- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
The Clinical and Economic Benefits Associated With Novel Multi-Cancer Early Detection Tests: Conference Highlights from the 2022 ISPOR Annual Meeting
To claim CE credit for this activity, please visit https://www.pharmacytimes.org/courses/the-clinical-and-economic-benefits-associated-with-novel-multi-cancer-early-detection-tests-conference-highlights-from-the-2022-ispor-annual-meeting
Introduction
Despite decades of advancements in cancer prevention and treatment, cancer remains the second most common cause of death in the United States. In 2022, approximately 609,360 people are expected to die from cancer, although that number is predicted to climb given the impact of the COVID-19 pandemic on preventive screenings and early diagnosis and treatment. Estimates based on 2018 and 2019 statistics predict 1.9 million new cases of cancer will be diagnosed in 2022.1
Cancer carries a high economic cost, with overall expenditures in 2020 of more than $200 billion.2 Yet while the United States spends more per capita on cancer care, a comparison with 22 other countries found it had a higher mortality rate than 9 others.2
The overall age-adjusted cancer death rate from fell 32% between 1991 and 2019. However, just 4 cancers—lung, breast, colorectal, and prostate—all of which have screening protocols either on a population basis or for certain high-risk groups, account for most of that decline. Improvements in survival rates for other cancers, particularly ovarian, pancreatic, and liver, have been much smaller.1
Cancers without recommended screening tests account for 71% of cancer deaths in the United States.3 The incidence rate of those cancers increased 1.2% between 2000 and 2018, while there was no significant change in cancers with guideline-recommended screenings. Among those aged 50 years and older, incidence rates of cancers without guideline-recommended screenings remained constant, while rates fell 0.1% per year for those with screenings.4
Detecting cancers as early as possible, when treatment is more likely to be successful, is an important way to reduce overall cancer mortality.5 Earlier diagnoses can also result in significant economic savings.One study found an absolute mean cost for women diagnosed with stage I ovarian cancer of $73,428; by stage IV, the cost increased to $227,899, a more than 4-fold difference. Costs for colorectal cancer doubled, from $129,645 when diagnosed in stage I to $271,216 when diagnosed in stage IV.6 Thus, earlier diagnosis could have economic as well as lifesaving benefits, provided it is not associated with a high burden of overdiagnosis and overtreatment.7,8
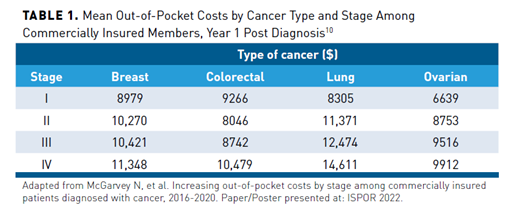
Patients with cancer shoulder a significant part of the economic burden, with an estimated $16 billion in out-of-pocket expenses to diagnose and treat their cancer in 2020.9 The more advanced the presentation of cancer, the higher those costs. A study presented at the 2022 International Society for Pharmacoeconomics and Outcomes Research (ISPOR) Annual Meeting assessed out-of-pocket costs (co-insurance, co-pay, and deductible) for the first year after diagnosis for 6028 commercially insured patients with cancer, the majority of whom had breast cancer. Those diagnosed with stage I breast cancer had mean costs of $8979 while those diagnosed with stage IV encountered mean out-of-pocket costs of $11,348 (P <.001) The results were similar for ovarian, lung, and colorectal cancers (Table 110). The authors suggested that earlier diagnosis could reduce patient financial burden by requiring less intensive treatment and management.10
The stage at which cancer is diagnosed affects employment status in patients who are still working. An analysis of claims from more than 1.2 million commercially insured patients aged 18 to 64 years found a median time to reduction in employment status of 14.7 months in those diagnosed in the earlier stages (n = 141,440) and 4.3 months in those diagnosed with metastatic cancer (n = 17,875 [P <.001]). These differences were observed regardless of cancer type.11
Cancer Detection: Current Screening
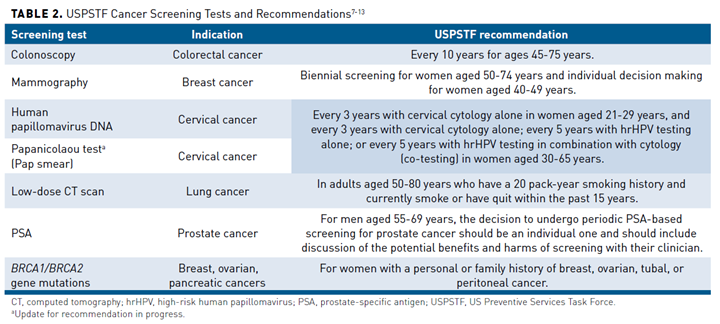
The US Preventive Services Task Force (USPSTF), an independent, volunteer panel of national experts in disease prevention and evidence-based medicine that makes evidence-based recommendations about clinical preventive services, currently recommends population-based screening for breast, colorectal, and cervical cancers, with prostate cancer screening based on a discussion of the potential harms and benefits.12-15 It also recommends screening certain smokers for lung cancer.12Table 27-13 contains a summary of cancer screening tests and recommendations from the USPSTF.
The Task Force’s decisions on screening recommendations are based on 4 factors (Figure 115):
- Evidence related to benefits and harms from randomized clinical trials and observational studies.
- Whether benefits outweigh harms and, if so, by how much and in which populations.
- The degree of certainty the evidence provides for both benefits and harms.
- Ages and other risk factors needed to specify when to begin and when to stop offering the service and in which populations.

There are different well-recognized guidelines and recommendations but there may be variations when compared with the USPSTF recommendations; one example pertains to prostate cancer, for which recommendations from the American Cancer Society are also widely accepted and recommendations vary based on age and risk.1 Despite available guidelines, screening uptake in the United States remains low. Numerous barriers exist, including financial, educational, psychosocial, and logistical. Others include a lack of provider recommendations as well as a lack of trust in the healthcare system.16-19 Pre-pandemic screenings for certain cancers had already been declining, even among insured individuals.20 Those declines were even higher among those with low socioeconomic status and no insurance. For example, women without health insurance had a 26% to 39% lower prevalence of breast cancer screening compared with those with insurance.20 During the pandemic, screening rates for all cancers plummeted, leaving providers warning of a coming tsunami of later-stage cancer diagnoses.1,19,21,22
False-positive results add another layer of complexity to the decision to recommend population-based screening. For instance, false-positive rates for low-dose computed tomography (LDCT) screening in smokers have been reported as high as 26.6%.23-25 Nearly half of women who undergo an annual mammography will have at least 1 false-positive test over 10 years, with some studies estimating rates between 29% and 77%.26,27
False-positive results elicit significant anxiety in patients, particularly those with a high risk of cancer.28,29 It can also lead to significantly higher medical costs due to biopsies and scans to rule out cancer.30
Multi-Cancer Early Detection Tests
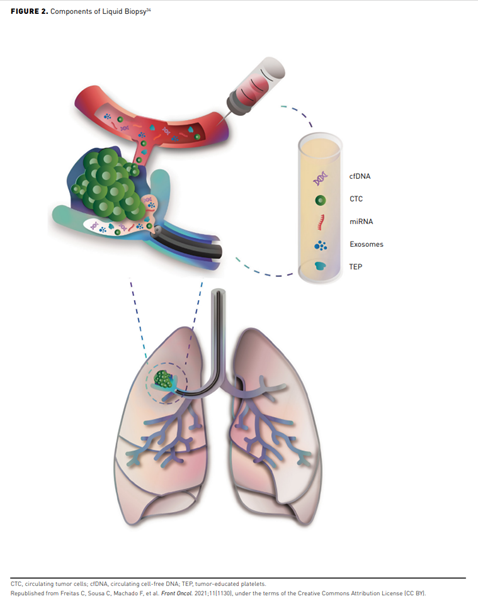
The use of blood tests to screen maternal blood for DNA evidence of fetal abnormalities ushered in the potential of similar screening tests for cancer when the pregnancy tests also picked up DNA evidence of maternal neoplasms.28This spurred the development of several multi-cancer early detection (MCED) blood tests that could be used to identify dozens of cancers at earlier stages, including those without routine screening tests.31-33 The tests often combine artificial intelligence (AI) and machine learning with assays to detect a variety of circulating analytes, typically cell-free DNA (cfDNA), for early indications of cancer (Figure 234).
MCED tests offer several advantages, including potentially greater accessibility than more complicated, organ-specific tests. There is even some thought that they could help reduce cancer-related racial disparities by eliminating the need for access to specialists for screening and ensuring consistent quality and accuracy of test results. However, the opposite could also be true if uptake is low in minority communities and/or there is a lack of insurance coverage.35
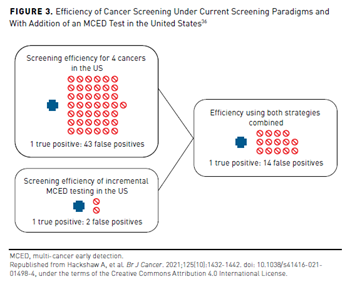
One study estimating the impact of adding MCED screening to standard population-based screenings for breast, cervical, colorectal, and lung cancers predicted it would result in a diagnosis of an additional 105,526 cancers with a 25% uptake and an additional 189,498 cancers with a 100% uptake. The estimated true-positive/false-positive (TP/FP) rate with current screening was 1.43 (43 false positives for every person diagnosed with cancer) at a cost of $89,042 to confirm there was no cancer versus 1:1.8 using the MCED test at a cost of $7060 (Figure 336).
While MCED tests have low false-positive rates, there is concern they could increase the diagnosis of indolent cancers that may never impact the mortality of the patient or precancers that never develop into cancer or cause symptoms.31,36,37 Large clinical trials have been conducted for 3 MCED tests.
Galleri
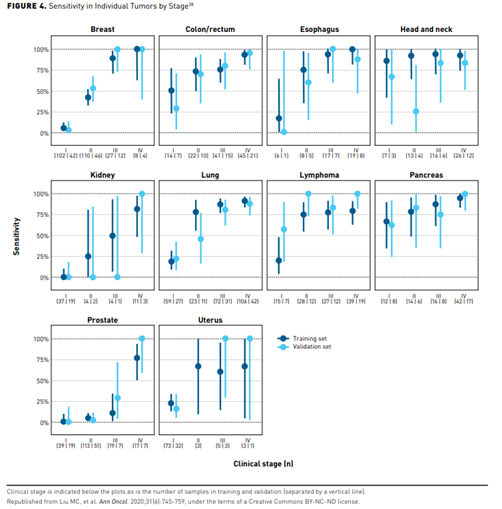
Galleri examines cfDNA methylation patterns across a very large number of methylation sites and uses AI analysis to recognize patterns associated with the presence of cancer as well as the likely organ of origin of the suspected malignancy. It has been shown to detect more than 50 cancers.38 Figure 438 depicts its sensitivity in individual tumors by stage.
Galleri is currently marketed in the United States under a Clinical Laboratory Improvement Amendments (CLIA) waiver and is intended for use in those older than 50 years with and without additional risk factors for cancer in conjunction with currently recommended screenings.3,39 It has received Breakthrough Device Designation from the Food and Drug Administration (FDA).40 Clinical trials assessing the clinical utility of the test are ongoing and there are plans to seek FDA approval in 2023.
Galleri has been evaluated in several studies, including the Circulating Cell-free Genome Atlas (CCGA), a prospective, multicenter, case-control, observational study conducted with specimens from 15,254 participants, 56% of whom had suspected cancer,41,42 and the PATHFINDER trial, a prospective study in 6629 adults aged 50 years and older designed to evaluate the role of the test in clinical practice.31 Publications from the CCGA trial report up to 100% specificity (no false positives) in a group of confirmed, cancer-free patients and a 46.7% cancer detection accuracy among patients with confirmed cancer. The test detected 78.9% of cancers in stage II with tumor of origin predicted in all samples with a 97.1% accuracy.41 A sub-study in 6689 participants (2482 with cancer) found a 99.3% specificity overall for more than 50 cancers.43 Participants in CCGA continue to be followed.
The PATHFINDER study provided a real-world scenario to evaluate the potential use of MCED tests. In this study, the participant and the physician received the results and the physician determined the diagnostic pathway. The goal was to identify the most effective approach to achieve diagnostic certainty after a cancer “signal” from the test. Interim results showed a cancer signal in 92 participants (1.4%), of which 29 had a true positive and 36 had a false positive after imaging and procedures, resulting in a positive predictive value of 45%. The cancer signal origin prediction was 100% when predicting the first or second stage of cancer of origin in those with an elevated cancer risk (smoking history, history of prior cancer treatment completed more than 3 years ago, or genetic predisposition to cancer; 95% CI, 83.2-100) and 87.5% in those without a higher cancer risk (CI, 52.9-99.4). It took about 50 days to diagnostic resolution from the time the test results were returned. The majority of cancers detected were diagnosed at stages I-III. The study has closed accrual with final analysis still pending.31
A follow-up study, PATHFINDER 2, is a currently accruing multicenter clinical trial. With an estimated sample size of 10,000 participants older than 50 years, the investigators aim to evaluate the safety of the MCED test in terms of diagnostic testing triggered by the MCED test result as well as the performance of the MCED test in individuals eligible for cancer screening.44
CancerSEEK
The CancerSEEK test detects the presence of prespecified DNA mutation and protein markers associated with cancer. It is designed as a 2-step process, with a second test to validate the results of the first in the case of an initial positive result.
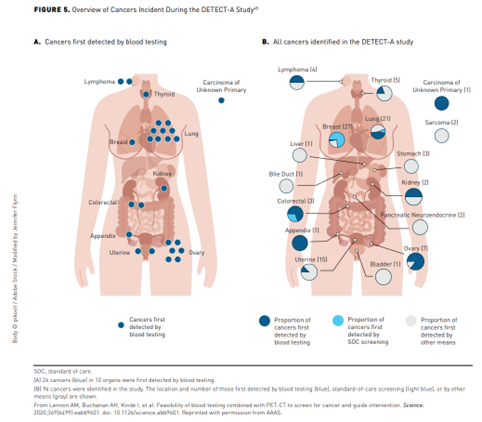
In the DETECT-A trial, 9911 healthy women aged 65 to 75 years with no personal history of cancer and a high adherence to recommended screening guidelines received the CancerSEEK MCED test coupled with positron emission tomography/CT imaging if both the baseline and confirmatory CancerSEEK test were positive. The study investigators chose to enroll only women to enrich for ovarian cancer, a malignancy that currently lacks standard-of-care (SOC) screening and typically has a favorable prognosis only when detected early.45
Of 9911 women screened, 490 (4.9%) had positive baseline testing, and 127 (1.3%) had confirmation on the second test. After the second test, 64 women had imaging concerning for cancer, with ultimately 26 cancers confirmed by biopsy (6 ovarian). All patients were followed closely for 1 year, during which time an additional 67 cancers were observed in women who had a negative baseline CancerSEEK test (22 detected with SOC screening and 45 detected by other means) (Figure 545).
The DETECT-ASCEND 2 study is an actively enrolling clinical trial aiming to further refine the CancerSEEK MCED test in 21,000 patients older than 50 years in 2 different cohorts of healthy volunteers with no cancer history and those with recently diagnosed but untreated cancers.
DELFI
The DELFI test is based on fragmentomes, disordered DNA packaging in cancer cells, and uses machine learning algorithms to assess patterns. It was evaluated in the 7-year LUCAS trial, which prescreened 365 individuals at high risk for lung cancer to determine if they should undergo LDCT screening. The combination of the test plus LDCT detected 90% of lung cancers, including 80% of stage I cancers, and reduced the number of unnecessary LDCTs by half.33
An earlier study analyzed fragmentation profiles of 236 patients with breast, colorectal, lung, ovarian, pancreatic, gastric, or bile duct cancer and 245 healthy individuals. It found a sensitivity ranging from 57% to 99% among the 7 cancers with a 98% specificity. Overall, it detected cancer in 91% of the patients with cancer.46 Several trials are also underway using MCED screening for colorectal cancer.42,47,48
Managed Care Implications of MCED Tests
Managed care providers must consider several issues, including economic, clinical, and psychosocial, when determining coverage of MCED tests. Clinical trial participation is strongly recommended if a patient is interested in one of these MCED tests. However, if a patient chooses not to participate in a clinical trial, the cost is expected to be about $1000, with Galleri currently sold in the United States at $949 per test.49
An estimated 120 million people in the United States are 50 years or older.50 If half of these individuals were tested, the cost for the tests alone would approach $60 billion, with additional costs for testing and treatment in those with identifiable cancers. It is also not clear how often the tests might be given or their impact on current screening uptake. In addition, because follow-up diagnostic tests will be required to confirm initial test results, patients may face significant out-of-pocket costs.51,52
Nonetheless, bipartisan bills in the US House of Representatives and Senate would require Medicare coverage of the tests once they are approved by the FDA.53 The economics of MCED tests are based on modeling since the tests are not yet in wide use. They also must use certain assumptions about the potential outcomes of the tests to reduce cancer-related deaths and treatment as no studies have yet evaluated this issue.
An abstract presented at ISPOR 2022 suggested using a mixture cure model, often used to determine cure fractions due to cancer pharmacologic therapies, to assess the economic impact of earlier cancer diagnosis. One advantage is that it allows for more robust calculation of costs attributable to cancer by isolating end-of-life costs from patients who do not die from cancer. Using this approach, the authors aggregated reductions in cancer-attributable costs after incorporating cure fraction versus no cure fraction of −26.5%, −9.45%, and −0.5% for local, regional, and distant, respectively.54
There are concerns that making MCED tests part of Medicare’s annual screening benefit could overwhelm the healthcare system due to the current cost per test plus the cost of follow-up scans and biopsies.55 An abstract presented at ISPOR 2022 modeled the potential of a value-based price (VBP) for an MCED test in a Medicare population. The model predicted that the proportion of cancers detected at stage IV would decline from 20.4% to 10.7%; patients diagnosed with an MCED test as well as SOC screening would have on average $5397 less in cancer-related treatment and diagnosis costs versus SOC screening alone. However, the model did not include the cost of the MCED test (which ranged from $730 to $1771 per test) or additional workup costs to confirm the diagnosis. At willingness-to-pay (WTP) thresholds of $50,000/QALY to $150,000/QALY, the authors concluded that VBP in this population was sensitive to the number of clinically significant cancers detected.56
A Markov model comparing an annualMCED test plus SOC screening in US adults aged 50 to 79 years predicted that 10.7% of cancers would be detected at stage IV by adding an MCED test compared with 20.4% with SOC screening. The combined screening method led to 0.17 more QALYs and reduced cancer-related treatment and diagnosis costs by $5208. At a WTP threshold of $50,000/QALY, the VBP would be $923 per test; at a WTP threshold of $150,000/QALY, the VBP would be $2069.11,57
Another health economic model comparing the clinical outcomes of adding an MCED test to current cancer screening versus current screening alone over a lifetime in people aged 50 to 79 years found those receiving an MCED test had an incremental gain of 0.35 life-years and 0.34 QALYs per person, primarily due to earlier detection of cancers and improved mortality. At WTP thresholds of $100,000/QALY to $150,000/QALY, that translated to a cost benefit of $34,400 to $51,600 per person, respectively.58
A study estimating the impact of adding MCED screening for breast, cervical, colorectal, and lung cancers to current screening modalities estimated it would detect an additional 105,526 of these and other cancers with a 25% uptake and 422,105 with a 100% uptake. The estimated TP/FP ratio, which demonstrates how many patients without cancer should undergo diagnostic evaluation to detect 1 person with cancer, was 1:43 ($89,042 per cancer detected) with the 4 SOC tests and 1:1.8 with MCED ($7060 per cancer detected). Combining both yielded a TP/FP ratio of 1:14 in the United States, with diagnostic costs per cancer of $32,461.36
The authors noted that while reported sensitivities for MCED tests tended to be lower than currently used screening tests, potential advantages could be that they cover multiple cancers and have a relatively low false-positive rate. They also noted that a single test could help overcome the high rates of nonadherence seen in the United States.36
Another consideration is that the lower false-positive rates of MCEDs could reduce patient anxiety as well as costs.30,59 The results of a vignette-based utility elicitation study presented at ISPOR 2022, in which participants completed the time-tradeoff utility interviews, found a true negative had the highest utility at 0.978 (SD 0.028), as might be expected. Among scenarios with false positives, the scenario in which the test delivered a false-positive result for breast cancer but no biopsy was performed had the highest utility at 0.958 (SD 0.016), while a false-positive result for lung cancer with a follow-up CT scan at 6 months had the lowest utility (0.847 [SD 0.122]).60
There are other considerations beyond the cost of the tests.61 For instance, it should be considered whether the test be applied only to those at high risk of developing certain cancers or with known risk factors, such as obesity. Discussions should include when they begin and how often they should be received. Additionally, it must be determined how the tests will integrate with existing screening protocols. Assessment of potential psychological effects of early multi-cancer detection should be addressed and involve detailed patient monitoring. Other considerations include follow-up protocols for patients with positive tests; use of the tests in patients whose cancer is in remission; and the need for large-scale, real-world studies to determine their utility in reducing deaths from cancer and their impact on patients.61
The National Cancer Institute plans to launch a large trial within the next 2 years to evaluate these and other questions using several MCED tests. The trial will be designed using feedback from a 2021 workshop the agency held with research leaders.62
Conclusions
Cancer continues to be a leading cause of mortality in the United States, second only to cardiovascular disease. While the overall cancer-related mortality has fallen by one-third since 1991, much of that decline occurred in just 4 cancers, lung, breast, colorectal, and prostate, for which there are screening protocols in place. The majority of other cancers are diagnosed in later stages, at which time treatments are typically less effective. It is clear from decades of research that early detection is associated with improved prognosis and survival. However, the USPSTF recommends widespread screening for just 4 types of cancers listed previously. There are no recommended screening tests for cancers that cause 71% of all cancer-related deaths. In addition, screening rates remain below national targets, with several barriers to population-based screening.
Clinical studies show that MCED tests can identify multiple cancers early, including those that lack screening tests. This has the potential to reduce mortality rates and overall direct and indirect healthcare costs. The use of noninvasive MCEDs to screen for multiple cancers simultaneously may improve early diagnosis of many cancers. The evidence is strong as to their specificity and sensitivity; yet, despite the clinical efficacy of these tests, at this time there is no evidence that they can prevent deaths or reduce cancer-related costs. These data, along with policy discussions regarding coverage, frequency of use, accessibility, and other issues, are needed.
Author affiliation: Nima Nabavizadeh, MD, is Associate Professor, Department of Radiation Medicine atOregon Health & Science University, Portland, OR.
Funding source: This activity is supported by an educational grant from GRAIL, Inc.
Author disclosure: Dr Nabavizadeh has no relevant financial relationships with commercial interests to disclose.
Author information: Substantial contributions to analysis and interpretation of data, critical revision of the manuscript for important intellectual content, and supervision.
Address correspondence to: nabaviza@ohsu.edu
Medical writing and editorial support provided by: Debra Gordon, MS
REFERENCES
- American Cancer Society (ACS). Cancer Facts and Figures, 2022. ACS; 2022. Accessed July 25, 2022. www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2022/2022-cancer-facts-and-figures.pdf
- Chow RD, Bradley EH, Gross CP. Comparison of cancer-related spending and mortality rates in the US vs 21 high-income countries. JAMA Health Forum. 2022;3(5):e221229-e221229. doi: 10.1001/jamahealthforum.2022.1229
- Securities and Exchange Commission. Form S-1 Registration Statement: GRAIL, Inc. Published September 9, 2020. Accessed July 18, 2022. www.sec.gov/Archives/edgar/data/1699031/000162827920000227/grails-1.htm
- Kim A, Cong Z, Cohen SS. Time trend of incidence rates in cancers with and without commonly adopted guideline-recommended screening (CGRS) in the United States, 2000-2018. Paper presented at: ISPOR 2022. grail.com/wp-content/uploads/2022/05/Kim_ISPOR-2022_Cancer-Burden-Over-Time_Poster_FINAL.pdf
- Clarke CA, Hubbell E, Kurian AW, Colditz GA, Hartman A-R, Gomez SL. Projected reductions in absolute cancer–related deaths from diagnosing cancers before metastasis, 2006–2015. Cancer Epidemiol Biomarkers Prev. 2020;29(5):895-902. doi: 10.1158/1055-9965.EPI-19-1366
- McGarvey N, Gitlin M, Qi J, Chung KC. Increasing healthcare costs by stage and over time among patients diagnosed with cancer: 2008-2020. Paper presented at: AMCP Nexus 2021 Virtual. grail.com/wp-content/uploads/2021/10/AMCP_Nexus_2021_Cost_by_Cancer_Type_and_Stage_FINAL.pdf
- Kakushadze Z, Raghubanshi R, Yu W. Estimating cost savings from early cancer diagnosis. Data. 2017;2(30):2-16. doi: 10.3390/data2030030
- Guide to Cancer Early Diagnosis. World Health Organization;2017. Accessed July 25, 2022. apps.who.int/iris/handle/10665/254500
- Yabroff KR, Mariotto A, Tangka F, et al. Annual report to the nation on the status of cancer, part 2: patient economic burden associated with cancer care. J Natl Cancer Inst. 2021;113(12):1670-1682. doi: 10.1093/jnci/djab192
- McGarvey N, Gitlin M, Fadli ES, Chung KC. Increasing out-of-pocket costs by stage among commercially insured patients diagnosed with cancer, 2016-2020. Paper presented at: ISPOR 2022. Accessed August 3, 2022. www.ispor.org/heor-resources/presentations-database/presentation/intl2022-3460/115321
- Cong Z, Tran O, Nelson J, Silver M, Chung KC. Employment decrease among patients newly diagnosed with early versus late-stage cancers in the US. Paper presented at: ISPOR 2022. Accessed August 3, 2022. www.ispor.org/heor-resources/presentations-database/presentation/intl2022-3461/115880
- A and B recommendations. United States Preventive Services Task Force (USPSTF). Updated 2021. Accessed July 9, 2022. www.uspreventiveservicestaskforce.org/uspstf/recommendation-topics/uspstf-and-b-recommendations
- Prostate cancer screening. USPSTF. Published May 8, 2018. Accessed July 23, 2022. www.uspreventiveservicestaskforce.org/uspstf/recommendation/prostate-cancer-screening
- Grossman DC, Curry SJ, Owens DK, et al. Screening for prostate cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;319(18):1901-1913. doi: 10.1001/jama.2018.3710
- Use of decision models in the development of evidence-based clinical preventive services recommendations. USPSTF. Published May 2019. Accessed June 9, 2022. www.uspreventiveservicestaskforce.org/uspstf/about-uspstf/methods-and-processes/use-decision-models-development-evidence-based-clinical-preventive-services-recommendations
- Castro S, Sosa E, Lozano V, et al. The impact of income and education on lung cancer screening utilization, eligibility, and outcomes: a narrative review of socioeconomic disparities in lung cancer screening. J Thorac Dis. 2021;13(6):3745-3757. doi: 10.21037/jtd-20-3281
- Moss JL, Leach K, Stoltzfus KC, et al. Multilevel associations with cancer screening among women in rural, segregated communities within the northeastern USA: a mixed-methods study. J Cancer Educ. 2021:1-11. doi: 10.1007/s13187-021-02069-0
- Moss JL, Popalis M, Ramirez SI, Reedy-Cooper A, Ruffin MT. Disparities in cancer screening: the role of county-level metropolitan status and racial residential segregation. J Community Health. 2021;47(1):168-178. doi: 10.1007/s10900-021-01035-7
- Zhu X, Parks PD, Weiser E, Jacobson DJ, Limburg PJ, Finney Rutten LJ. Barriers to utilization of three colorectal cancer screening options - data from a national survey. Prev Med Rep. 2021;24:101508. doi: 10.1016/j.pmedr.2021.101508
- Benavidez GA, Zgodic A, Zahnd WE, Eberth JM. Disparities in meeting USPSTF breast, cervical, and colorectal cancer screening guidelines among women in the United States. Prev Chronic Dis. 2021;18:E37. doi: 10.5888/pcd18.200315
- Chen RC, Haynes K, Du S, Barron J, Katz AJ. Association of cancer screening deficit in the united states with the COVID-19 pandemic. JAMA Oncol. 2021;7(6):878-884. doi: 10.1001/jamaoncol.2021.0884
- Knoll K, Reiser E, Leitner K, et al. The impact of COVID-19 pandemic on the rate of newly diagnosed gynecological and breast cancers: a tertiary center perspective. Arch Gynecol Obstet. 2022;305(4):945-953. doi: 10.1007/s00404-021-06259-5
- Pinsky PF, Bellinger CR, Miller DP, Jr. False-positive screens and lung cancer risk in the National Lung Screening Trial: implications for shared decision-making. J Med Screen. 2018;25(2):110-112. doi: 10.1177/0969141317727771
- Pinsky PF, Gierada DS, Black W, et al. Performance of lung-RADS in the National Lung Screening Trial: a retrospective assessment. Ann Intern Med. 2015;162(7):485-491. doi: 10.7326/M14-2086
- Thalanayar PM, Altintas N, Weissfeld JL, Fuhrman CR, Wilson DO. Indolent, potentially inconsequential lung cancers in the Pittsburgh Lung Screening Study. Ann Am Thorac Soc. 2015;12(8):1193-1196. doi: 10.1513/AnnalsATS.201412-577OC
- Elmore JG, Barton MB, Moceri VM, Polk S, Arena PJ, Fletcher SW. Ten-year risk of false positive screening mammograms and clinical breast examinations. N Engl J Med. 1998;338(16):1089-1096. doi: 10.1056/NEJM199804163381601
- Hubbard RA, Kerlikowske K, Flowers CI, Yankaskas BC, Zhu W, Miglioretti DL. Cumulative probability of false-positive recall or biopsy recommendation after 10 years of screening mammography: a cohort study. Ann Intern Med. 2011;155(8):481-492. doi: 10.7326/0003-4819-155-8-201110180-00004
- Domínguez-Vigil IG, Moreno-Martínez AK, Wang JY, Roehrl MHA, Barrera-Saldaña HA. The dawn of the liquid biopsy in the fight against cancer. Oncotarget. 2018;9(2):2912-2922. doi: 10.18632/oncotarget.23131
- Kim A, Chung KC, Kier C, Patrick D. Patient-reported outcomes associated with cancer screening: a systematic review. Paper presented at: ISPOR 2021; Virtual. Accessed August 3, 2022. www.ispor.org/heor-resources/presentations-database/presentation/intl2021-3339/110551
- Lafata JE, Simpkins J, Lamerato L, Poisson L, Divine G, Johnson CC. The economic impact of false-positive cancer screens. Cancer Epidemiol Biomarkers Prev. 2004;13(12):2126-2132.
- Beer TM, McDonnell CH, Nadauld L, et al. Interim results of PATHFINDER, a clinical use study using a methylation-based multi-cancer early detection test. Paper presented at: American Society of Clinical Oncology (ASCO) Annual Meeting. June 2021; Virtual. Accessed August 3, 2022. ascopubs.org/doi/abs/10.1200/JCO.2021.39.15_suppl.3010
- Chen X, Dong Z, Hubbell E, et al. Prognostic significance of blood-based multi-cancer detection in plasma cell-free DNA. Clin Cancer Res. 2021;27(15):4221-4229. doi: 10.1158/1078-0432.CCR-21-0417
- Mathios D, Johansen JS, Cristiano S, et al. Detection and characterization of lung cancer using cell-free DNA fragmentomes. Nat Commun. 2021;12(1):5060. doi: 10.1038/s41467-021-24994-w
- Freitas C, Sousa C, Machado F, et al. The role of liquid biopsy in early diagnosis of lung cancer. Front Oncol. 2021;11(1130):634316. doi: 10.3389/fonc.2021.634316
- Ward AS, Van Nuys K, Lakdawalla D. Reducing racial disparities in early cancer diagnosis with blood-based tests. Leonard D. Schaeffer Center for Health Policy & Economics, University of Southern California; Published July 12, 2021. Accessed July 25, 2022. healthpolicy.usc.edu/research/reducing-racial-disparities-in-early-cancer-diagnosis-with-blood-based-tests/
- Hackshaw A, Cohen SS, Reichert H, Kansal AR, Chung KC, Ofman JJ. Estimating the population health impact of a multi-cancer early detection genomic blood test to complement existing screening in the US and UK. Br J Cancer. 2021;125(10):1432-1442. doi: 10.1038/s41416-021-01498-4
- Benson JR, Jatoi I, Toi M. Treatment of low-risk ductal carcinoma in situ: is nothing better than something? Lancet Oncol. 2016;17(10):e442-e451. doi: 10.1016/S1470-2045(16)30367-9
- Liu MC, Oxnard GR, Klein EA, Swanton C, Seiden MV; CCGA Consortium. Sensitive and specific multi-cancer detection and localization using methylation signatures in cell-free DNA. Ann Oncol. 2020;31(6):745-759. doi: 10.1016/j.annonc.2020.02.011
- Cairns E. GRAIL launches pan-cancer screen – for those who can pay out of pocket. Evaluate Vantage. Published June 4, 2021. Accessed July 25, 2022. www.evaluate.com/vantage/articles/news/snippets/grail-launches-pan-cancer-screen-those-who-can-pay-out-pocket
- GRAIL gets FDA breakthrough designation for multi-cancer test. Medical Device Network. Published May 15, 2019. Accessed June 13, 2022. www.medicaldevice-network.com/news/grail-test-fda-breakthrough-status/
- Thiel D, Chen X, Kurtzman KN, et al. Prediction of cancer and tissue of origin in individuals with suspicion of cancer using a cell-free DNA multi-cancer early detection test. Cancer Res. 2020;80(16 suppl):CT021. doi: 10.1158/1538-7445.AM2020-CT021
- AI-EMERGE: Development and Validation of a Multi-analyte, Blood-based Colorectal Cancer Screening Test. ClinicalTrials.gov. ClinicalTrials.gov identifier: NCT03688906. Updated March 2, 2022. Accessed July 5, 2022. clinicaltrials.gov/ct2/show/NCT03688906
- Liu MC. Transforming the landscape of early cancer detection using blood tests—commentary on current methodologies and future prospects. Br J Cancer. 2021;124(9):1475-1477. doi: 10.1038/s41416-020-01223-7
- PATHFINDER 2: a Multi-Cancer Early Detection Study. ClinicalTrials.gov. ClinicalTrials.gov identifier: NCT05155605. Updated May 23, 2022. Accessed July 27, 2022. clinicaltrials.gov/ct2/show/NCT05155605
- Lennon AM, Buchanan AH, Kinde I, et al. Feasibility of blood testing combined with PET-CT to screen for cancer and guide intervention. Science. 2020;369(6499):eabb9601. doi: 10.1126/science.abb9601
- Cristiano S, Leal A, Phallen J, et al. Genome-wide cell-free DNA fragmentation in patients with cancer. Nature. 2019;570(7761):385-389. doi: 10.1038/s41586-019-1272-6
- Evaluation of the ctDNA LUNAR Test in an Average Patient Screening Episode (ECLIPSE). ClinicalTrials.gov. ClinicalTrials.gov identifier: NCT04136002. Updated June 23, 2022. Accessed July 5, 2022. clinicaltrials.gov/ct2/show/NCT04136002
- Prevention of Colorectal Cancer Through Multiomics Blood Testing (PREEMPT CRC). ClinicalTrials.gov. ClinicalTrials.gov identifier: NCT04369053. Updated March 11, 2022. Accessed July 5, 2022. clinicaltrials.gov/ct2/show/NCT04369053
- Ueberroth BE, Marks LA, Borad MJ, Agrwal N. Multicancer early detection panels (MCEDs) in the primary care setting. Am J Med. 2022;135(7):e145-e149. doi: 10.1016/j.amjmed.2022.03.006
- Annual estimates of the resident population by single year of age and sex for the United States: April 1, 2020, to July 1, 2021 (NC-EST2021-AGESEX-RES). US Census Bureau. Published 2022. Accessed July 14, 2022. www2.census.gov/programs-surveys/popest/datasets/2020-2021/national/asrh/nc-est2021-agesex-res.csv
- Welch HG. Liquid biopsy: misplaced faith in early cancer detection? STAT. Published August 31, 2021. Accessed July 18, 2022. www.statnews.com/2021/08/31/liquid-biopsy-misplaced-faith-in-early-cancer-detection/
- Deverka PA, Douglas MP, Phillips KA. Multicancer screening tests: anticipating and addressing considerations for payer coverage and patient access. Health Aff (Millwood). 2022;41(3):383-389. doi: 10.1377/hlthaff.2021.01316
- S.1873. Medicare Multi-Cancer Early Detection Screening Coverage Act of 2021. Published May 27, 2021. Accessed July 14, 2022. www.congress.gov/bill/117th-congress/senate-bill/1873
- Hathaway C, Shah N, Tyson C, Cohain A, Li Y. Implications of cure fractions on costs of cancer care: an innovative application to multi-cancer early detection (MCED) economic modeling. Paper presented at: ISPOR 2022. Accessed August 3, 2022. www.ispor.org/heor-resources/presentations-database/presentation/intl2022-3459/117378
- Kolata G. Blood tests that detect cancers create risks for those who use them. The New York Times. Published June 10, 2022. Accessed July 25, 2022. www.nytimes.com/2022/06/10/health/cancer-blood-tests.html
- Tafazzoli A, Ramsey SD, Shaul A, et al. EPR22-119: cost-effectiveness of multi-cancer early detection (MCED) test in subgroups with smoking history or obesity. J Natl Compr Canc Netw. 2022;20(3.5):EPR22-119-EPR122-119.
- Tafazzoli A, Ramsey SD, Shaul A, et al. Drivers of value-based price (VBP) for a multi-cancer early detection (MCED) test. Value Health. 2021;24(12):S2. doi: 10.1016/j.jval.2021.11.317
- Ortendahl J, Lee J, Hubbell E, Clarke CA, Chung KC, Kansal AR. Projected lifetime clinical value of a multicancer early detection test. Paper presented at: ISPOR 2020; Virtual. Accessed August 3, 2022. www.ispor.org/heor-resources/presentations-database/presentation/intl2020-3182/102294
- Braunstein GD, Ofman JJ. Criteria for evaluating multi-cancer early detection tests. Rev Oncol Haematol. 2021;17(1):3-6.
- Matza LS, Howell TA, Fung E, et al. Pilot study for assessment of health state utilities associated with false-positive cancer screening results. Paper presented at: ISPOR 2022. Accessed August 3, 2022. www.ispor.org/publications/journals/value-in-health/abstract/Volume-25--Supplemental-Issue-1S/POSC356-Pilot-Study-for-Assessment-of-Health-State-Utilities-Associated-with-False-Positive-Cancer-Screening-Results
- Ajani JA, Benson AB, Daly MB, Ettinger DS, Ho MM. Multicancer detection: the need for clinical guidance. Value-Based Cancer Care. 2021;12(5). valuebasedcancer.com/issues/2021/october-2021-vol-12-no-5/2983-multicancer-detection-the-need-for-clinical-guidance
- Screening for many cancers with one test: uncertainty abounds. National Cancer Institute, Current Cancers Blog. Published April 21, 2022. Accessed June 14, 2022. www.cancer.gov/news-events/cancer-currents-blog/2022/finding-cancer-early-mced-tests
