- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Study Identifies Risk Factors for Thromboembolic Events in Patients With PNH
Researchers found indicators that increased the risk of thromboembolic events in patients with paroxysmal nocturnal hemoglobinuria (PNH).
Several factors appear to be indicators of increased risk of thromboembolic events (TEs) in patients with paroxysmal nocturnal hemoglobinuria (PNH), according to a study published in Annals of Hematology. These factors include a prior history of TEs, 30% or more glycosylphosphatidylinositol (GPI)-negative granulocytes, and lactate dehydrogenase (LDH) of at least 1.5 × upper limit of normal (ULN) plus 2 or more high disease activity (HDA) criteria.
PNH is a rare clonal hematopoietic stem cell disorder that is caused by a mutation in a specific gene, phosphatidylinositol glycan class A. TEs are the leading cause of death in patients with PNH, with 40% to 67% of deaths stemming from TEs. The proportion of GPI-negative granulocytes has been found to be associated with risk of TEs, as well as elevated LDH. This study aimed to analyze “patient data from [the International PNH Registry] to identify risk factors for TE and evaluate the odds of TE in the presence of specific disease characteristics and clinical parameters.”
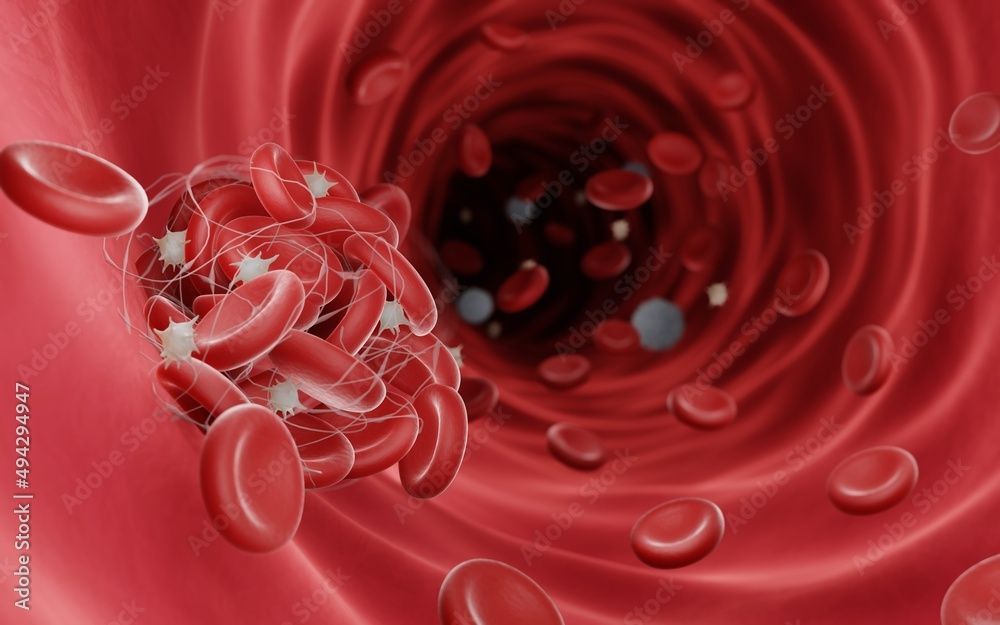
Blood clots (fibrin clots) are usually formed to stop the bleeding during injury, Blood clots can be dangerous when they obstruct blood flow and cause thrombosis | Image Credit: Artur - stock.adobe.com
Patients who were included in the International PNH Registry through July 8, 2019, were eligible for the study. Patients who were not treated with complement inhibitors and had incident TE after enrollment, a nonzero follow-up duration, and documented information had their data included for the analysis. TE cases were defined as untreated patients who had at least 1 TE after enrollment. Demographic and clinical parameters were collected at 2 points before the TE index date, including immediately preceding the date.
There were 57 patients who had TE included in this study who were matched with 189 controls. Patients were primarily European (77.6%) and male (54.5%), with a mean age of 47 years. A history of bone marrow failure was found less often in TE cases compared with the controls (68.4% vs 78.8%). Fewer TE cases had less than 10% and 10% to 30% of GPI-negative granulocytes compared with controls (<10%: 12.3% vs 22.8%; 10%-30%: 1.8% vs 8.5%). There were also more TE cases who had 50% or more GPI-negative granulocytes (29.8% vs 13.2%), an LDH ratio of at least 1.5 × ULN (38.6% vs 21.7%), HDA (33.3% vs 15.3%), and a history of TEs (21.1% vs 5.8%) compared with controls.
Patients who had an LDH ratio of at least 1.5 × ULN and 4 or more HDA criteria had an increased risk of TE (odds ratio [OR], 11.76; 95% CI, 1.80-95.79). Having an LDH ratio of at least 1.5 × ULN and 2 to 3 HDA criteria (OR, 6.23; 95% CI, 1.36-35.30), recent anticoagulation (OR, 4.79; 95% CI, 1.78-14.18), history of major adverse vascular events (OR, 2.17; 95% CI, 0.96-4.80), history of TE (OR, 3.60; 95% CI, 1.41-9.24), and HDA (OR, 3.07; 95% CI, 0.96-4.80) were also associated with an increased risk of TE. Patients with symptoms of abdominal pain (OR, 5.00; 95% CI, 1.73-15.88), hemoglobinuria (OR, 2.73; 95% CI, 1.07-6.95), and dysphagia (OR, 3.00; 95% CI, 0.54-16.67) also had increased risk of TE.
A multivariable analysis specified that patients with no history of TE but a recent anticoagulation (OR, 9.30; 95% CI, 1.20-72.27), history of TE with recent anticoagulation (OR, 8.91; 95% CI, 0.86-92.62), a history of TE without recent anticoagulation (OR, 5.33; 95% CI, 0.26-109.57), GPI-negative granulocytes between 30% and 50% (OR, 4.94; 95% CI, 0.54-45.32), 50% or more GPI-negative granulocytes (OR, 1.97; 95% CI, 0.45-8.55), LDH ratio of at least 1.5 × ULN and 2 or 3 HDA criteria (OR, 3.18; 95% CI, 0.44-23.20), and LDH ratio of at least 1.5 × ULN and 4 or more HDA criteria (OR, 3.60; 95% CI, 0.44-23.20) all had an increased risk of TE.
There were some limitations to this study. Values of potential risk factors for TE were missing for some patients due to using an observational data set; as many as 50% of the patients could be missing data. Only a subset of the patients met the inclusion criteria to be labeled as having had a case of TE. Patients at highest risk were potentially left out of the analysis due to those with prior treatment with complement inhibitors being excluded. Controls for smoking and obesity were not performed. A reason was also not identified for patients not receiving anticoagulation if they had a history of TE.
The researchers concluded that this analysis provided the likeliest risk factors associated with TE, which is the leading cause of death in patients with PNH. Further studies on patients with PNH who have TEs is needed in the future.
Reference
Hochsmann B, Peffault de Latour R, Hill A, et al. Risk factors for thromboembolic events in patients with paroxysmal nocturnal hemoglobinuria (PNH): a nested case–control study in the International PNH Registry. Ann Hematol. Published online September 5, 2023. doi:10.1007/s00277-023-05402-3
