- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Telehealth Claim Lines Rise From July 2019 to July 2020
Telehealth claims peaked in June 2020, then eased off a bit in July. There were more telehealth claims in the Northeast than in other regions.
Telehealth claim lines increased 3,806% nationally from July 2019 to July 2020, rising from 0.15% of medical claim lines in July 2019 to 6.0% in July 2020, according to new data from FAIR Health’s Monthly Telehealth Regional Tracker (FIGURE 1). The data represent the privately insured population, excluding Medicare and Medicaid.
FIGURE 1.
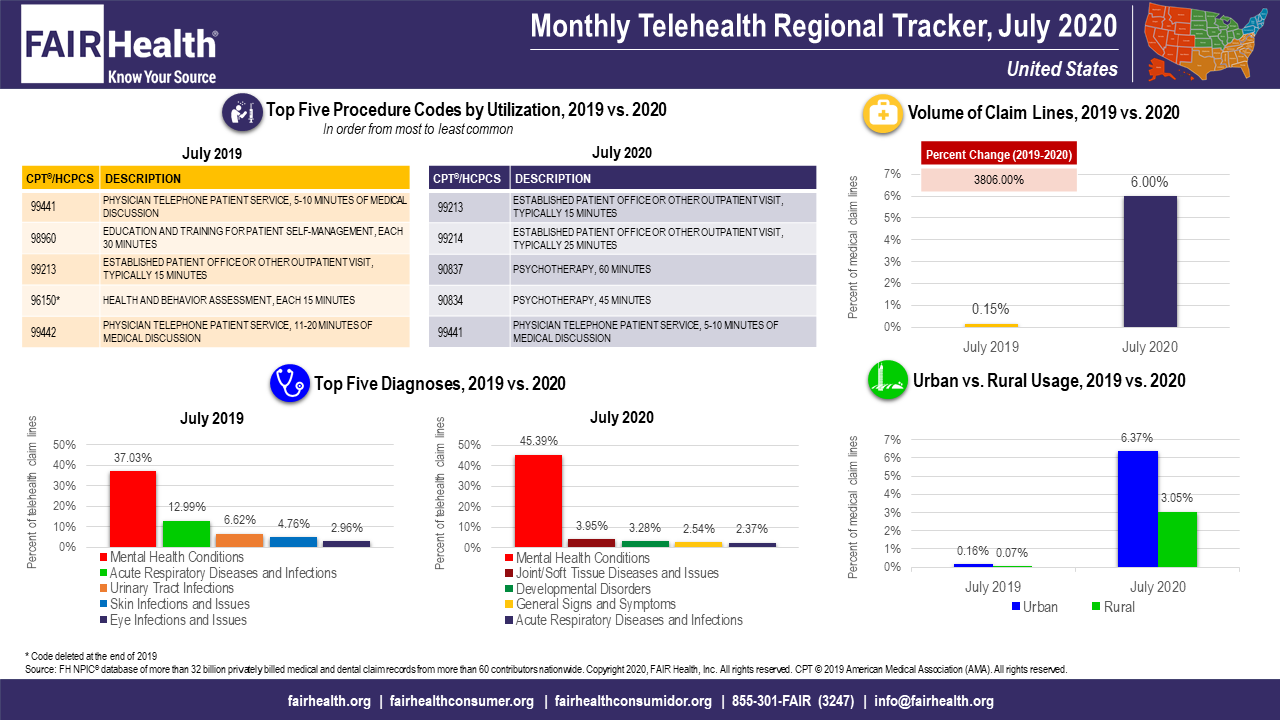
While increasing greatly from 2019 to 2020, telehealth claim lines fell 12% nationally on a month-to-month basis, from 6.85% of medical claim lines in June 2020 to 6.0% in July 2020.
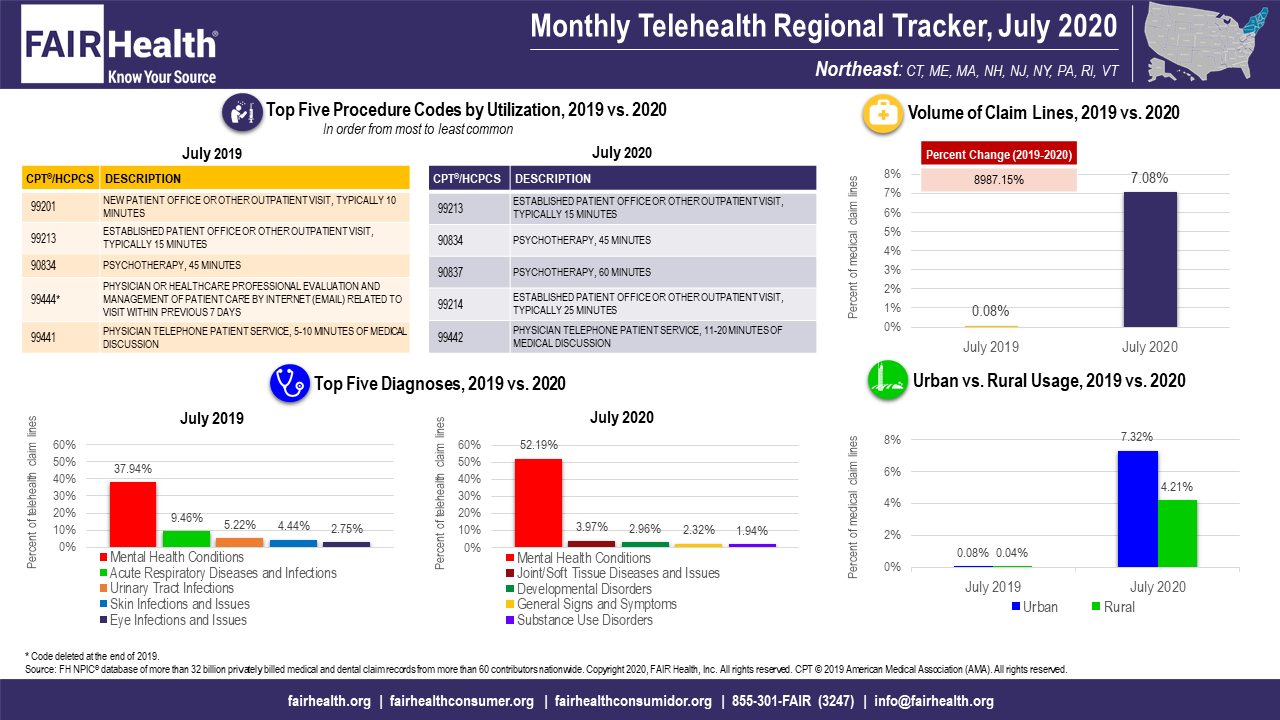
Trends in the 4 US census regions (Midwest, Northeast, South and West) were similar to those in the nation as a whole. In each region, there were large percent increases in volume of claim lines from July 2019 to July 2020, but small drops in volume of claim lines from June 2020 to July 2020. The Northeast had the greatest percent increase in volume of any region from July 2019 to July 2020: 8,987% (FIGURE 2). From June to July 2020, it also had the greatest percent decrease: 16%.
FIGURE 2.
Higher telehealth utilization from March to July 2020 in comparison with the same months in 2019 is likely a result of the COVID-19 pandemic. In March and April 2020, many states prohibited in-person rendering of elective procedures, making telehealth an attractive alternative. Many of these prohibitions expired in May as states began to open up, perhaps accounting for the decline in the telehealth share of total medical claim lines in May, June and July relative to April. However, that decline slowed from month to month, and telehealth usage remained high by comparison with 2019.
In another notable finding of the July Monthly Telehealth Regional Tracker, for the first time this year, substance use disorders emerged as one of the top five telehealth diagnoses, though only in the Northeast, where this diagnosis ranked fifth. This is consistent with an increase in substance use disorders that has been noted during the COVID-19 pandemic by CDC and others. It is also consistent with a trend toward use of telehealth to treat a wider variety of conditions.
In July, mental health conditions continued to be the number one telehealth diagnosis nationally and in every region, as they had been since March 2020. Nationally, mental health conditions represented 45% of telehealth claim lines in July 2020, compared to 37% in July 2019.
However, the percentage of telehealth claim lines accounted for by mental health conditions nationally in July 2020 stabilized, increasing monthly by one percentage point (from 44% in June to 45% in July) after larger increases in May and June. This stabilization may be the result of many people having already sought telehealth for mental health issues during the COVID-19 pandemic, leaving little room for the diagnosis to grow. It may also be due to the increasing number of other diagnoses being treated during the pandemic.
About the Monthly Telehealth Regional Tracker
Launched in May as a free service, the Monthly Telehealth Regional Tracker uses FAIR Health data to track how telehealth is evolving from month to month. An interactive map of the four US census regions allows the user to view an infographic on telehealth in a specific month in the nation as a whole or in individual regions. In addition to data on the volume of claim lines and on diagnoses, each infographic includes findings on urban versus rural usage and the Top 5 telehealth procedure codes.
The COVID-19 pandemic is continuing to have a pronounced impact on telehealth, but the details of that impact vary from month to month. FAIR Health’s Monthly Telehealth Regional Tracker provides a window into how this venue of care is evolving.
For the Monthly Telehealth Regional Tracker, click here.
Author Information
Robin Gelburd, JD, is the President of FAIR Health, a national, independent nonprofit organization with the mission of bringing transparency to healthcare costs and health insurance information. FAIR Health possesses the nation’s largest collection of private healthcare claims data, which includes over 32 billion claim records and is growing at a rate of over 2 billion claim records a year. Certified by the Centers for Medicare & Medicaid Services (CMS) as a national Qualified Entity, FAIR Health also receives data representing the experience of all individuals enrolled in traditional Medicare Parts A, B and D; FAIR Health includes among the private claims data in its database, data on Medicare Advantage enrollees. Ms. Gelburd is a nationally recognized expert on healthcare policy, data and transparency.
