- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Exploring the Clinical Burden of OFF Periods in Parkinson Disease
ABSTRACT
Parkinson disease, the second-most-common neurodegenerative disorder, affects approximately 1 million individuals in the United States, and this number is projected to increase to 1.2 million by 2030. Characterized pathologically by degeneration of dopaminergic neurons, with widespread pathology in nondopaminergic systems, Parkinson disease leads to an array of motor and nonmotor symptoms that can significantly impact an affected individual’s quality of life. Treatments for Parkinson disease typically focus on controlling the motor symptoms of the disease, including treating OFF periods when motor symptoms return. OFF periods can occur for many individuals with Parkinson disease, especially as the disease progresses, and can pose a substantial burden to those with the disease and their caregivers. Available treatments for OFF periods may help alleviate this burden.
Am J Manag Care. 2020;26:S255-S264. https://doi.org/10.37765/ajmc.2020.88517
For author information and disclosures, see end of text.
Introduction
Parkinson disease (PD) is the second-most-common neurodegenerative disorder in the world.1 The global prevalence of PD increased 145% to an estimated 6.1 million people from 1990 to 2016, according to the results of the 2016 Global Burden of Disease Study.2 In the United States, the prevalence of PD among individuals 45 years and older is projected to increase to about 930,000 people in 2020 and to 1.2 million by 2030.3 As the population of older individuals continues to grow, the number of people with Parkinson disease (PwP) is expected to continue to rise.
Diagnosis of PD usually occurs after age 50 years, and incidence rises with increasing age.1 In most populations, incidence of PD is twice as common in men as in women.1 In a population-based study conducted in Olmsted County, Minnesota, incidence was observed to increase over a 30-year period, particularly in men 70 years or older (relative risk, 1.35 per decade; 95% CI, 1.10-1.65; P = .004).4
Etiology
The cause of PD is likely multifactorial in most cases, resulting from the combined effects of environment (eg, exposure to toxicants like certain pesticides), lifestyle factors, and genes.5,6
Lifestyle factors, including regular physical activity and adherence to a healthy diet (eg, the Mediterranean diet7), have been associated with a lower risk of PD; however, the most consistent lifestyle factor that has been seen to have an association with reduced risk of PD has been cigarette smoking, with a lower risk seen among those with a longer duration and greater frequency of tobacco use.8 Caffeine use, including coffee drinking, and physical activity—particularly at higher intensities—have also been shown to be associated with a lower risk of PD, especially in men.9,10
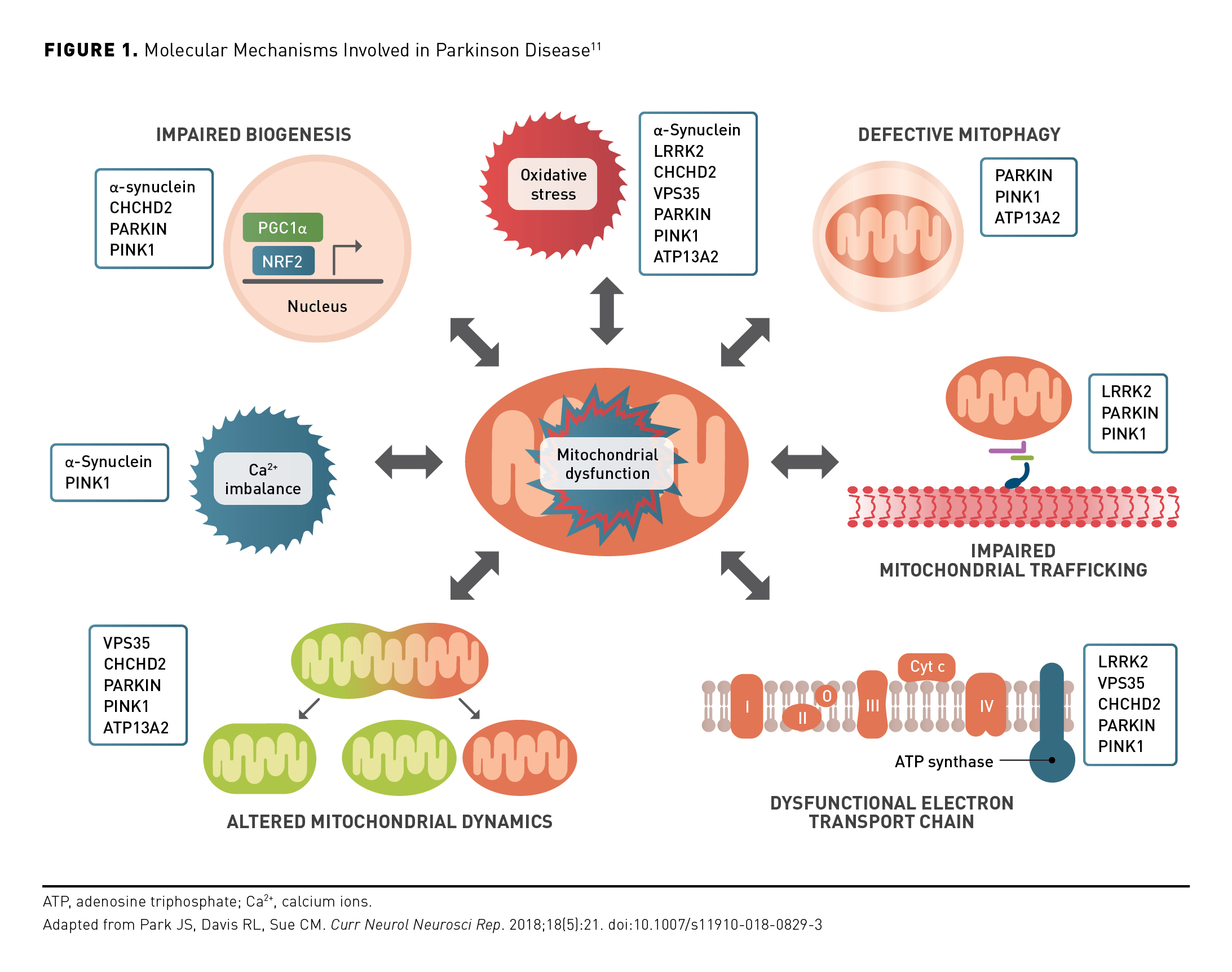
Approximately 5% to 10% of PD cases are familial and are associated with inherited pathogenic mutations in several genes, including LRRK2, SNCA, GBA, PARKIN, PINK1, and DJ1.1,5 These gene mutations correspond with dysfunctional protein products, which contribute to molecular mechanisms implicated in the pathogenesis of PD (Figure 1).11 The most common of these are mutations in LRRK2, with a higher prevalence reported in certain populations, including those of Ashkenazi Jewish ancestry and North African Arab ancestry.12,13 PARKIN and PINK1 gene mutations have been identified as causes of early-onset autosomal recessive PD.14-16
PD has characteristic pathological features, including widespread α-synuclein accumulation and dopaminergic neuronal loss in specific areas of the substantia nigra (SN), which are specific for a definitive diagnosis of the disease when present together.1 It has been hypothesized that aggregates of misfolded alpha-synuclein protein, a pathogenic hallmark of PD, propagate to multiple brain regions in a characteristic pattern with clinical correlates of anosmia, constipation, and rapid eye movement sleep behavior disorder, which commonly precede motor abnormalities in PwP.1,17,18 Loss of dopaminergic neurons occurs in the ventrolateral SN during early stages of PD and leads to the characteristic motor symptom of the disease, bradykinesia (slowed movement), which can be partially managed with symptomatic therapies that increase central nervous system dopamine.19 As neuronal degeneration progresses and becomes more widespread in end-stage disease, symptom amelioration is reduced and patients experience increased functional deficits.20,21
Diagnosis of Parkinson Disease
The progression of PD is slow and typically begins years before the condition reaches a point where it can be diagnosed. The essential diagnostic criterion is bradykinesia combined with rest tremor and/or rigidity—the definition of parkinsonism. This diagnosis, as well as all the signs and symptoms of PD, are based on clinical criteria established by the Movement Disorder Society (MDS).1,22
The MDS-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS), a clinical rating scale, measures motor and nonmotor aspects of PD using historical and objective information from patient, caregiver, and the examination.23,24 Requirements for a diagnosis of clinically established PD as presented in the MDS Clinical Diagnostic Criteria for Parkinson’s Disease include the presence of bradykinesia and at least 1 of tremor or rigidity, assessed as described in the MDS-UPDRS, the absence of absolute exclusion criteria (eg, cerebellar abnormalities, probable behavioral variant frontotemporal dementia), at least 2 supportive criteria (eg, verifiable benefit to dopaminergic therapy and resting tremor in a limb), and none of what are deemed as red flags (eg, gait impairment that necessitates the use of wheelchair within 5 years of diagnosis, bilateral symmetric parkinsonism).22
Symptoms of Parkinson Disease
The symptoms of PD can be divided into 2 groups: nonmotor symptoms and motor symptoms.1
Nonmotor Symptoms
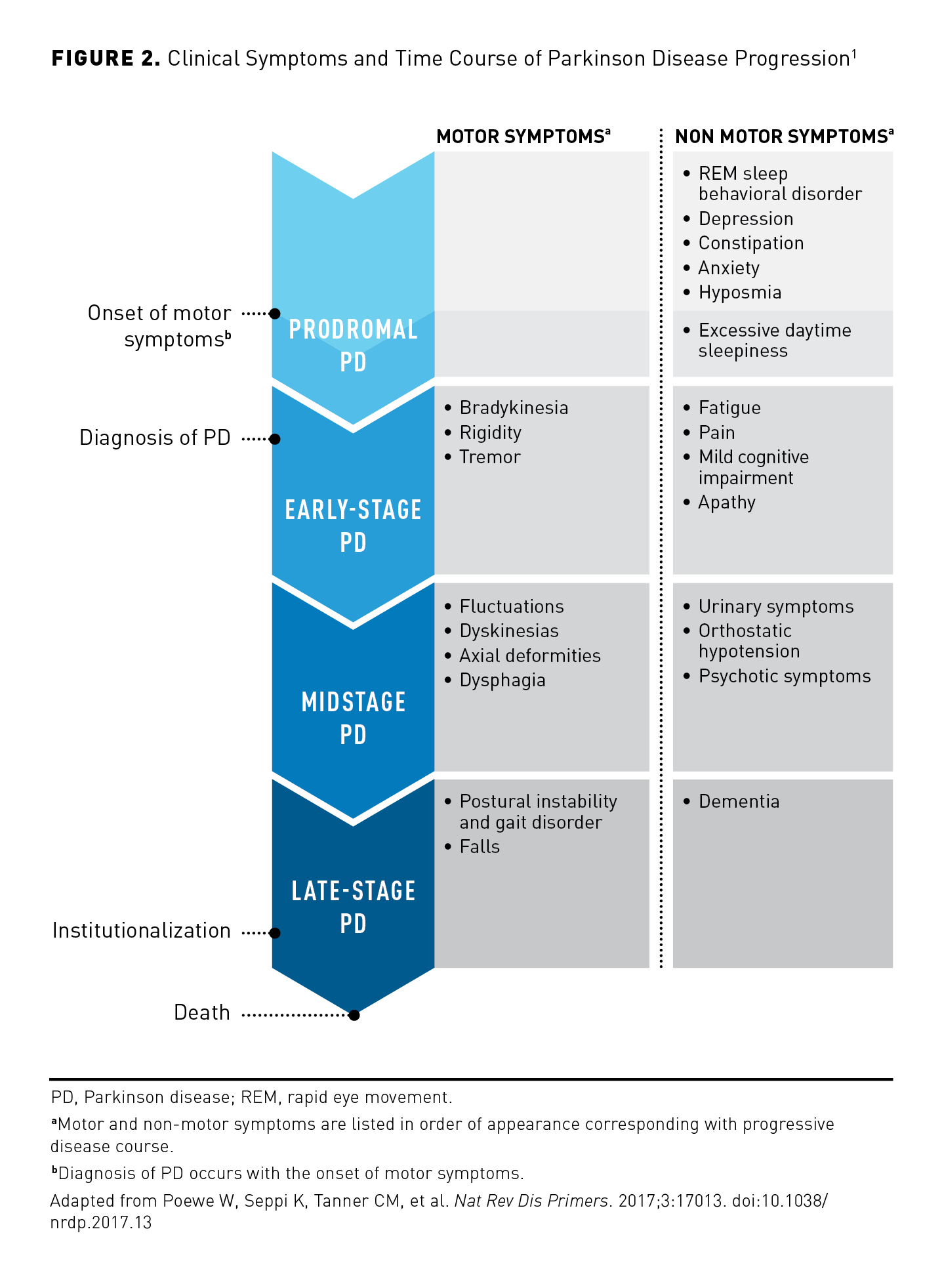
Nonmotor symptoms may appear years before the onset of motor symptoms (Figure 21) and have been shown to afflict a majority of PwP.1,25 Patients may experience a variety of nonmotor symptoms, ranging from cognitive impairment, depression, anxiety, sleep disorders, fatigue, sexual dysfunction, impaired olfaction and taste, increased occurrence of periodontal disease (likely secondary to poor oral hygiene and excessive saliva production), and autonomic dysfunction, including bowel and bladder dysfunction.24,26-28
Gastrointestinal (GI) dysfunction is a common nonmotor symptom in PwP, with the most prevalent GI symptom being constipation, as reported in 80% to 90% of patients.27 Constipation is likely multifactorial in origin, a result of disease-associated autonomic nervous system dysfunction, reduced physical activity, dietary changes, and adverse effects (AEs) of antiparkinsonian therapy.22,27 Malnutrition, secondary to gastroparesis, and small intestinal bacterial growth (SIBO) may occur, especially as PD progresses.27,29 PwP with SIBO more frequently have severe motor fluctuations than those without SIBO, possibly due to impaired absorption of levodopa.27,30
Motor Symptoms
Motor symptoms include the physical, visible signs of parkinsonism, including bradykinesia, muscular rigidity, resting tremor, and postural instability (Figure 2).1 Gait disorder, falls, axial postural deformities, and dysphagia (difficulty swallowing) are increasingly common as the disease advances.1 As many as 77% of PwP have been shown to suffer from dysphagia, which may be associated with subsequent difficulties in eating and poor nutrition.27 In advanced disease, oropharyngeal abnormalities and pharyngeal dysfunction may also contribute to an increased risk of aspiration and subsequent risk of upper respiratory tract infection and pneumonia.31
Treatment of Motor Symptoms of Parkinson Disease
Levodopa is the standard of care for the pharmacologic treatment of the motor symptoms of PD. Levodopa is typically combined with aromatic amino acid decarboxylase inhibitors and sometimes catechol-O-methyltransferase inhibitors to prolong central pharmacologic activity.32 Levodopa is available in various formulations, including immediate-release and extended-release oral formulations, enteral infusions, and an oral inhalation powder. Other drug treatments for the motor symptoms of PD include dopamine receptor agonists, monoamine oxidase B inhibitors, amantadine, and centrally active antimuscarinic agents. Each agent can be used alone or combined with others, although as PD advances, levodopa therapy is inevitably needed to maximize treatment benefit.33,34 Surgical therapies can also be efficacious in treating the motor symptoms of PD,35 but will not be reviewed here.
Pharmacotherapies for managing the symptoms of PD show the greatest efficacy early in the course of the disease. Symptoms typically then become increasingly refractory to standard therapies (levodopa) as the disease advances, and as a result, many patients may begin to experience fluctuations in the symptoms (ie, OFF periods, defined next) within 2 years of starting therapy.Because refractory symptoms can be related to the severity of the illness, fluctuations may begin after a much shorter therapy interval if treatment is started late in the course of the disease. Although the mechanism for fluctuations in motor response is not known, investigators postulate that as the disease progresses, the number of presynaptic dopaminergic terminals may decline; this may result in a decreased ability to store dopamine and a consequent vulnerability to fluctuations of levodopa levels in the plasma.1 Factors that have been postulated to contribute to delayed clinical response to a dose or to complete dosing failure, include delayed gastric emptying and dysphagia, dietary factors (specifically high-protein foods, which compete with levodopa absorption), or possibly other factors, such as Helicobacter pylori infection or certain constituents of the intestinal microbiome.34,36,37
Motor Complications of Parkinson Disease
Dyskinesias
Levodopa-induced dyskinesias are AEs of chronic treatment with levodopa. Dyskinesias typically manifest as hyperkinetic movements, although dystonia may also occur.1,38 Prior research has shown that the median weighted percentage of PwP who experienced the motor complication of dyskinesia within 2.5 to 3.5 years of starting long-term levodopa therapy was 26.9% followed by 36.2% within 4 to 6 years, and 87.8% within 9 to at least 15 years.39
ON vs OFF Periods
Although response to dopaminergic therapy can be characterized by sustained efficacy early in the course of PD, fluctuations in response to therapy occur as the disease progresses, with alternating periods of more and less effective control of motor symptoms.39 By convention, periods of symptom improvement from antiparkinsonian therapy are referred to as ON periods, and periods of symptom worsening are termed OFF periods.24
ON Periods
ON periods refer to times when medications to treat the symptoms of PD are working and symptoms are improved. ON periods are further characterized as: ON without the motor AE dyskinesia, ON with dyskinesia that is not troublesome, and ON with troublesome dyskinesia.24,36 The latter may be nearly as disabling as severe OFF episodes. As a consequence, treatment of advanced PD aims to achieve a therapeutic balance that minimizes fluctuations overall and, in particular, avoids extremes of OFF as well as ON with troublesome dyskinesias.34,40
OFF Periods
OFF periods, or OFF episodes, generally refer to a period when PD symptoms worsen despite antiparkinsonian therapy. The term OFF can be used to describe delayed onset of response to a levodopa dose, reduced duration of benefit, and reduced or no efficacy of a dose; however, no formal, codified definition of OFF exists.36 Several terms have been used to describe types of OFF periods; however, all refer to a point at which the motor symptoms and/or nonmotor symptoms of PD return or worsen, thus negatively affecting the patient’s ability to function (Table 1).34,36,41,42
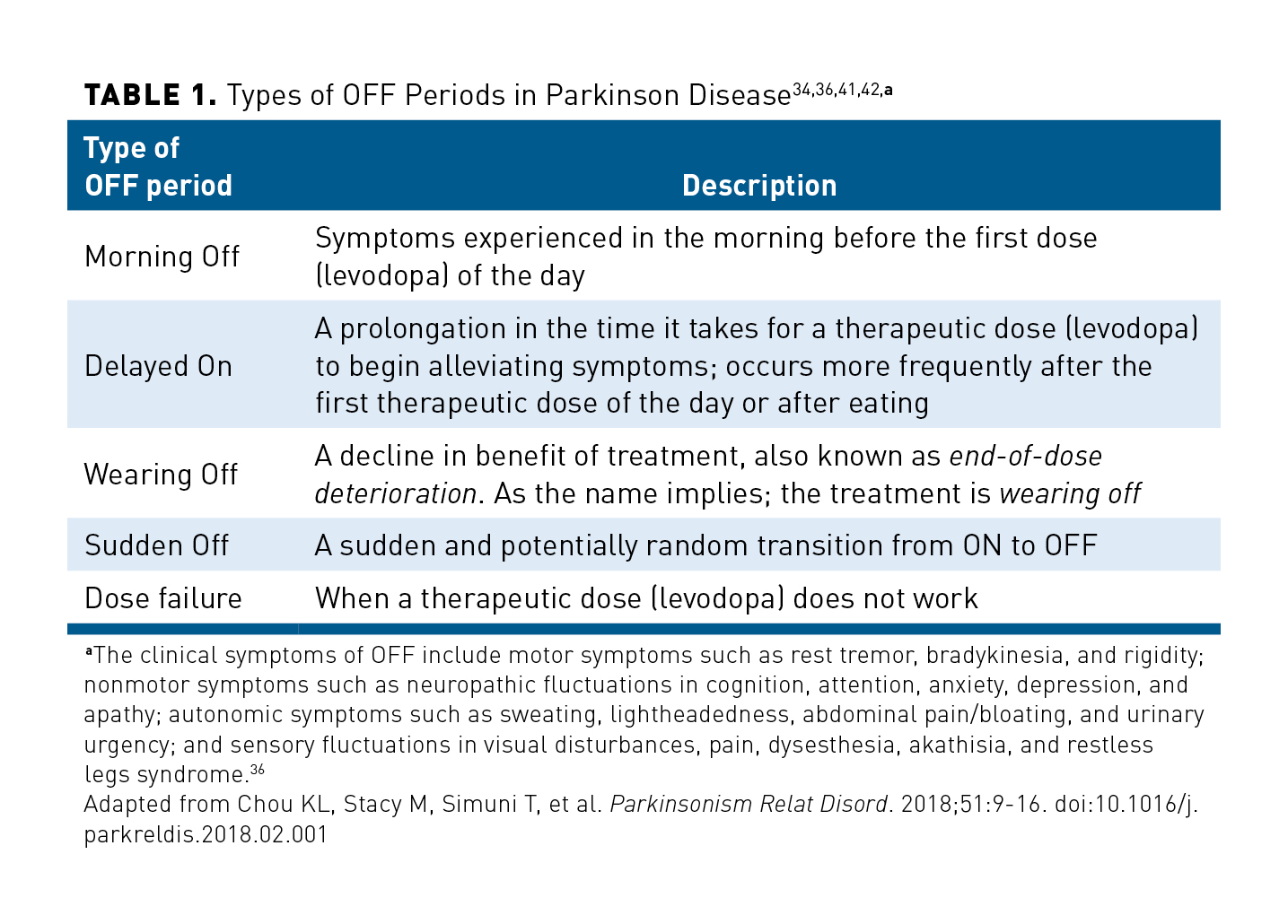
Types and severity of symptoms can be specific to each patient.36 OFF periods can be predictable or unpredictable and may have gradual or sudden onset.42 The variability of OFF periods and the difficulty of describing them have been cited as major barriers to their treatment. Because OFF periods are often poorly defined and identified, the symptoms of OFF periods are commonly underreported and go undetected by clinicians.1,36,43 This may likely be due to multiple factors, including time constraints at in-office visits, poor communication between the patient and practitioner, a misunderstanding that symptoms might not revolve around treatment and can occur in both ON and OFF states, lack of terminology, and the varying degrees of symptom severity, which can also appear differently based on the patient’s response to the levodopa cycle.1,36,43 Symptom severity may be accompanied by irregular occurrences, which may also lead to underreporting because patients might not recognize it as a symptom and not record or report it.44
Clinical Burden of OFF Periods
The debilitating motor symptoms and underrecognized nonmotor symptoms that PwP experience can have far-reaching effects on their quality of life (QOL). About 40% of PwP will experience OFF episodes within 4 to 6 years of starting oral levodopa treatment, and about 70% of patients will experience them after 9 years or more.39 A common form of OFF period is termed wearing off, and it is characterized by a reduced duration of full clinical benefit followed by a decline in response after a levodopa dose (Table 1).34,36,41,42
To elucidate patients’ experiences with symptoms of OFF periods, Armstrong and colleagues interviewed PwP and their caregivers. For this 2019 qualitative analysis, participants had to be US residents, have a diagnosis of PD, be experiencing OFF periods, and have a caregiver willing to be interviewed. The results were compared with the 19-item Wearing off Questionnaire (WOQ-19). Overall, participants found describing OFF period symptoms to be difficult, demonstrating a lack of terminology knowledge or a clear way to explain how they were feeling. However, despite a lack of consistent terminology, participants were still able to reflect on specific times, or the length of time, that they felt wearing-off or OFF periods and their symptoms. Participants experienced a range of nonmotor and motor symptoms, with most motor symptoms reported being reflective of those seen in the WOQ-19. Nonmotor and motor symptoms reported during OFF periods that were not included in the WOQ-19 included the motor symptoms of immobility, gait changes (in addition to imbalance), freezing, trouble swallowing, and having to concentrate on movements; they also included the nonmotor symptoms of behavioral changes, irritability, fatigue, language difficulties, dizziness, dry mouth, urinary symptoms, and swollen feet. The experience of fatigue was the most common nonmotor symptom of wearing off reported in the study.45
The frequency and severity of nonmotor symptoms were evaluated in a cross-sectional study by Storch and colleagues in 2013.Investigators focused on the frequency and severity of 10 nonmotor symptoms in a study population of 100 patients with advanced PD and motor fluctuations. The average age of patients included in the study was 68.4 years (range, 45-100), and all patients had at least 2 motor complications (such as end-of-dose akinesia or “on-off” phenomenon) and at least 2 nonmotor symptoms. All patients reported experiencing worsening of at least 2 nonmotor symptoms during OFF episodes. Fatigue, impaired concentration, inner restlessness, depression, and anxiety were more common during OFF periods, as assessed by structured clinical evaluations and home-based self-ratings.44
To determine the frequency of symptoms of wearing off and their impact on QOL, Stocchi and colleagues conducted the DEEP (Early DEtection of wEaring off in Parkinson disease) study. This multicenter, observational cross-sectional Italian study assessed the QOL of 617 PwP who had at least 1 year of dopaminergic therapy. The mean treatment duration was 6.6 (SD, ± 4.6) years; 87.2% of PwP were being treated with levodopa and 75.3% were treated with agonists. The 8-item Parkinson’s Disease Questionnaire (PDQ-8) was used to evaluate QOL.46
Patients reported experiencing a mean of 4.1 (SD, ± 3.8) symptoms of wearing off per day (motor and nonmotor symptoms combined). Patients who stated they experienced wearing off were younger, with longer disease duration, longer duration of antiparkinsonian therapy, and greater parkinsonian disability than those who did not experience wearing off. Study results indicated that patients who experienced wearing off reported worse QOL through the PDQ-8 than patients who did not experience wearing off (32.7 [SD, ± 19.2] vs 21.4 [SD, ± 15.7]; P < .0001, respectively). Patient’s QOL also was negatively affected by higher disease severity on the Hoehn and Yahr (H&Y) scale (P = .0003) and the need for a caregiver (P < .0001).46
Chapuis and colleagues analyzed the impact of motor complications of PD on patients’ QOL. For the 9-month study, which was conducted between 2000 and 2001, investigators used sections of the H&Y scale, the UPDRS, and a questionnaire they developed to assess patients based on their motor complications. Of the 143 patients who were assessed, the mean disease duration was 9.1 years and the mean duration of levodopa therapy was 7.7 years. QOL scores were assessed using the PDQ-39, which assesses QOL in 8 domains. End-of-dose akinesia episodes (OFF episodes occurring at the end of a therapeutic dose and before the next dose can take effect) were associated with reduced QOL, particularly affecting the domains of Mobility, Activities of Daily Living, Stigma and Communication. Paradoxical fluctuations and unpredictable OFF episodes adversely affected all those domains as well as Bodily Discomfort. Poor QOL was also associated with an increase in the patient’s daily dosage of levodopa or an increase in the number of doses.47
A Problem of Communication
Confounding the clinical burden of OFF periods is a knowledge and experience gap between patients and their health care provider(s).43 Physicians regularly note that one of the major barriers to understanding and identifying OFF symptoms is the difficulty patients have with recognizing their symptoms as being associated with OFF periods. Furthermore, many patients with advanced PD have cognitive impairment, which can complicate the communication between the patient and physician in identifying OFF periods.48 Caregivers play an important interpreting role in these situations, and they are often expected to be able to fill in the gaps and describe whether improvement has or has not occurred. According to Rastagardani and colleagues, the cornerstone of assessing OFF periods is free-flowing dialogue—a method supported by patients, physicians, and caregivers alike. There is also evidence suggesting that the integration of questionnaires and diaries into this existing method might be helpful to better elucidate the impact of OFF periods on patients.48
A 2-part study published by Levit and colleagues in 2019 analyzed communication shortcomings between treating physicians (general neurologists or movement disorder specialists) and PwP. Their results revealed that physicians often asked patients about OFF period symptoms in the context of their medication regimen (ie, at what time during the day they were taking medications and what medication dose they were taking) versus simply asking about symptomology. As such, this type of conversation led many patients in the study to inaccurately assume that the health care provider was investigating medication adherence versus wearing-off effects or OFF periods. Moreover, patients often were simply unaware of PD symptom progression and did not have appropriate expectations related to their medication and disease state.43 The investigators also found that patients perceived OFF periods as “an inescapable part of the disease.” This was confounded by the counter perception from physicians that patients do not want to mention OFF periods because they believe it is an admission of the disease “getting the better of them.”43
The results of an online survey conducted by Matthews and colleagues in 2013, in which investigators surveyed participants included in The Cure Parkinson’s Trust database, found that symptoms of wearing off impacted patients’ QOL; however, less than half of the survey respondents (47%) indicated that they discussed QOL with their PD specialist.49
Of the 47 pairs of PwP and their caregivers who completed the 21-question survey, the majority of patients received a diagnosis before age 66 years. Care partners were usually a husband (44.7%) or wife (48.9%), followed by a daughter, family friend, or a care partner of no familial relation. Survey results indicated that tiredness, slowness, reduced dexterity, slowness of movement, and slowness in the early morning were symptoms the patients thought to be the most troublesome during their OFF periods, appearing most noticeably 0.5 and 2.0 hours before the next dose of medication. These signs of wearing off were recognized by both the patient and their caregivers who stated that they understood what wearing off meant; however, when asked to define wearing off, patients and caregivers either refrained from answering (53% and 36%, respectively) or answered incorrectly (17% and 47%, respectively).49
Although symptoms of wearing off affected patients’ QOL, QOL was seldom reported during meetings with specialists. Only 47% of patients and 34% of care partners reported that they discussed QOL at appointments. Another 23% of patients disclosed that they talked about their QOL issues only at some appointments, whereas 26% of care partners stated that they were not asked about their own QOL.49
Clinical Approach to OFF Periods
Pharmacologic treatments for OFF periods can be classified as either those that aim to reduce motor fluctuations overall, or those that are indicated for intermittent treatment. The motor symptoms that occur during OFF periods are thought to reflect fluctuations in striatal dopamine activity, likely due to multiple, concomitant issues that vary from person to person. For this reason, pharmacologic approaches to managing OFF periods typically aim to avoid fluctuations in dopaminergic activity and aim primarily to eliminate OFF patterns and change. The standard of care involves 1 or more of the following strategies34:
- Adjusting the dose or frequency of standard carbidopa/levodopa preparations—typically more frequent, smaller doses replace higher, less frequent doses—to achieve a similar total daily dosage50
- Allowing a “rescue” dose of carbidopa/levodopa as needed for unpredictable OFF episodes34
- Using a controlled-release formulation of carbidopa/levodopa34
- Avoiding dietary protein within a fixed time before and after levodopa dosing, to minimize competition for absorption34
- Adding a catechol-O-methyltransferase inhibitor to reduce the peripheral breakdown of levodopa32
- Adding adjunctive oral therapies that reduce motor symptoms of PD in patients being treated with carbidopa/levodopa, such as monoamine oxidase B inhibitors, dopamine receptor agonists, amantadine, or levodopa oral inhalation powder34,51,52
- Using a transdermal patch delivery of the dopamine agonist rotigotine1
Although these approaches may be helpful, none is completely effective in controlling OFF episodes, either individually or in combination.34 Moreover, AEs are commonly associated with each approach, and they often are dose-limiting. These can include AEs associated with increased dopaminergic activity in patients, such as exacerbation of dyskinesias, psychosis, somnolence, and orthostatic hypotension, as well as AEs specific to the individual drugs or classes, such as impulse control disorders.34,42,53
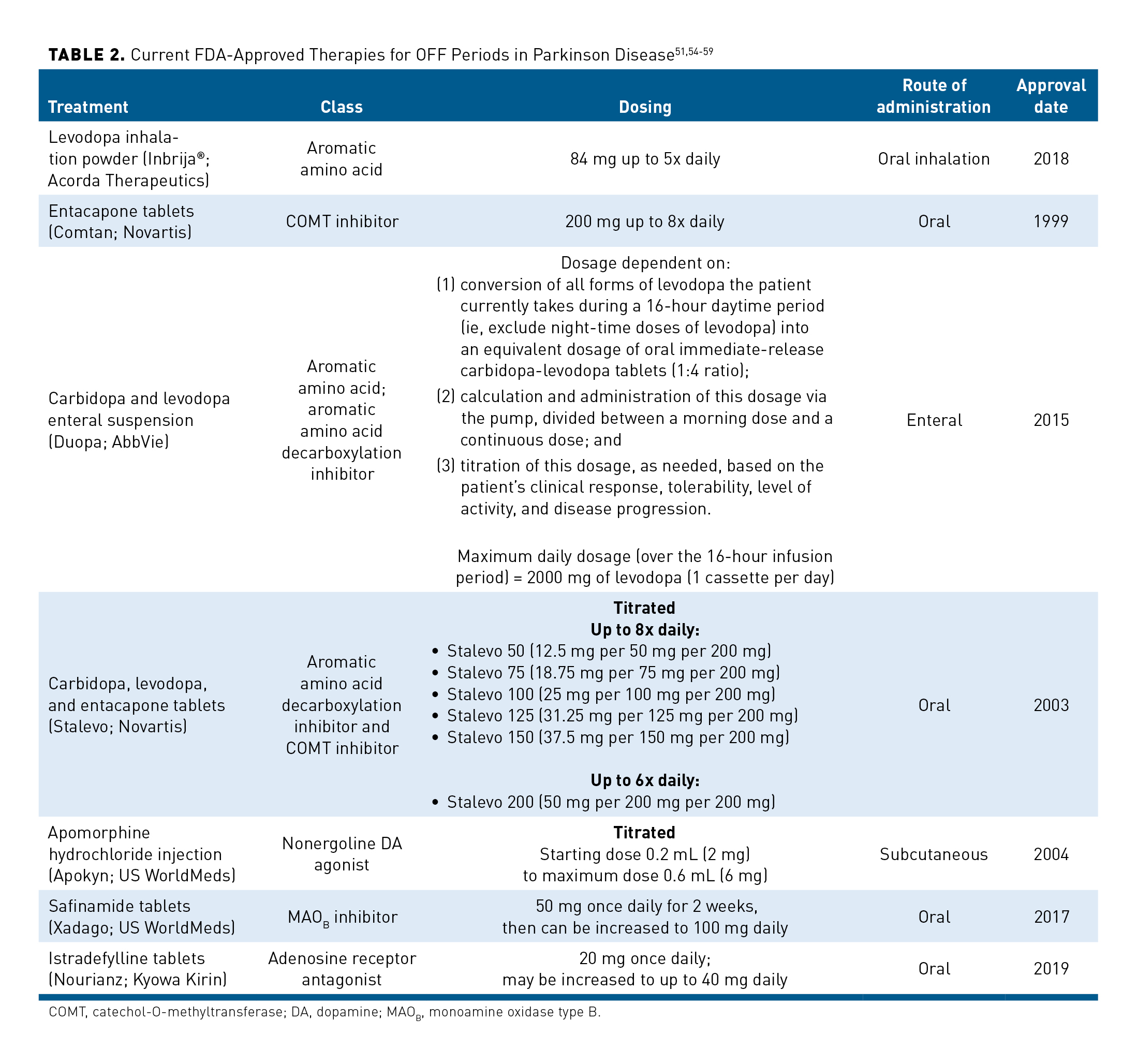
More effective approaches to treating OFF episodes are needed. To address this need, several pharmacological strategies have been approved by the FDA with the specific indication of addressing motor fluctuations and OFF episodes (Table 251,54-59). This manuscript focuses on 3 of these strategies: carbidopa and levodopa enteral suspension (Duopa; AbbVie), apomorphine hydrochloride injection (Apokyn; US WorldMeds), and levodopa inhalation powder (Inbrija®; Acorda Therapeutics).
Carbidopa and levodopa enteral suspension
The carbidopa and levodopa enteral suspension (Duopa, AbbVie) is an FDA-approved combination therapy indicated for treating motor fluctuations in patients with advanced PD. Circumventing the delayed gastric emptying experienced by many patients, the carbidopa and levodopa enteral suspension is delivered through a nasojejunal tube (short-term administration) or through a percutaneous endoscopic gastrostomy with jejunal tube (PEG-J) (long-term administration) as a 16-hour infusion controlled by a programmable portable infusion pump that is worn by the patient.55
The daily dosage of the carbidopa and levodopa enteral suspension can include a morning dose, a continuous dose, and extra doses, which are titrated for each patient. Treatment with carbidopa and levodopa enteral suspension is initiated using 3 primary steps: (1) conversion to oral immediate-release carbidopa-levodopa tablets; (2) calculation and administration of the starting dosage, which consists of the morning dose and continuous dose, for day 1; and (3) titration of the dosage, as needed, based on patient tolerability and clinical response.55
Importantly, the carbidopa and levodopa enteral suspension includes extra doses, which can be used to manage OFF symptoms in an acute setting when they are not controlled by the morning dose and the continuous dose. Once no additional adjustments are needed to the morning, continuous, and extra doses, the regimen should be administered daily; however, additional changes may be required over time based on patient tolerability and clinical response.55
Because the carbidopa and levodopa enteral suspension requires daily manipulation of a pump and management of a PEG-J tube, not all patients who are experiencing motor fluctuations may be able to use this treatment.60 AEs include procedure-related complications, weight loss, and polyneuropathy, as well as those associated with dopaminergic treatment. Failure of the device or the PEG-J may require additional procedures.60,61
Apomorphine hydrochloride subcutaneous injection
Apomorphine hydrochloride injection (Apokyn, US WorldMeds) is a dopamine agonist that can be administered subcutaneously for the acute, intermittent treatment of OFF episodes. Subcutaneous delivery avoids impaired GI absorption and results in symptom reduction beginning 10 minutes after use.41,54 AEs, including nausea and vomiting, orthostatic hypotension, yawning and somnolence, injection site reactions, or exacerbation of dyskinesias, may limit use in some patients.54,62
The results of a phase 4, multicenter, open-label study of the use of subcutaneous apomorphine injections in patients with prolonged morning akinesia, episodes of which were related to delayed or unreliable response following morning doses of levodopa, indicated that the time to ON significantly decreased with subcutaneous apomorphine injection. The trial results were published by Isaacson and colleagues in 2017. For this study, a total of 88 patients self-recorded their time to ON every 5 minutes until onset of benefit for the first 60 minutes after each morning dose of levodopa during a 7-day baseline phase and after each apomorphine injection during a 7-day treatment phase. Study results indicated that the mean ± SD time to ON significantly decreased from 60.86 ± 18.11 minutes with levodopa therapy at baseline to 23.72 ± 14.55 minutes at the end of the treatment time. Furthermore, 95.5% of patients exhibited improvements in time to ON. Only 7% of dose failures were reported with apomorphine compared with 46% with levodopa. Improvements were also reported for QOL scores and motor function following the apomorphine treatment period.41
Levodopa inhalation powder
Levodopa inhalation powder(Inbrija®, Acorda Therapeutics) is an inhalation powder formulation of levodopa forthe intermittent treatment ofOFF episodes in PwP treated with carbidopa/levodopa.51 Inhalation of levodopa has been shown to provide rapid absorption by the lung via the alveolar epithelium.63
The results of an international, randomized, double-blind, placebo-controlled, phase 3 study indicated that treatment with CVT-301 (the inhalation powder formulation of levodopa) was shown to lead to improvements in motor function based on the UPDRS Part 3 scale. The trial was conducted between December 2014 and December 2016 by LeWitt and colleagues.52
Of the 351 patients initially enrolled in the trial, 339 were eligible for assignment. A total of 114 patients were randomly assigned to receive 84 mg of the inhalation powder formulation of levodopa in the intention-to-treat population, 113 were assigned to receive 60 mg, and 112 were assigned to the placebo group. A total of 290 patients completed the study. The average age of study participants ranged from 62.6 years (placebo group) to 63.5 years (84-mg group). The average amount of time patients had been living with diagnosed PD ranged from 95.7 months (84-mg group) to 97.4 months (placebo group). Their mean daily levodopa intake ranged from 818.6 mg (84-mg group) to 841.4 mg (placebo group). The total hours of daily OFF times reported in patient diaries ranged from 5.35 hours (84-mg group) to 5.59 hours (placebo group). Investigators instructed patients to treat up to 5 OFF periods per day. At least once during the 12-week treatment period, 26% of patients in the 84-mg group (n = 30) utilized the full 5 doses per day, and 50% (n = 57) of them utilized 4 doses per day at least once.52
The primary efficacy end point was defined as the change in UPDRS motor score from before taking the dose to 30 minutes after taking the dose. The least-squares mean difference between the 84-mg dose and placebo was found to be significant at –3.92 (–6.84 to –1.00; P = .0088).52
In both the 84-mg and 60-mg groups, there was a greater decrease in UPDRS motor scores than in the placebo group at all time points (range, 10-60 minutes) at the week-12 assessment. A total of 58% of patients in the 84-mg group (56 of 97 patients) had maintained response through 60 minutes versus 36% of patients in the placebo group (35 of 97 patients), which was a statistically significant difference (P = .0027). Patients in the 84-mg group also had a statistically significantly greater decrease in UPDRS motor scores at 30 minutes, compared with patients taking placebo (P = .0088).52
The inhalation powder formulation of levodopa was found to be generally well tolerated at both dose levels. Patients in the 84-mg and 60-mg groups had about the same number of AEs. The most common AE was cough, which occurred more commonly in the 84-mg and 60-mg groups than the placebo group and was typically considered mild or moderate in severity. Additional commonly reported AEs included upper respiratory tract infection, nausea, and sputum discoloration.52
Conclusions
Although levodopa remains a cornerstone of therapy for PD, significant limitations of sustained therapy include the near inevitability of OFF periods. The disability associated with OFF periods in turn leads to poor QOL, increased burden for patients and caregivers, and, ultimately, increased societal burden. Although treatments have been developed that reduce or avoid OFF periods, there still remains an unmet need for further therapeutic improvements with better benefit-to-risk AE profiles. Meeting this need successfully will require improved identification of OFF, starting with better education for both patients and practitioners, and addition of treatment approaches that can provide prompt relief of OFF periods while bridging the gap between medication doses.
Funding Source: Financial support for this work was provided by Acorda Therapeutics.
Author Affiliations: UCSF Weill Institute for Neurosciences, University of California, San Francisco.
Author Disclosures: Dr Tanner is an employee of the University of California – San Francisco, and the San Francisco Veterans Affairs Health Care System. She receives grants from the Michael J. Fox Foundation, the Parkinson’s Foundation, the Department of Defense, BioElectron, Roche/Genentech, Biogen Idec, and the National Institutes of Health; compensation for serving on data monitoring committees from Voyager Therapeutics, Intec Pharma, and Cadent Therapeutics; and personal fees for consulting from Neurocrine Biosciences, Adamas Therapeutics, Grey Matter, Acorda Therapeutics, Acadia, Amneal, and CNS Ratings.
Authorship Information: Concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; and critical revision of the manuscript for important intellectual content are attributed to Dr Tanner.
Address correspondence to: Caroline M. Tanner, MD, PhD, 212A Sandler Bldg, 675 Nelson Rising Lane, San Francisco, CA 94158. Email:
Caroline.Tanner@UCSF.edu.
REFERENCES
1. Poewe W, Seppi K, Tanner CM, et al. Parkinson disease. Nat Rev Dis Primers. 2017;3:17013. doi:10.1038/nrdp.2017.13
2. Feigin VL, Nichols E, Alam T, et al; GBD 2016 Neurology Collaborators. Global, regional, and national burden of neurological disorders, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(5):459-480. doi:10.1016/S1474-4422(18)30499-X
3. Marras C, Beck JC, Bower JH, et al. Prevalence of Parkinson’s disease across North America. NPJ Parkinsons Dis. 2018;4:21. doi:10.1038/s41531-018-0058-0
4. Savica R, Grossardt BR, Bower JH, Ahlskog JE, Rocca WA. Time trends in the incidence of Parkinson disease. JAMA Neurol. 2016;73(8):981-989. doi:10.1001/jamaneurol.2016.0947
5. Simon DK, Tanner CM, Brundin P. Parkinson disease epidemiology, pathology, genetics, and pathophysiology. Clin Geriatr Med. 2020;36(1):1-12. doi:10.1016/j.cger.2019.08.002
6. Racette BA, Searles Nielsen S, Criswell SR, et al. Dose-dependent progression of parkinsonism in manganese-exposed welders. Neurology. 2017;88(4):344-351. doi:10.1212/WNL.0000000000003533
7. Gao X, Chen H, Fung TT, et al. Prospective study of dietary pattern and risk of Parkinson disease. Am J Clin Nutr. 2007;86(5):1486-1494. doi:10.1093/ajcn/86.5.1486
8. Ritz B, Ascherio A, Checkoway H, et al. Pooled analysis of tobacco use and risk of Parkinson disease. Arch Neurol. 2007;64(7):990-997. doi:10.1001/archneur.64.7.990
9. Ross GW, Abbott RD, Petrovitch H, et al. Association of coffee and caffeine intake with the risk of Parkinson disease. JAMA. 2000;283(20):2674-2679. doi:10.1001/jama.283.20.2674
10. Yang F, Trolle Lagerros Y, Bellocco R, et al. Physical activity and risk of Parkinson’s disease in the Swedish National March cohort. Brain. 2015;138(pt 2):269-275. doi:10.1093/brain/awu323
11. Park JS, Davis RL, Sue CM. Mitochondrial dysfunction in Parkinson’s disease: new mechanistic insights and therapeutic perspectives. Curr Neurol Neurosci Rep. 2018;18(5):21. doi:10.1007/s11910-018-0829-3
12. Lesage S, Ibanez P, Lohmann E, et al. G2019S LRRK2 mutation in French and North African families with Parkinson’s disease. Ann Neurol. 2005;58(5):784-787. doi:10.1002/ana.20636
13. Ozelius LJ, Senthil G, Saunders-Pullman R, et al. LRRK2 G2019S as a cause of Parkinson’s disease in Ashkenazi Jews. N Engl J Med. 2006;354(4):424-425. doi:10.1056/NEJMc055509
14. Kitada T, Asakawa S, Hattori N, et al. Mutations in the parkin gene cause autosomal recessive juvenile parkinsonism. Nature. 1998;392(6676):605-608. doi:10.1038/33416
15. Valente EM, Abou-Sleiman PM, Caputo V, et al. Hereditary early-onset Parkinson’s disease caused by mutations in PINK1. Science. 2004;304(5674):1158-1160. doi:10.1126/science.1096284
16. Narendra DP, Min Jin S, Tanaka A, et al. PINK1 is selectively stabilized on impaired mitochondria to activate Parkin. PLoS Biol. 2010;8(1):e1000298. doi:10.1371/journal.pbio.1000298
17. Braak H, Del Tredici K, Rub U, de Vos RA, Jansen Steur EN, Braak E. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging. 2003;24(2):197-211. doi:10.1016/s0197-4580(02)00065-9
18. Pearce RKB, Hawkes CH, Daniel SE. The anterior olfactory nucleus in Parkinson’s disease. Mov Disord. 1995;10(3):283-287. doi:10.1002/mds.870100309
19. LeWitt PA. Levodopa therapy for Parkinson’s disease: pharmacokinetics and pharmacodynamics. Mov Disord. 2015;30(1):64-72. doi:10.1002/mds.26082
20. Fearnley JM, Lees AJ. Ageing and Parkinson’s disease: substantia nigra regional selectivity. Brain. 1991;114(pt 5):2283-2301. doi:10.1093/brain/114.5.2283
21. Damier P, Hirsch EC, Agid Y, Graybiel AM. The substantia nigra of the human brain. II. Patterns of loss of dopamine-containing neurons in Parkinson’s disease. Brain. 1999;122(pt 8):1437-1448. doi:10.1093/brain/122.8.1437
22. Postuma RB, Berg D, Stern M, et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord. 2015;30(12):1591-601. doi:10.1002/mds.26424
23. Goetz CG, Tilley BC, Shaftman SR, et al. Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord. 2008;23(15):2129-2170. doi:10.1002/mds.22340
24. Goetz CG, Fan S, Martinez-Martin P. MDS-UPDRS. The MDS-sponsored revision of the Unified Parkinson’s Disease Rating Scale. International Parkinson and Movement Disorder Society. Updated August 13, 2019. Accessed September 30, 2020. https://www.movementdisorders.org/MDS/MDS-Rating-Scales/MDS-Unified-Parkinsons-Disease-Rating-Scale-MDS-UPDRS.htm
25. Shulman LM, Taback RL, Bean J, Weiner WJ. Comorbidity of the nonmotor symptoms of Parkinson’s disease. Mov Disord. 2001;16(3):507-510. doi:10.1002/mds.1099
26. Sung VW, Nicholas AP. Nonmotor symptoms in Parkinson’s disease: expanding the view of Parkinson’s disease beyond a pure motor, pure dopaminergic problem. Neurol Clin. 2013;31(suppl 3):S1-S16. doi:10.1016/j.ncl.2013.04.013
27. Fasano A, Visanji NP, Liu LW, Lang AE, Pfeiffer RF. Gastrointestinal dysfunction in Parkinson’s disease. Lancet Neurol. 2015;14(6):625-639. doi:10.1016/S1474-4422(15)00007-1
28. Muller T, Palluch R, Jackowski J. Caries and periodontal disease in patients with Parkinson’s disease. Spec Care Dentist. 2011;31(5):178-181. doi:10.1111/j.1754-4505.2011.00205.x
29. Gabrielli M, Bonazzi P, Scarpellini E, et al. Prevalence of small intestinal bacterial overgrowth in Parkinson’s disease. Mov Disord. 2011;26(5):889-892. doi:10.1002/mds.23566
30. Fasano A, Bove F, Gabrielli M, et al. The role of small intestinal bacterial overgrowth in Parkinson’s disease. Mov Disord. 2013;28(9):1241-1249. doi:10.1002/mds.25522
31. Lin CW, Chang YC, Chen WS, Chang K, Chang HY, Wang TG. Prolonged swallowing time in dysphagic Parkinsonism patients with aspiration pneumonia. Arch Phys Med Rehabil. 2012;93(11):2080-2084. doi:10.1016/j.apmr.2012.07.010
32. Salat D, Tolosa E. Levodopa in the treatment of Parkinson’s disease: current status and new developments. J Parkinsons Dis. 2013;3(3):255-269. doi:10.3233/JPD-130186
33. Fox SH, Katzenschlager R, Lim SY, et al; Movement Disorder Society Evidence-Based Medicine Committee. International Parkinson and Movement Disorder Society evidence-based medicine review: update on treatments for the motor symptoms of Parkinson’s disease. Mov Disord. 2018;33(8):1248-1266. doi:10.1002/mds.27372
34. Dewey RB Jr. Management of motor complications in Parkinson’s disease. Neurology. 2004;62(6 suppl 4):S3-S7. doi:10.1212/wnl.62.6_suppl_4.s3
35. Okun MS. Deep-brain stimulation for Parkinson’s disease. N Engl J Med. 2012;367(16):1529-1538. doi:10.1056/NEJMct1208070
36. Chou KL, Stacy M, Simuni T, et al. The spectrum of “OFF” in Parkinson’s disease: what have we learned over 40 years? Parkinsonism Relat Disord. 2018;51:9-16. doi:10.1016/j.parkreldis.2018.02.001
37. Pierantozzi M, Pietroiusti A, Brusa L, et al. Helicobacter pylori eradication and L-dopa absorption in patients with PD and motor fluctuations. Neurology. 2006;66(12)1824-1829. doi:10.1212/01.wnl.0000221672.01272.ba
38. Thanvi B, Lo N, Robinson T. Levodopa-induced dyskinesia in Parkinson’s disease: clinical features, pathogenesis, prevention and treatment. Postgrad Med J. 2007;83(980):384-388. doi:10.1136/pgmj.2006.054759
39. Ahlskog JE, Muenter MD. Frequency of levodopa-related dyskinesias and motor fluctuations as estimated from the cumulative literature. Mov Disord. 2001;16(3):448-458. doi:10.1002/mds.1090
40. Hauser RA, Deckers F, Lehert P. Parkinson’s disease home diary: further validation and implications for clinical trials. Mov Disord. 2004;19(12):1409-1413. doi:10.1002/mds.20248
41. Isaacson S, Lew M, Ondo W, Hubble J, Clinch T, Pagan F. Apomorphine subcutaneous injection for the management of morning akinesia in Parkinson’s disease. Mov Disord Clin Pract. 2017;4(1):78-83. doi:10.1002/mdc3.12350
42. Swope DM. Rapid treatment of “wearing off” in Parkinson’s disease. Neurology. 2004;62(6 suppl 4):S27-S31. doi:10.1007/s00415-005-4009-4
43. Levit AV, Zebendon C, Walter L, O’Donnell P, Marras C. Communication gaps about OFF periods between physicians and patients with Parkinson’s disease: a patient–physician dialogue analysis. Res Rev in Parkinsonism. 2019;9:3-8. doi:10.2147/JPRLS.S188923
44. Storch A, Schneider CB, Wolz M, et al. Nonmotor fluctuations in Parkinson disease: severity and correlation with motor complications. Neurology. 2013;80(9):800-809. doi:10.1212/WNL.0b013e318285c0ed.
45. Armstrong MJ, Rastgardani T, Gagliardi AR, Marras C. The experience of off periods: qualitative analysis of interviews with persons with Parkinson’s and carepartners. Clin Park Relat Disord. 2019(1);31-36.
46. Stocchi F, Antonini A, Barone P, et al; DEEP study group. Early DEtection of wEaring off in Parkinson disease: the DEEP study. Parkinsonism Relat Disord. 2014;20(2):204-211. doi:10.1016/j.parkreldis.2013.10.027
47. Chapuis S, Ouchchane L, Metz O, Gerbaud L, Durif F. Impact of the motor complications of Parkinson’s disease on the quality of life. Mov Disord. 2005;20(2):224-230. doi:10.1002/mds.20279
48. Rastgardani T, Armstrong MJ, Gagliardi AR, Grabovsky A, Marras C. Communication about OFF periods in Parkinson’s disease: a survey of physicians, patients, and carepartners. Front Neurol. 2019;10:892. doi:10.3389/fneur.2019.00892
49. Matthews H, Stamford J, Saha R, Martin A; Off-Park survey steering group. Exploring issues around wearing-off and quality of life: the OFF-PARK survey of people with Parkinson’s disease and their care partners. J Parkinsons Dis. 2015;5(3):533-539. doi:10.3233/JPD-150547
50. Fahn S. How do you treat motor complications in Parkinson’s disease: medicine, surgery, or both? Ann Neurol. 2008;64(suppl 2):S56-S64. doi:10.1002/ana.21453
51. Inbrija (levodopa inhalation powder). Prescribing information. Acorda Therapeutics Inc; 2020. Accessed September 30, 2020. https://www.inbrija.com/prescribing-information.pdf
52. LeWitt PA, Hauser RA, Pahwa R, et al; SPAN-PD Study Investigators. Safety and efficacy of CVT-301 (levodopa inhalation powder) on motor function during off periods in patients with Parkinson’s disease: a randomised, double-blind, placebo-controlled phase 3 trial. Lancet Neurol. 2019;18(2):145-154. doi:10.1016/S1474-4422(18)30405-8
53. DeMaagd G, Philip A. Parkinson’s disease and its management: part 4: treatment of motor complications. P t. 2015;40(11):747-773.
54. Apokyn (apomorphine hydrochloride injection). Prescribing information. US WorldMeds LLC; 2020. Accessed September 30, 2020. https://www.apokyn.com/sites/all/themes/apokyn/content/resources/Apokyn_PI.pdf
55. Duopa (carbidopa and levodopa) enteral suspension. Prescribing information. AbbVie Inc; 2020. Accessed September 30, 2020. rxabbvie.com/pdf/duopa_pi.pdf#page=1
56. Comtan (entacapone) tablets. Prescribing information. Novartis; 2018. Accessed July 9, 2020. https://www.pharma.us.novartis.com/sites/www.pharma.us.novartis.com/files/comtan.pdf
57. Stalevo (carbidopa, levodopa, and entacapone) tablets. Prescribing information. Novartis; 2019. Accessed September 30, 2020. https://www.pharma.us.novartis.com/sites/www.pharma.us.novartis.com/files/stalevo.pdf
58. Xadago (safinamide) tablets. Prescribing information. US WorldMeds LLC; 2019. Accessed September 30, 2020. http://xadago.com/XADAGO_FullPI.pdf
59. Nourianz (istradefylline) tablets. Prescribing information. Kyowa Kirin Inc; 2020. Accessed September 30, 2020. https://www.nourianzhcp.com/assets/pdf/nourianz-full-prescribing-information.pdf
60. Burack M, Aldred J, Zadikoff C, et al. Implementing levodopa-carbidopa intestinal gel for Parkinson disease: insights from US practitioners. Mov Disord Clin Pract. 2018;5(4):383-393. doi:10.1002/mdc3.12630
61. Fernandez HH, Standaert DG, Hauser RA, et al. Levodopa-carbidopa intestinal gel in advanced Parkinson’s disease: final 12-month, open-label results. Mov Disord. 2015;30(4):500-9. doi:10.1002/mds.26123
62. Carbone F, Djamshidian A, Seppi K, Poewe W. Apomorphine for Parkinson’s disease: efficacy and safety of current and new formulations. CNS Drugs. 2019;33(9):905-918. doi:10.1007/s40263-019-00661-z
63. Lipp MM, Batycky R, Moore J, Leinonen M, Freed MI. Preclinical and clinical assessment of inhaled levodopa for OFF episodes in Parkinson’s disease. Sci Transl Med. 2016;8(360):360ra136. doi:10.1126/scitranslmed.aad8858

