- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Symptom-Triggered Testing Detects Early-Stage Ovarian Cancer in 1 in 4 Women
Symptom-triggered testing via the fast-track pathway identified early-stage high-grade serous ovarian cancer in 1 in 4 women, potentially leading to better survival outcomes.
One in 4 women diagnosed with high-grade serous ovarian cancer through symptom-triggered testing was found to have early-stage disease, according to a study published in the International Journal of Gynecological Cancer.1
Ovarian cancer is the 6th most common cause of cancer-related deaths in the United Kingdom (UK).2 Most (93%) women diagnosed with early-stage ovarian cancer (International Federation of Gynecology and Obstetrics [FIGO] stage I or II) survive after 5 years vs 13% diagnosed in advanced stages (stage III or IV). Although those diagnosed with stages I and II ovarian cancer have better survival rates, early detection is often difficult due to the vague symptoms and low incidence of ovarian cancer.3
However, past research identified a symptom triad associated with ovarian cancer, namely pain, early satiety, and increased abdominal size and/or bloating.4 This was then used to develop a symptom index incorporated into national guidelines to raise awareness among clinicians.
Consequently, ovarian cancer symptom-triggered testing was endorsed by cancer organizations in the US and UK; it is considered the fast-track pathway. In this pathway, it is recommended that symptomatic women be prioritized for testing and referred to see a gynecologist within 2 weeks.1 It also involves testing for cancer antigen (CA)-125; if the CA-125 level is raised, the patient must undergo a transvaginal ultrasound scan.
Despite being endorsed by cancer organizations, the potential value of symptom-triggered testing in detecting early-stage disease or low tumor burden among women with high-grade serous ovarian cancer remains unclear. Therefore, the researchers conducted a study to report on the FIGO stage, disease distribution, and complete cytoreduction rates of women in the fast-track pathway who were diagnosed with high-grade serous ovarian cancer.
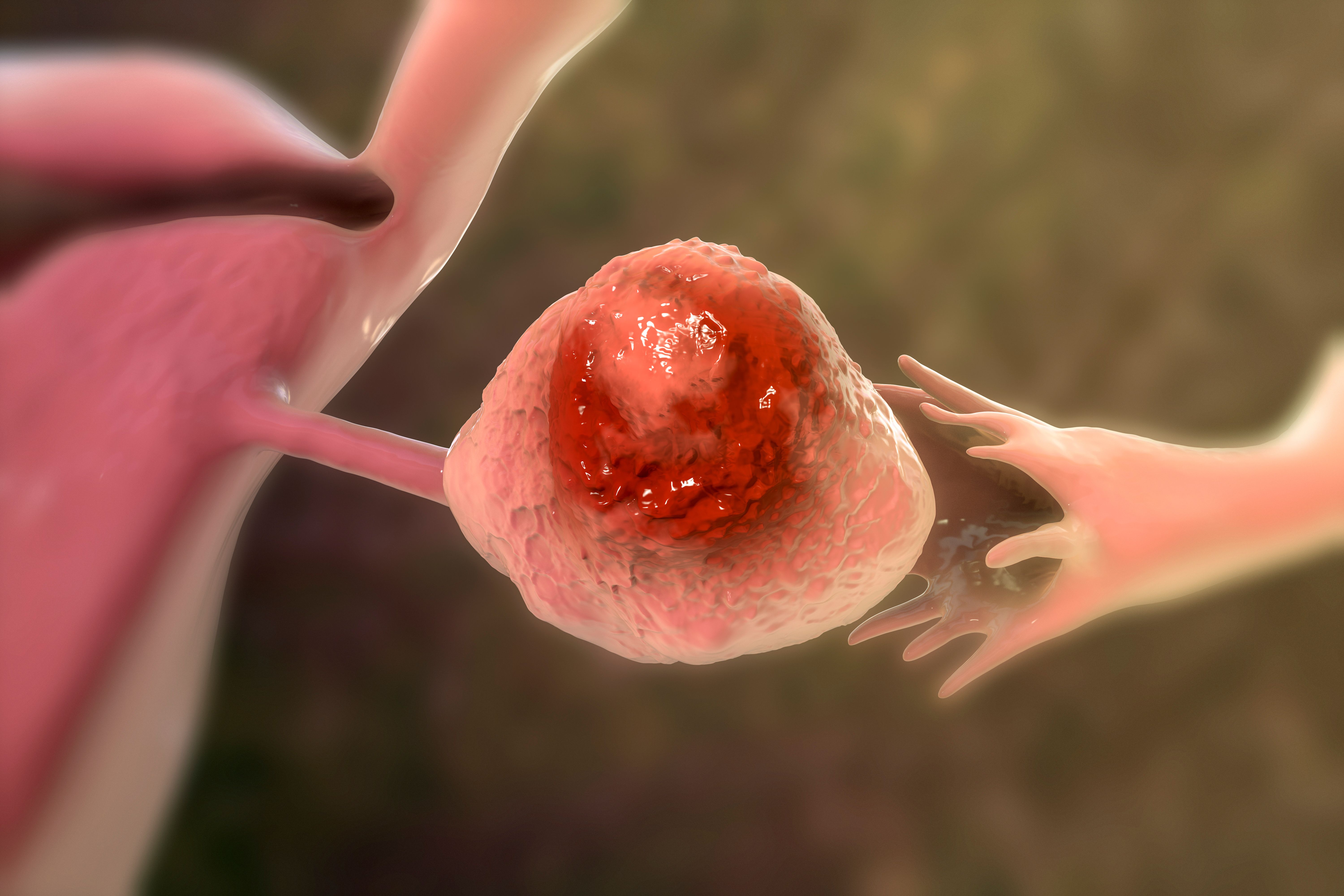
Symptom-triggered testing via the fast-track pathway identified early-stage high-grade serous ovarian cancer in 1 in 4 women. | Image Credit: Dr_Microbe - stock.adobe.com
They analyzed a dataset from Refining Ovarian Cancer Test accuracy Scores (ROCkeTS), a single-arm prospective diagnostic test accuracy study that recruited patients from 24 UK hospitals. Eligible women between the ages of 16 and 90 had a raised CA-125 level at the primary care level, any abnormal imaging results, or both.
Between June 2015 and July 2022, these women were recruited after a referral to the hospital via the fast-track pathway, routine outpatient referrals, or following emergency admissions. The researchers followed these patients until a histological diagnosis was attained through a biopsy or surgery at 3 months; those who did not undergo biopsy or surgery were followed up at 12 months. Consequently, patients could only be recruited before undergoing surgery or a biopsy.
Of the 2596 patients in ROCkeTS, 1741 (67.0%) were recruited via the fast-track pathway, 692 (26.7%) through outpatient clinics, and 163 (6.3%) following emergency presentations. The researchers found that 119 of 1741 (6.8%) women presenting via the fast-track pathway were diagnosed with high-grade serous ovarian cancer; the median age was 63 years, and 89.9% were post-menopausal.
Out of these 119 patients, 112 (94.1%) had a performance status of 0 and 1, 77 (64.7%) had low-to-moderate disease distribution, and 30 (25.2%) were diagnosed with stages I/II ovarian cancer. Also, 78 (65.5%) patients underwent primary debulking surgery, while 36 (30.3%) received neoadjuvant chemotherapy followed by interval debulking surgery; the remaining patients (4.2%; n = 5) did not undergo surgery. Lastly, 61.3% achieved complete cytoreduction (n = 73), while 15.1% (n = 18) achieved optimal cytoreduction.
“Our figures demonstrate that in a real-world setting, symptom-based testing can potentially lead to a diagnosis of high-grade serous ovarian cancer with low disease spread and results in a high proportion of complete cytoreduction,” the authors wrote.
The researchers acknowledged their limitations, including the modest number of women recruited through the emergency pathway and other outpatient referrals; this limited the ability to draw meaningful conclusions. Despite their limitations, the researchers expressed confidence in their findings.
“Symptom-triggered testing may help identify women with low disease burden, potentially contributing to high complete cytoreduction rates and improving survival outcomes in these patients,” the authors concluded.
References
- Kwong FLA, Kristunas C, Davenport C, et al. Symptom-triggered testing detects early stage and low volume resectable advanced stage ovarian cancer. Int J Gynecol Cancer. Published online August 13, 2024. doi:10.1136/ijgc-2024-005371
- Ovarian cancer statistics. Cancer Research UK. Accessed August 29, 2024. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/ovarian-cancer
- Rai N, Nevin J, Downey G, et al. Outcomes following implementation of symptom triggered diagnostic testing for ovarian cancer. Eur J Obstet Gynecol Reprod Biol. 2015;187:64-69. doi:10.1016/j.ejogrb.2015.02.011
- Ovarian cancer: recognition and initial management. NICE. April 27, 2011. Accessed August 29, 2024. https://www.nice.org.uk/guidance/cg122/
