- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Contributor: Telehealth Utilization Grew for Second Straight Month in December 2021
For the second straight month, national telehealth utilization, measured as a percentage of all medical claim lines, grew in December 2021, according to FAIR Health’s Monthly Telehealth Regional Tracker.
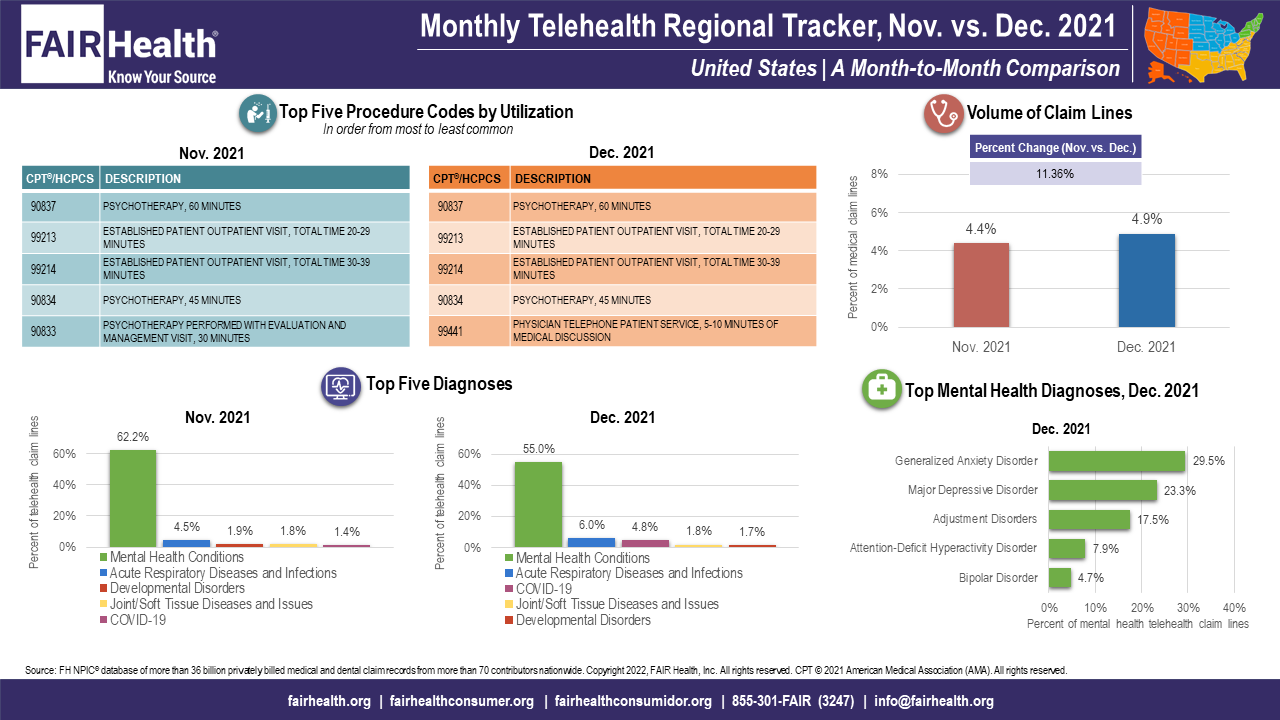
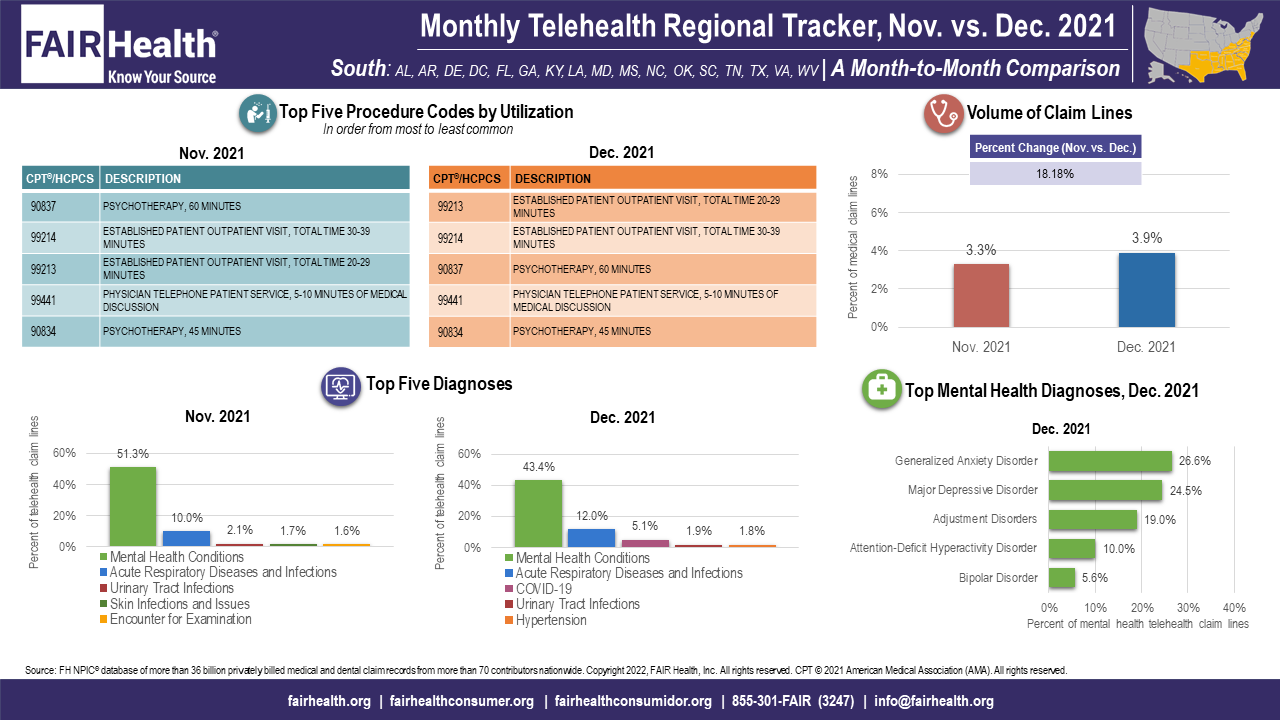
For the second straight month, national telehealth utilization, measured as a percentage of all medical claim lines, grew in December 2021, according to FAIR Health’s Monthly Telehealth Regional Tracker. Telehealth utilization increased nationally 11.4%, from 4.4% of all medical claim lines in November to 4.9% in December (FIGURE 1). Telehealth utilization also increased in December in every US census region (Midwest, Northeast, South and West), with the greatest increase (18.2%) in the South. The data represent the privately insured population, including Medicare Advantage and excluding Medicare fee-for-service and Medicaid.
FIGURE 1
Source: FAIR Health
COVID-19 and Changes in Diagnosis Rankings
The December increases in telehealth utilization coincided with the nationwide surge of COVID-19 cases fueled by the highly transmissible Omicron variant. FAIR Health data show that COVID-19, which in November had been among the top 5 telehealth diagnoses nationally and in the Midwest and Northeast, continued to hold that status in December while also joining the top 5 telehealth diagnoses in the South and West. Nationally, from November to December, COVID-19 rose from fifth place to third place among telehealth diagnoses; in the Northeast, the epicenter of December’s Omicron surge, COVID-19 rose from fifth place to second place.
In December, other diagnoses changed in their percentage share of telehealth claim lines, their rankings among telehealth diagnoses, or both. Mental health conditions remained the number one diagnosis in the nation and all regions, but everywhere fell in percentage share. In the South, mental health conditions fell to less than 50% of telehealth claim lines (43.4%), the only region where that was the case (FIGURE 2). Acute respiratory diseases and infections rose everywhere in percentage share of telehealth claim lines. Hypertension joined the top 5 telehealth diagnoses in the South and joint/soft tissue diseases and issues joined that list in the Northeast.
FIGURE 2
Source: FAIR Health
Changes in Procedure Code Rankings
In December, the procedure code for 60-minute psychotherapy, CPT® 90837, remained in first place among telehealth procedure codes nationally and in all regions but the South, where it fell from first to third place. Its percentage age share, however, fell nationally and regionally. This was part of a general trend in December toward lower utilization of psychiatric procedure codes and higher utilization of evaluation and management (E&M) codes. For example, in the Midwest, CPT 99212, an E&M code (10-19-minute established patient outpatient visit), supplanted CPT 90833, a psychiatric code (30-minute psychotherapy performed with E&M visit), in fifth place among telehealth procedure codes. In addition, in the national rankings, CPT 99441, a telehealth audio visit (5-10-minute physician telephone patient service) supplanted CPT 90833 in fifth place.
About the Monthly Telehealth Regional Tracker
Launched in May 2020 as a free service, the Monthly Telehealth Regional Tracker uses FAIR Health data to track how telehealth is evolving from month to month. An interactive map of the four US census regions allows the user to view an infographic on telehealth in a specific month in the nation as a whole or in individual regions. Each infographic shows month-to-month changes in volume of telehealth claim lines, top 5 telehealth procedure codes and top five telehealth diagnoses (or diagnostic categories), along with that month’s top five granular diagnoses within the most common diagnostic category.
As the COVID-19 pandemic and telehealth utilization continue to evolve, FAIR Health’s Monthly Telehealth Regional Tracker serves as a window into that evolution. This is one of the many ways we pursue our healthcare transparency mission.
For the Monthly Telehealth Regional Tracker, click here.
