- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Taking Stock After the First 100 Days of CJR
Launched on April 1, 2016, the Comprehensive Care for Joint Replacement (CJR) model is the first mandatory bundled payment program from CMS. To ensure that they are getting the most from the initial CJR data feeds from CMS, hospitals must understand what can and cannot be measured, and take steps now to address any issues.
What the Initial Data Will—and Won’t—Reveal
Launched on April 1, 2016, the Comprehensive Care for Joint Replacement (CJR) model is the first mandatory bundled payment program from CMS. Affecting more than 750 hospitals in 67 markets, CJR creates a host of new challenges and opportunities for participants. To ensure that they are getting the most from the initial CJR data feeds from CMS, hospitals must understand what can and cannot be measured, and take steps now to address any issues.
Analyzing 2012 to 2014 Baseline Data: Factoring in Care Path and Physician Changes
Over the last few months, hospitals participating in CJR have had the opportunity to review their 2012 to 2014 baseline data. This data set provides an important comparison point, as it comprises two-thirds of participants’ initial targets and affords insight on a number of measures, including how often patients were discharged without requiring postacute institutional care, as well as infection and revision rates. However, participants should remember to take into account any changes in their care paths and joint replacement surgeons that occurred after this time period.
What to Expect from the First CJR Data Feed
Accurate Patient Identification is Critical, Yet Challenging
Hospitals are eagerly awaiting the first round of performance period data, due to be disseminated by CMS shortly after the end of the first quarter of the program. The first CJR data feed will chiefly serve to indicate how well the system is able to identify attributed patients. Participants should analyze these data to determine which patients were missed and, conversely, which patients were identified as participating in the program who should not have been included.
It is critical, yet challenging, to properly identify CJR patients and include them in discharge planning, follow-up, and the required beneficiary notification. Ideally, this process should begin prior to or at admission. Factors that can hinder accurate identification include:
- Assigning the incorrect Diagnosis Related Group (DRG) at admission—when a complication or other significant diagnosis arises during the hospital stay, the patient’s DRG assignment upon discharge may change. This is particularly impactful when a patient is admitted with DRG 470 but discharged with DRG 469, with complications and comorbidities that entail vastly different target amounts.
- Mistaking fee-for-service patients for those enrolled in Medicare Advantage, who are excluded from the CJR program.
- Patients may convert to end-stage renal disease status midway through the episode of care. The hospital may not know that these patients have been excluded from the program until reconciliation.
- Attributing Bundled Payments for Care Improvement (BPCI) episodes to CJR—if 1 or more of a facility’s operating physicians participates in BPCI for joint services, the episode is attributed to the physician instead of the hospital. Because CMS may not identify these episodes until reconciliation, the hospital must institute measures to identify these physicians itself.
Why the Initial Data Feed Won’t Measure Financial Performance
Insufficient Time for Claims Run-out
Unfortunately, because of insufficient claims run-out, the first data feed will not permit participants to accurately compare their financial performance with the target. The data feed will only include claims submitted and paid by the time the data are cut.
For example, an episode starting on April 1 will be complete by June 30; however, depending on when CMS cuts the data, claims submitted at the end of the episode may not yet be paid and therefore will not be part of the initial data feed (see figure 1). An episode that starts on May 1 and ends on July 30 will not even have been completed by the time the data are cut. Therefore, hospitals should anticipate that not all claims will be included—only the simplest of episodes will have complete data, such as when all care is provided in the first month and the patient has no other significant issues in the second and third months.
Figure 1.
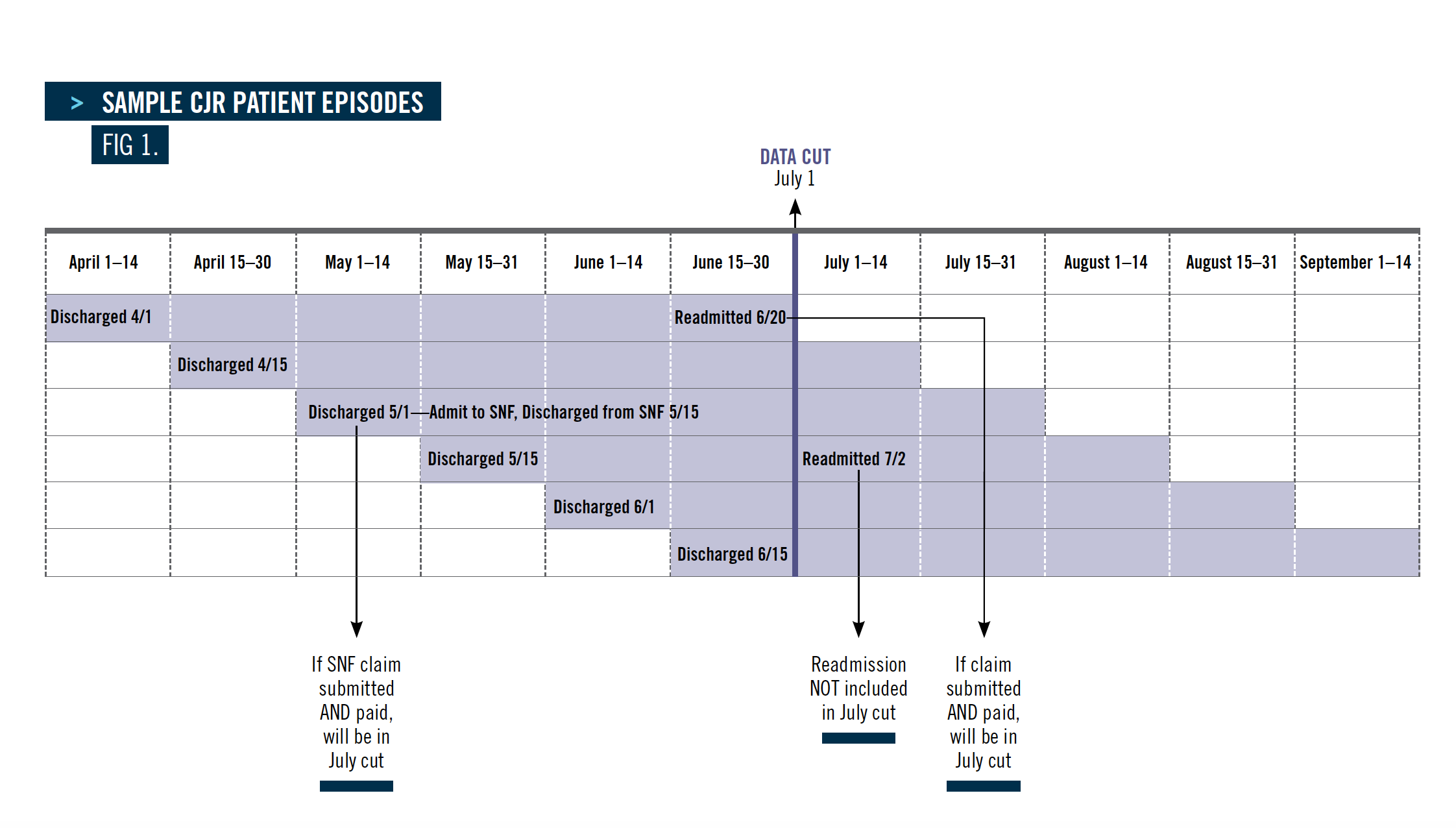
Examples of why claims may be omitted from the performance period data feed include:
- The patient is admitted to a skilled nursing facility (SNF) right before the data are cut and the claim has not yet been submitted.
- The patient is readmitted just before the data are cut, and the claim has been submitted but not yet paid.
- The 90-day episode is not complete by the time the data are cut—initially, this will include all episodes except those beginning on April 1 or 2.
What the Second 2016 Data Feed Can Reveal: Exercise Caution When Comparing Financial Performance of Complete Claims
The second performance data feed is expected in October 2016. This will include a complete refresh of all claims submitted, including those for episodes included in the first data feed. By October, all episodes that began in the April to June performance period will have ended and many will be “complete” in terms of claims included in the data feed. That is, they will have been paid and in the data feed.
However, hospitals must exercise caution when determining which episodes from the April to June performance period can be compared to the target. While participating providers should have claims for the first postdischarge setting—such as SNF, inpatient rehabilitation, and home health—they should evaluate the financial performance only for those episodes that ended at least 2 months before the data were cut. Even when the initiating hospital has submitted and received payment for the episode of care, other providers may not have submitted and/or received payment for their services.
Hospitals can also conduct the first evaluation of their readmission rates to assess how often infections are occurring, whether chronic conditions are properly managed, and how many revisions are necessary.
Remember that hospitals may be financially accountable under the program rules even if they believe a readmission is not related to the patient’s joint replacement. For example, if the patient is readmitted for congestive heart failure during the third month, that readmission will count as part of the episode of care.
The postacute network and discharge pattern is an important metric that can be examined in part from the initial performance data feed, and more fully in the second performance data feed. It is critical to know which postacute providers are receiving the hospital’s CJR patients; if the hospital has established a preferred network, the October data feed can help it determine if those providers are being used. Participants will have enough data at this point to assess the readmission rate from those postacute providers, as well as to determine whether length of stay (LOS) protocols for SNFs are being followed.
Importance of Postacute Care Coordination Under CJR: Appropriate Home Care Could Yield Significant Savings
Clearly, coordination with postacute providers is critically important in managing care and costs under CJR. Nationally, most spending following acute care for joint replacements has occurred within 5 to 10 days of discharge, and, not surprisingly, SNFs are responsible for the greatest portion of that spend. Ensuring that all appropriate patients are referred to home care rather than SNFs can yield significant savings, and coordinating protocols and the care transition with SNFs that admit the facility’s CJR patients is also essential.
If a participant does not have a SNF network in place, it should develop one now. At a minimum, it should require participating SNFs to provide key metrics, such as hospital readmission rates, percent of discharges to home health, LOS, patient satisfaction, and Medicare star rating. Most importantly, hospitals should begin preparing for discharge and postacute care as soon as the joint replacement procedure is scheduled, and consider implementing a strong “prehab” program if one is not already in place.
