- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Team-Based CINEMA Program Targets SDOH and Precision Care in Diabetes
Ian Neeland, MD, discusses the CINEMA program's impact on addressing social determinants of health (SDOH) in Ohio and the importance of precision risk tests to reduce cardiovascular metabolic disease risk.
The Center for Integrated and Novel Approaches in Vascular-Metabolic Disease (CINEMA) program is a team-based care model designed to address cardiovascular, kidney, and metabolic health risks in patients with type 2 diabetes or prediabetes. Developed by the University Hospitals Harrington Heart & Vascular Institute, the program aims to streamline care through multidisciplinary collaboration and evidence-based interventions.
Ian Neeland, MD | Image credit: University Hospitals
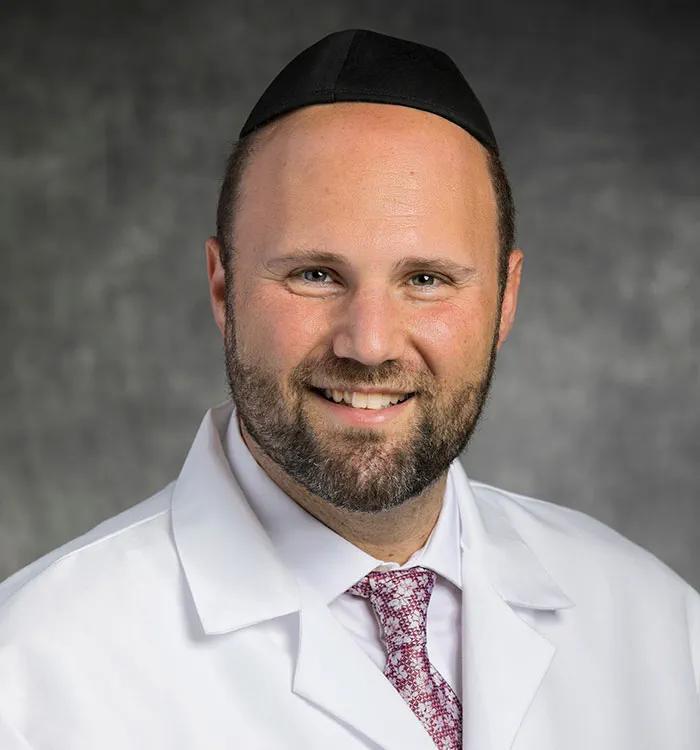
In an interview with The American Journal of Managed Care® (AJMC®), Ian Neeland, MD, provided deeper insights into the value of community health workers in the program, social determinants of health (SDOH) in Ohio, and the role of calcium scoring in clinical decision-making. Neeland serves as director of cardiovascular prevention and codirector of CINEMA at the University Hospitals Harrington Heart & Vascular Institute, as well as associate professor of medicine at Case Western Reserve University School of Medicine.
Neeland recently coauthored an article for a supplement to AJMC about the CINEMA program’s design and potential for broader application. Learn more about the management of cardiovascular-kidney-metabolic syndrome.
This transcript has been lightly edited for clarity.
AJMC: How has integrating community health workers into the CINEMA program helped address SDOH and improve patient outcomes?
Neeland: Community health workers are really a key and fundamental part of what we do, especially for folks who have several barriers to cardiovascular and metabolic care through social determinants of health, such as housing issues or other social issues like access to insurance and different therapies. Community health workers are great because they go out to where the patient lives many times and meet the patient where they are, and they’re able to navigate some of those barriers and understand where they're coming from and how that can be addressed to assist their health care and improve their outcomes.
For patients who have Medicaid, we refer every patient with Medicaid in our program to our community health worker for a screening to see if they'd be eligible for that part of CINEMA and to see if they can meet with a community health worker and establish a relationship to help them with those with those social determinants of health. We don't have data yet on how social determinants of health may directly impact health outcomes, but hopefully with more time and a greater number of patients who are availing themselves of that service, we will hopefully have some data to back up what we think shows an improvement in total access to care and engagement in care by addressing those social determinants of health.
AJMC: What are some specific SDOH in Ohio that make the CINEMA program so valuable to the area?
Neeland: A large part of Cleveland has an underserved minority area. There are barriers to housing; there are barriers to medical access—that means appointments and doctors as well as medical spends, such as pharmacy and medications. There are also food deserts, so there are a lot of areas where they're lacking fresh, healthy vegetables and fruits and things like that, where most of the food is bought from convenience stores or [are] mostly processed, packaged foods. They don't have a lot of healthy options, so that's another one.
I think also in Cleveland, socioeconomically, there are some depressed areas where there’s just not enough available in terms of resources and education for patients to, for example, do exercise at a recreation center or something like that, or to be engaged in classes. There's not as much out there. So those are areas—especially with Northeast Ohio and Cleveland, specifically—where there are several barriers to health care from a social determinants aspect, and where we can address these in the future.
AJMC: What role does precision risk assessment, such as coronary artery calcium scoring, play in tailoring care for patients in the CINEMA program, and how has it influenced clinical decisions?
Neeland: Precision risk assessment is key to understanding and intervening for patients to reduce their risk for cardiovascular metabolic disease. We use the most contemporary, up-to-date tools we can. That includes the new PREVENT calculator from the American Heart Association, which actually includes a social determinant of health—in this case, zip code—in that risk score, as well as several other components that were not present in prior risk scores that improve upon our precision to make risk assessments.
Calcium scoring is a big part of our program. We have a no-cost calcium scoring program, and we do many thousands of calcium scores every year. Calcium scoring is probably the most impactful additional ancillary test to risk scores that we have for cardiovascular risk prediction, and we utilize those as well to help refine and guide our interventions and our recommendations for patients.
We also do other tests, such as advanced lipoprotein profiles, checking lipoprotein(a), looking at family history, and looking at other risk enhancers to better refine risk. That influences our clinical decision-making on a daily basis, and I think we've demonstrated that that's important, because the highest-risk patients will then receive the most aggressive preventive therapies for both primary and secondary prevention of cardiovascular disease and hopefully improve outcomes. So, I think those have a day-to-day impact on our patients’ care.
Telehealth Intervention by Pharmacists Collaboratively Enhances Hypertension Management and Outcomes
January 7th 2026Patient interaction and enhanced support with clinical pharmacists significantly improved pass rates for a measure of controlling blood pressure compared with usual care.
Read More
