding a new drug to formulary, it is important that managed care organizations can quantify the potential budgetary impact of new medications based on variable frequency regimens, such as PRN, T&E, and real-world evidence (RWE). A recent study was conducted to estimate the budgetary impact of the following 4 treatment regimens of brolucizumab in patients with nAMD over a 1-year period: manufacturer dosing recommendations per FDA product labeling, PRN, T&E, and RWE.39 Data showed the manufacturer-recommended brolucizumab regimen led to an annual savings of $93,068, and the RWE regimen led to an annual savings of $94,170. Conversely, a maximum increase in expenditure was associated with brolucizumab PRN ($824,696) and T&E treatment regimens ($163,101). Based on 2022 census data including adults aged 50 years and older, the introduction of brolucizumab would result in a cost-savings of approximately $31 million in both the manufacturer-recommended and RWE treatment regimens but an increase in annual expenditures in the T&E and PRN regimens ($54 million and $274 million, respectively). The study results emphasize the importance of considering all available treatment regimens and how each regimen might impact drug spending. While the study focused on drug expenditures and cost-savings, managed care organizations must take into account patient drug preferences, provider suggestions, indirect costs, and clinical outcomes when considering the addition of medications to drug formularies.39
Conclusions
The prevalence rates of nAMD and DME are increasing, and these trends are not expected to slow down due to an aging population and improved life expectancy. Vision impairment is associated with loss of independence and compromised mental health, underscoring the importance of optimal cost-effective care. With the emergence of new treatment options in a competitive market space, managed care pharmacists must stay current with evidence-based drug information, updates on emerging biosimilars, and prescribing behaviors of medical providers. With proper management, formulary coverage of anti-VEGF agents can result in significant cost-savings while still allowing individualized patient treatment.
Author affiliation: Khalid M. Kamal, MPharm, PhD, is professor and chair of the department of Pharmaceutical Systems and Policy, West Virginia University School of Pharmacy, Morgantown, WV.
Funding source: This activity is supported by an educational grant from Genentech, a member of the Roche Group.
Author disclosure: Dr Kamal has the following relevant financial relationships with commercial interests to disclose: Grant/Research Support: Cerevel Therapeutics, EMD Serono; Consultant: Pfizer/Cytel Inc.
Authorship information: Drafting of the manuscript; critical revision of the manuscript for important intellectual content; supervision; and administrative, technical, or logistic support.
Address correspondence to: kkamal@hsc.wvu.edu
Medical writing and editorial support provided by: Andrew Abe, PharmD
References
- Deng Y, Qiao L, Du M, et al. Age-related macular degeneration: epidemiology, genetics, pathophysiology, diagnosis, and targeted therapy. Genes Dis. 2021;9(1):62-79. doi:10.1016/j.gendis.2021.02.009
- Rein DB, Wittenborn JS, Burke-Conte Z, et al. Prevalence of age-related macular degeneration in the US in 2019. JAMA Ophthalmol. 2022;140(12):1202-1208. doi:10.1001/jamaophthalmol.2022.4401
- Ehrlich R, Harris A, Ciulla TA, Kheradiya N, Winston DM, Wirostko B. Diabetic macular oedema: physical, physiological and molecular factors contribute to this pathological process. Acta Ophthalmol. 2010;88(3):279-291. doi:10.1111/j.1755-3768.2008.01501.x
- Cannon E. Managed care opportunities and approaches to supporting appropriate selection of treatment for sight preservation. Am J Manag Care. 2019;25(10 suppl):S182-S187.
- Cooper OAE, Taylor DJ, Crabb DP, Sim DA, McBain H. Psychological, social and everyday visual impact of diabetic macular oedema and diabetic retinopathy: a systematic review. Diabet Med. 2020;37(6):924-933. doi:10.1111/dme.14125
- Marques AP, Ramke J, Cairns J, et al. The economics of vision impairment and its leading causes: a systematic review. EClinicalMedicine. 2022;46:101354. doi:10.1016/j.eclinm.2022.101354
- Varma R, Vajaranant TS, Burkemper B, et al. Visual impairment and blindness in adults in the United States: demographic and geographic variations from 2015 to 2050. JAMA Ophthalmol. 2016;134(7):802-809. doi:10.1001/jamaophthalmol.2016.1284
- Wong WL, Su X, Li X, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health. 2014;2(2):e106-e116. doi:10.1016/S2214-109X(13)70145-1
- Lundeen EA, Andes LJ, Rein DB, et al. Trends in prevalence and treatment of diabetic macular edema and vision-threatening diabetic retinopathy among Medicare Part B fee-for-service beneficiaries. JAMA Ophthalmol. 2022;140(4):345-353. doi:10.1001/jamaophthalmol.2022.0052
- Lundeen EA, Kim M, Rein DB, et al. Trends in the prevalence and treatment of diabetic macular edema and vision-threatening diabetic retinopathy among commercially insured adults aged <65 years. Diabet Care. 2023;46(4):687-696. doi:10.2337/dc22-1834
- Teo ZL, Tham YC, Yu M, et al. Global prevalence of diabetic retinopathy and projection of burden through 2045: systematic review and meta-analysis. Ophthalmology. 2021;128(11):1580-1591. doi:10.1016/j.ophtha.2021.04.027
- Almony A, Keyloun KR, Shah-Manek B, et al. Clinical and economic burden of neovascular age-related macular degeneration by disease status: a US claims-based analysis. J Managed Care Spec Pharm. 2021;27(9):1260-1272. doi:10.18553/jmcp.2021.27.9.126
- Brown MM, Brown GC, Lieske HB, Tran I, Turpcu A, Colman S. Societal costs associated with neovascular age-related macular degeneration in the United States. Retina (Philadelphia, Pa.). 2016;36(2):285-298. doi:10.1097/IAE.000000000000071
- Parikh R, Ross JS, Sangaralingham LR, Adelman RA, Shah ND, Barkmeier AJ. Trends of anti-vascular endothelial growth factor use in ophthalmology among privately insured and Medicare Advantage patients. Ophthalmology. 2017;124(3):352-358. doi:10.1016/j.ophtha.2016.10.036
- Cubanski J, Neuman T. Relatively few drugs account for a large share of Medicare prescription drug spending. Kaiser Family Foundation. Published April 19, 2021. Accessed February 21, 2023. www.kff.org/medicare/issue-brief/relatively-few-drugs-account-for-a-large-share-of-medicare-prescription-drug-spending/
- Van de Wiele VL, Hammer M, Parikh R, Feldman WB, Sarpatwari A, Kesselheim AS. Competition law and pricing among biologic drugs: the case of VEGF therapy for retinal diseases. J Law Biosci. 2022;9(1):lsac001. doi:10.1093/jlb/lsac001
- Erie JC, Barkmeier AJ, Hodge DO, Mahr MA. High variation of intravitreal injection rates and medicare anti-vascular endothelial growth factor payments per injection in the United States. Ophthalmology. 2016;123(6):1257-1262. doi:10.1016/j.ophtha.2016.02.015
- Bressler NM, Varma R, Mitchell P, et al. Effect of ranibizumab on the decision to drive and vision function relevant to driving in patients with diabetic macular edema: report from RESTORE, RIDE, and RISE trials. JAMA Ophthalmol. 2016;134(2):160-166. doi:10.1001/jamaophthalmol.2015.4636
- Emami-Naeini P, Boucher N, Fernando R, Menezes A, Garmo V. Long-term maintenance of vision required to drive in patients with neovascular age-related macular degeneration (nAMD) and diabetic macular edema (DME) following anti-VEGF intravitreal therapy (IVT). Abstract presented at: Association for Research in Vision and Ophthalmology (ARVO) Annual Meeting; Virtual; May 1-7, 2021. Investig Ophthalmol Vis Sci. 2021;62(8):3516. iovs.arvojournals.org/article.aspx?articleid=2774063
- Global trends in retina. The American Society of Retina Specialists. Accessed January 29, 2023. www.asrs.org/sections/international/global-trends-in-retina
- Voluntary recall of the Susvimo ocular implant. Genentech, Inc; October 2022. Accessed February 19, 2023. www.gene.com/download/pdf/Susvimo_DHCP_Important_Prescribing_Information_2022-10-18.pdf
- Prenner JL, Halperin LS, Rycroft C, Hogue S, Williams Liu Z, Seibert R. Disease burden in the treatment of age-related macular degeneration: findings from a time-and-motion study. Am J Ophthalmol. 2015;160(4):725-731.e1. doi:10.1016/j.ajo.2015.06.023
- Meer EA, Oh DH,Brodie FL. Time and distance cost of longer acting anti-VEGF therapies for macular degeneration: contributions to drug cost comparisons. Clin Ophthalmol. 2022;16:4273-4279. doi:10.2147/OPTH.S384995
- Amoaku WM, Chakravarthy U, Gale R, et al. Defining response to anti-VEGF therapies in neovascular AMD [published correction appears in Eye (Lond). 2015;29(10):1397-1378]. Eye (Lond). 2015;29(6):721-731. doi:10.1038/eye.2015.48
- The use of biosimilars in ophthalmic practice—2022. American Academy of Ophthalmology. Published January 1, 2022. Accessed February 11, 2023. www.aao.org/clinical-statement/use-of-biosimilars-in-ophthalmic-practice
- Bro T, Derebecka M, Jørstad ØK, Grzybowski A. Off-label use of bevacizumab for wet age-related macular degeneration in Europe. Graefes Arch Clin Exp Ophthalmol. 2020;258(3):503-511. doi:10.1007/s00417-019-04569-8
- Bhagat D, Kirby B, Bhatt H, Jager R, George M, Sheth V. Patient preferences associated with anti-vascular endothelial growth factor therapies for neovascular age-related macular degeneration and diabetic macular edema. Clin Ophthalmol. 2020;14:2975-2982. doi:10.2147/OPTH.S273564
- Freund KB, Korobelnik JF, Devenyi R, et al. Treat-and-extend regimens with anti-VEGF agents in retinal diseases: a literature review and consensus recommendations. Retina. 2015;35(8):1489-1506. doi:10.1097/IAE.0000000000000627
- Brown GC, Brown MM, Rapuano S, Boyer D. Cost-utility analysis of VEGF inhibitors for treating neovascular age-related macular degeneration. Am J Ophthalmol. 2020;218:225-241. doi:10.1016/j.ajo.2020.05.029
- Okada M, Mitchell P, Finger RP, et al. Nonadherence or nonpersistence to intravitreal injection therapy for neovascular age-related macular degeneration: a mixed-methods systematic review. Ophthalmology. 2021;128(2):234-247. doi:10.1016/j.ophtha.2020.07.060
- Schwartz RK, Soumerai SB, Avorn J. Physician motivations for nonscientific drug prescribing. Soc Sci Med. 1989;28(6):577-582. doi:10.1016/0277-9536(89)90252-9
- Medicare Advantage prior authorization and step therapy for Part B drugs. Centers for Medicare & Medicaid Services. Published August 2018. Accessed March 10, 2023. www.cms.gov/newsroom/fact-sheets/medicare-advantage-prior-authorization-and-step-therapy-part-b-drugs
- Mott M. Step therapy: clinicians concerns and challenges. American Academy of Ophthalmology: EyeNet Magazine. Published April 2022. Accessed March 2, 2022. www.aao.org/eyenet/article/step-therapy-clinicians-concerns-and-challenges
- Jhaveri CD, Glassman AR, Ferris FL 3rd, et al; DRCR Retina Network. Aflibercept monotherapy or bevacizumab first for diabetic macular edema. N Engl J Med. 2022;387(8):692-703. doi:10.1056/NEJMoa2204225
- Soumerai SB, Avorn J. Principles of educational outreach (‘academic detailing’) to improve clinical decision making. JAMA. 1990;263(4):549-556.
- Cubanski J, Sroczynski N, Neuman T. Medicare Part B drugs: cost implications for beneficiaries in traditional Medicare and Medicare Advantage. Kaiser Family Foundation. Published March 15, 2022. Accessed February 23, 2023. www.kff.org/medicare/issue-brief/medicare-part-b-drugs-cost-implications-for-beneficiaries-in-traditional-medicare-and-medicare-advantage/
- Kelly K, Bhatt S, Aten A, Sockman C, Sumner A, Denno M. Cost of care initiative: analyzing a least cost alternative program with specialty ophthalmic injections under the medical benefit. Poster presented at: Academy of Managed Care Pharmacy Annual Meeting 2018; April 23-26, 2018; Boston, MA; Accessed February 21, 2023. www1.magellanrx.com/documents/2019/03/research_opthamology_analysis-least-cost-alternative-specialty-ophthalmic-injections.pdf/
- Kiss S, Malangone-Monaco E, Wilson K, et al. Real-world injection frequency and cost of ranibizumab and aflibercept for the treatment of neovascular age-related macular degeneration and diabetic macular edema. J Manag Care Spec Pharm. 2020;26(3):253-266. doi:10.18553/jmcp.2020.19245
- Siddiqui ZA, Dhumal T, Patel J, LeMasters T, Almony A, Kamal KM. Cost impact of different treatment regimens of brolucizumab in neovascular age-related macular degeneration: a budget impact analysis. J Manag Care Spec Pharm. 2022;28(12):1350-1364. doi:10.18553/jmcp.2022.28.12.1350
2 Commerce Drive
Cranbury, NJ 08512
AJMC®
All rights reserved.