- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
SPHERE Registry Data Highlight Racial, Ethnic Disparities in PAH Treatment, Outcomes
Data from the SPHERE registry revealed racial and ethnic discrepancies in disease severity, comorbidities, and outcomes experienced by patients with pulmonary arterial hypertension (PAH) receiving selexipag.
Real-world data have indicated that the severity, onset, and comorbidities associated with pulmonary arterial hypertension (PAH) can vary across different patient populations. A poster presented at the CHEST Annual Meeting 2023 identified racial and ethnic disparities in disease characteristics, treatment interventions, as well as outcomes in patients with PAH using registry data.
Researchers utilized data from SelexiPag: tHe usErs dRug rEgistry (SPHERE) to gather information on eligible patients. SPHERE is a multicenter, prospective, US-based, observational registry that was created to distinguish the dosing regimens, clinical features, and patient outcomes for individuals receiving selexipag.
Pulmonary Hypertension Concept | image credit: Orawan - stock.adobe.com

Eligible patients enrolled in SPHERE were considered either newly initiated on selexipag (if treatment began at or prior to 60 days before enrollment) or previously initiated (if treatment started beyond 60 days prior). Additionally, this analysis focused on race and ethnicity, specifically focusing on White, Black, and Hispanic patients.
In total, 759 patients with PAH were identified: 549 were White (72.3%), 117 were Black (15.4%), and 45 were Hispanic (5.9%), which comprised 93.7% of the SPHERE registry. The remaining patients were Asian or other/unknown, and due to the low percentage of these individuals, they were not included in the analysis. Patients were followed for up to 18 months, and data were gathered from their routine clinical visits during this time.
Among the range of PAH subtypes, over 50% of the total group had idiopathic PAH. In the subgroups, idiopathic PAH affected 51.4% of White, 55.6% of Black, and 37.8% of Hispanic patients. Additionally, 27% of the total group was affected by connective tissue disease related to PAH, and this occurred in 26.2% of White, 32.5% of Black, and 33.0% of Hispanic patients.
The data showed discrepancies affecting patients according to race and ethnicity. For example, the lowest median age at the time of PAH diagnosis and the initiation of selexipag was in Hispanic patients. Median time at diagnosis was 43 years among Hispanic patients, compared with 57 years in White patients, and 56 years in Black patients. Median age at selexipag initiation was 51 years among Hispanic patients, compared with 62 years and 60 years in White and Black patients, respectively. Hispanic patients experienced the longest time interval between their diagnosis and selexipag initiation, whereas White patients experienced the shortest.
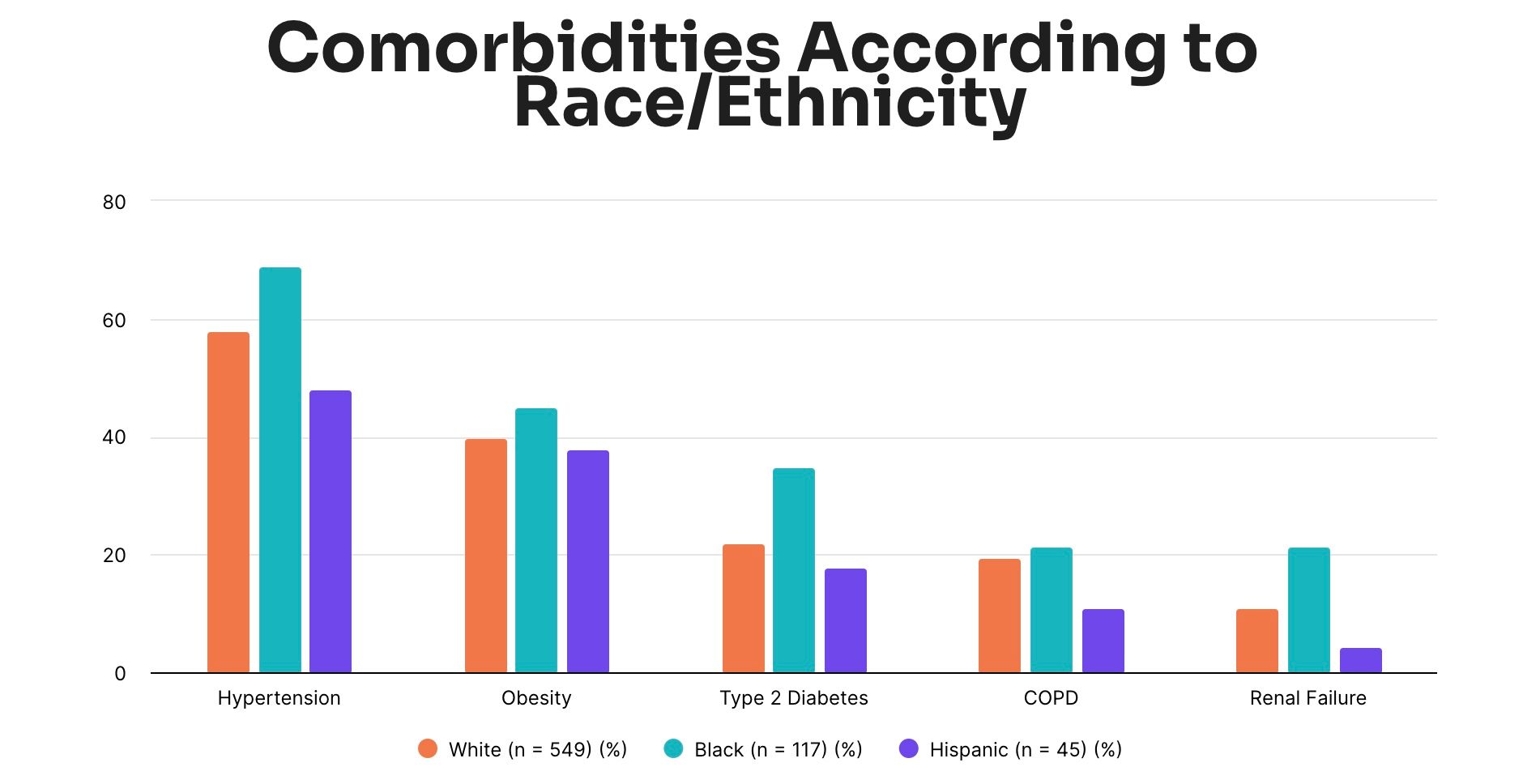
Comorbidities such as hypertension, obesity, type 2 diabetes, chronic obstructive pulmonary disease (COPD) and renal failure affected Black patients at a higher rate. Hispanic patients experienced these comorbidities at the lowest rates, respectively.
The World Health Organization (WHO) functional class (FC) status and Registry to Evaluate Early and Long-Term PAH Disease Management (REVEAL) 2.0 and REVEAL Lite 2 scoring were used to measure disease severity in this study. Results showed that, in a similar trend, Hispanic patients carried less risk and had less severe disease compared to White and Black patients. Forty percent of Hispanic patients were assessed as WHO FC III, compared with 53.4% of White patients and 50.4% of Black patients.
Overall, the researchers’ findings suggest existing disparities between racial and ethnic groups affected by PAH. SPHERE proved to be a valuable tool in their assessment as it highlighted differences in individuals with PAH according to age, duration of disease, as well as disease severity and duration prior to and at the initiation of selexipag.
The authors also noted that the registry was able to include valuable data on minority populations usually underrepresented in randomized trials on PAH. These real-world data more appropriately characterize the state of PAH and how it affects individuals across the US; however, the authors point to the lower percentages of Hispanic and Asian patients enrolled in SPHERE. This discrepancy remains important because it demonstrates that certain populations are still underrepresented and how it is crucial to understand the recruitment or enrollment obstacles these demographics face, and that more work needs to be done to create a holistic picture of PAH’s influence in the US.
Reference
Farber H, Chakinala MM, Hemnes AR, et al. Characteristics of patients with pulmonary arterial hypertension receiving selexipag in the SPHERE registry by race and ethnicity. Poster presented at: CHEST Annual Meeting 2023; October 8-11; Honolulu, HI. doi:10.1016/j.chest.2023.07.3836
