- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Study Finds Pirtobrutinib Associated With Improved Outcomes vs Venetoclax in Relapsed CLL
Pirtobrutinib led to improved outcomes compared with venetoclax in patients with relapsed chronic lymphocytic leukemia (CLL) following covalent Bruton tyrosine kinase inhibitor therapy.
The objective response rate (ORR) among patients with relapsed or refractory chronic lymphocytic leukemia (CLL) treated with pirtobrutinib was higher and overall survival (OS) and progression-free survival (PFS) of pirtobrutinib were comparable with venetoclax monotherapy, according to a matching adjusted indirect comparisons (MAIC) study published in Haematologica.1 In the study, all patients had been previously treated with a covalent Bruton tyrosine kinase inhibitor (cBTKi) therapy.
“Pirtobrutinib was also associated with a generally better toxicity profile compared to venetoclax, suggesting it may be an effective treatment option for patients who are venetoclax-naïve after progressing on a cBTKi,” the authors wrote.
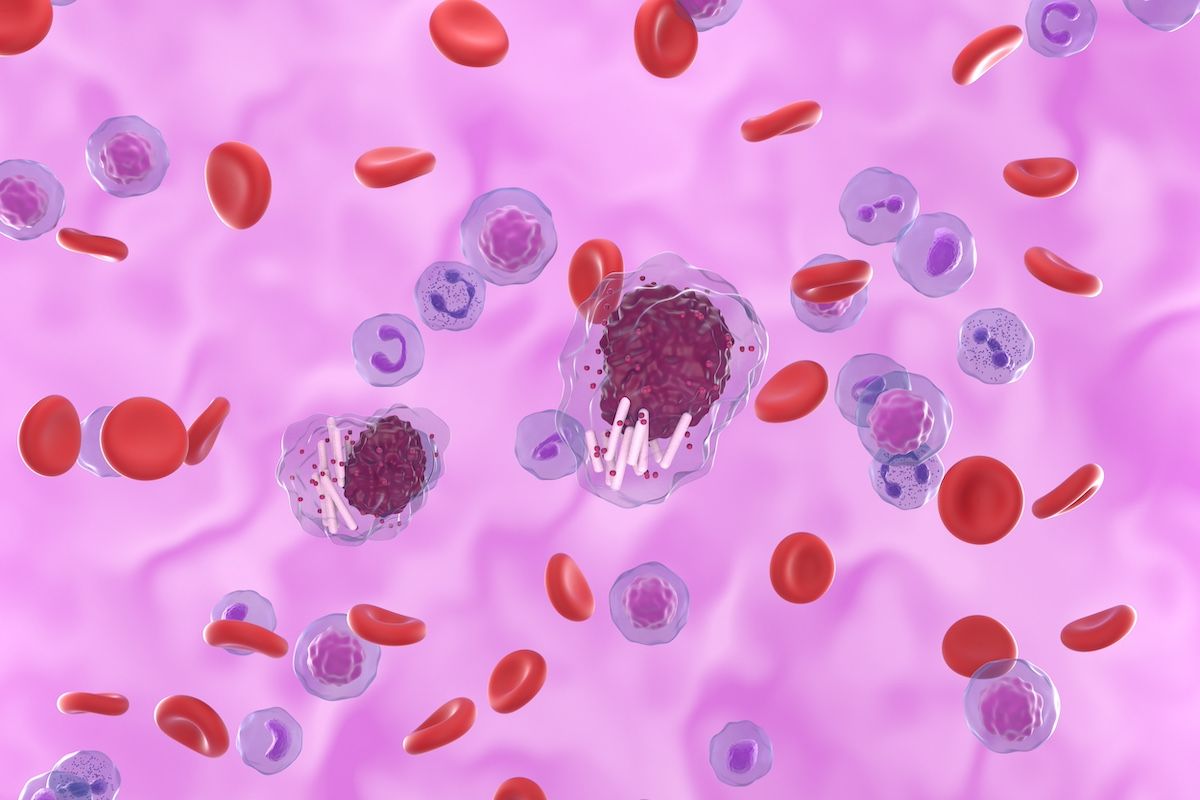
In a recent MAIC study, pirtobrutinib showed a superior ORR and similar PFS and OS compared with venetoclax in relapsed or refractory CLL. | Image credit: Laszlo - stock.adobe.com
In contrast to standard BTK inhibitors, pirtobrutinib blocks the action of the protein that signals cancer cells to multiply, without affecting other similar proteins in the body, thereby reducing the risk of side effects, according to the National Cancer Institute.2 The current study aimed to estimate the efficacy of pirtobrutinib vs venetoclax continuous monotherapy in relapsed or refractory CLL following treatment with a cBTKi.1
“While many specialists and institutions have gained experience in the safe administration of venetoclax, careful patient selection and attention to patient care remain critical with adherence to the recommended ramp-up phase of treatment to avoid the serious adverse event (AE) of tumor lysis syndrome (TLS), which often requires administration of uric acid-lowering agents, and, less commonly, the need for hospitalization for TLS monitoring,” the authors wrote, “Therefore, a need remains for additional safe and effective treatment options for patients with CLL after failure of cBTKi therapy.”
The researchers performed a comparison analysis of 146 patients receiving pirtobrutinib in the phase 1/2 BRUIN trial (NCT03740529) and 91 patients from a phase 2 open-label trial (NCT02141282) of single-agent venetoclax. Both studies enrolled patients with CLL who had relapsed or refractory disease, and patients in both cohorts were limited to those with prior cBTKi exposure and without prior venetoclax. No patient was excluded from either cohort from exhibiting pathological evidence of Richter’s transformation. Patients receiving pirtobrutinib were evaluated from March 2019 to July 2022, and the venetoclax trial enrolled 91 patients between September 2014 and November 2016.
PFS and OS among those treated with pirtobrutinib and venetoclax were comparable in both unweighted and weighted analyses. The weighted HR for PFS was 1.01 (95% CI, 0.58-1.73; P = .98) and for OS was 0.64 (95% CI, 0.25-1.67; P = .34). ORR was significantly higher for pirtobrutinib (80.2% vs. 64.8%, P = .01). Treatment-emergent AEs of grade 3 or higher were lower in weighted analyses for pirtobrutinib versus venetoclax (all P < .01), except for pneumonia, which was similar. The rates of complete response were 1.4% and 8.8%, respectively.
Anemia, neutropenia, febrile neutropenia, and thrombocytopenia were each significantly lower in patients treated with pirtobrutinib, while pneumonia and treatment discontinuations due to an AE were not different between pirtobrutinib and venetoclax.
The authors noted that inherent limitations to indirect analyses should be recognized when evaluating the study findings, such as the fact that there were no patient-level data available for venetoclax. The outcomes observed may not be replicated in a trial where cohorts were balanced at the individual patient level by means of randomization.
“Despite the limitations of using a MAIC, this study provides initial insights and improves upon naïve indirect comparisons by adjusting for known cross-trial differences to suggest improved ORR, similar PFS and OS, and the favorable toxicity profile associated with pirtobrutinib,” the authors wrote. “The selection of treatment after cBTKi failure is a clinically relevant question, since the use of BTK inhibitors is widely established in most routine health care settings and post-BTKi salvage strategies remain understudied. This study provides data to inform treatment choice in a setting where little data exist.”
References
1. Al-Sawaf O, Jen M, Hess L, et al. Pirtobrutinib versus venetoclax in covalent Bruton tyrosine kinase inhibitor-pretreated chronic lymphocytic leukemia: a matching-adjusted indirect comparison. Haematologica. 2024;109(6):1866-1873. doi.org/10.3324/haematol.2023.284150.
2. Clinical trials using pirtobrutinib. National Cancer Institute. Accessed July 10, 2024. https://www.cancer.gov/research/participate/clinical-trials/intervention/pirtobrutinib
