
- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Screening for Cancer: The Economic, Medical, and Psychosocial Issues
Abstract
Despite significant improvements in mortality over the past 20 years, cancer remains the second leading cause of death in the United States. One reason for the improvement in mortality is screening for several common cancers in people at average risk for breast, cervical, colorectal, and prostate cancers, and screening for lung cancer in those with a 20-plus pack-year history. Such screening may result in earlier diagnosis when the cancer is most likely to respond to treatment. However, there are no population-based screening recommendations for the majority of cancers in average-risk patients, most of which are not diagnosed until the later stages. One question is whether earlier diagnosis could not only reduce mortality rates but also reduce medical costs. Screening comes with several potential risks, including false positives and overdiagnosis, both of which can affect patients’ mental health, increase morbidity and mortality, and lead to excess spending. Additionally, certain cancers can evade traditional screening tests and lead to false-negative results, which delays cancer detection, treatment, and may affect treatment efficacy. The advent of liquid biopsy tests that could screen for dozens of cancers holds promise for identifying more cancers early. However, the cost, the potential for overdiagnosis and false positives, and a lack of evidence demonstrating clinical utility or an improvement in health outcomes call into question their potential use for widespread screening. Government and managed care organizations will need to consider the risks and benefits of these assays in determining coverage.
Am J Manag Care. 2020;26(suppl 14):S300-S306. https://doi.org/10.37765/ajmc.2020.88534
Introduction
More than 1.8 million cases of cancer are projected to be diagnosed in 2020, and 606,520 individuals are projected to die from the disease, making it the second leading cause of death in the United States.1 However, there hasbeen a significant decline in the rate of cancer deaths in the United States since 1991, primarily due to smoking-cessation efforts, earlier detection, and improved treatments.1 Between 1991 and 2017, the death rate from cancer fell 29%, resulting in 2.9 million fewer deaths. At the same time, the 5-year survival rate for all cancers combined has continued to increase, rising from 49% in 1975 to 69% in 2015 among all races and from 39% to 64% among African Americans.2
Cancer exerts a significant economic burden on the US healthcare system, with estimated medical costs in 2020 expected to reach $157.7 billion, a 27% increase from 2010 costs.3 Annual mean costs (direct payments and patient out-of-pocket costs) for those aged 18 years and older with cancer in 2014 dollars were described as $16,346 compared with $4484 for those without cancer, with private insurance and Medicare being the 2 largest payers of cancer care. Hospital expenses accounted for 27%, ambulatory care visits for 41%, and prescription drug expenses for 21%.4 The National Cancer Institute reports the national economic burden, defined as patient and payer medical costs for cancer (excluding oral drugs) in 2018 at $150.8 billion.5
Cancer has a significant impact on the financial health of patients and their families. Today, the estimated 16.1 million individuals living with cancer face annual out-of-pocket medical expenditures 61% higher than those without cancer ($1000 vs $622). About 1 in 4 report problems paying bills, and one-third worry about paying bills.6 A 2017 systematic review of 45 studies found that 12% to 16% of those with cancer were in debt due to their treatment, about half reported some level of financial distress, and between 4% and 45% were nonadherent with medication because of cost.7 Cancer also has significant indirect costs related to lost income. An analysis of 492,146 cancer deaths in persons aged 16 to 84 years in the United States in 2015 found $94.4 billion in lost earnings, with average loss of $191,900,8 which likely underestimated productivity loss.
Preventive Care and Early Cancer Detection
Five-year survival rates for cancer are significantly higher for those diagnosed in earlier stages (Table 11). The 5-year survival rate for patients diagnosed with metastatic lung cancer is 5% versus 57% for those diagnosed with localized disease, a mortality rate that can be significantly improved with low-dose computed tomography (LDCT) screening in current or former smokers.1
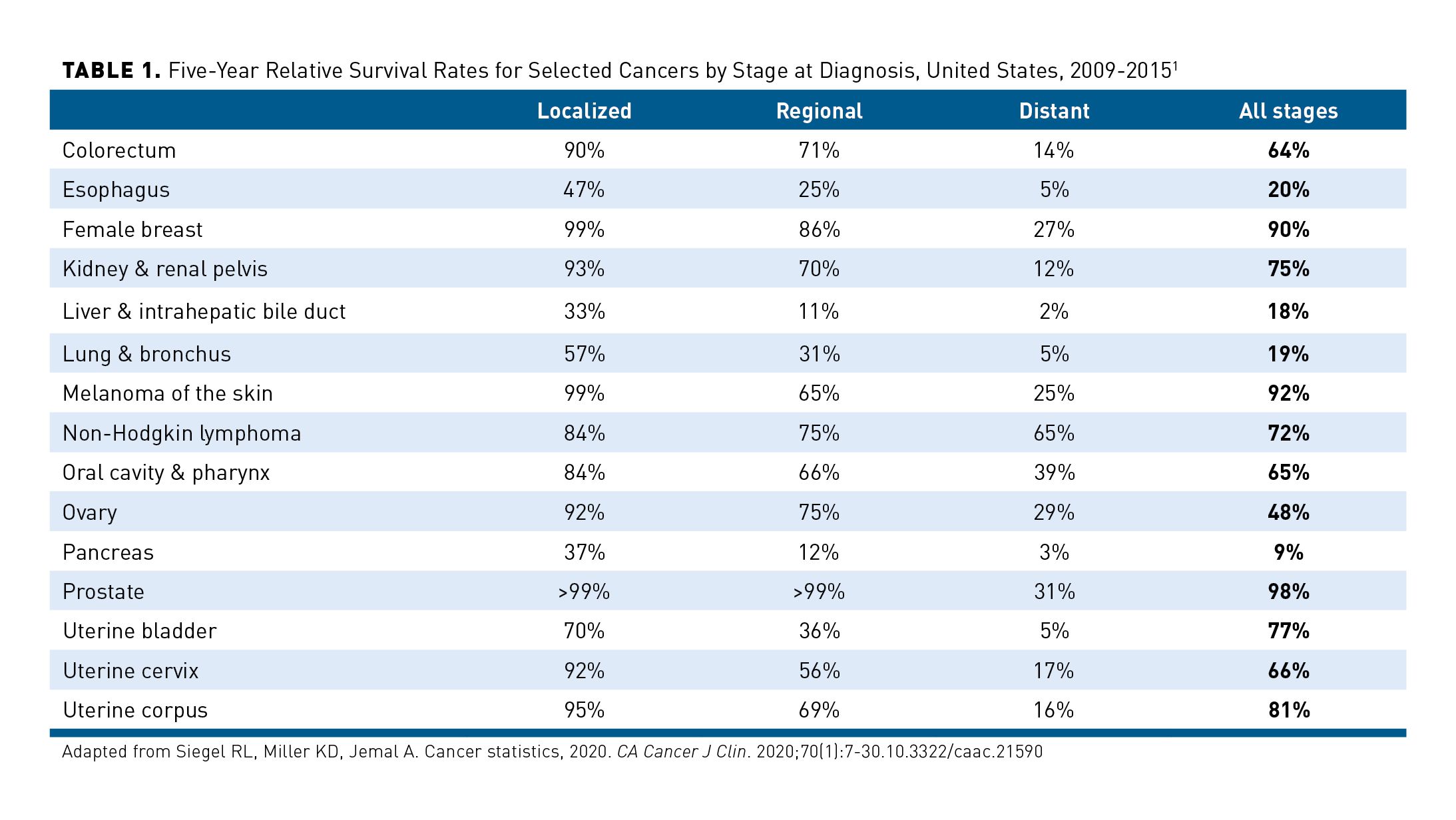
Clarke et al examined the potential reductions in cancer-related deaths if malignancies diagnosed after metastasis were, instead, diagnosed at earlier stages. Although stage IV cancers represented 18% of all diagnoses, they accounted for 48% of all cancer-related deaths within 5 years.9 The researchers found that if these patients had been diagnosed at stage III, there would have been 51 fewer cancer-related deaths per 100,000 (or 15% of all cancer-related deaths). If one-third of metastatic cancers were diagnosed at stage III, one-third at stage II, and one-third at stage I, there would be 81 fewer cancer-related deaths per 100,000 (or 24% fewer cancer-related deaths).9
Early diagnosis can reduce the cost of treatment. One study estimated the national cost-savings in the United States from early diagnosis at $26 billion per year.10 Studies in other industrialized countries find treatment costs for patients diagnosed early in the disease course to be 2 to 4 times less than those diagnosed at later stages.11 Earlier diagnosis may also reduce the financial impact on the patient and their family given shorter treatment courses, which can allow patients to continue working and therefore incur fewer expenses related to therapies.11
Barriers to Early Detection of Cancer
There are numerous barriers to the early detection of cancer, both medical and socioeconomic, including:
- Lack of symptoms. Liver, pancreatic, and ovarian cancers are typically diagnosed late in the disease course because they rarely present with symptoms early within the disease course.2
- Awareness. Individuals may not be aware of the signs and symptoms of cancer or assume they are part of some other condition.11
- Access. Lack of access to screening and diagnostic testing can delay early diagnosis and treatment.11
- Financial. Those who are uninsured or underinsured, or who have low socioeconomic status, may be less likely to obtain screening or early diagnosis.12
- Fear. This includes fear of learning about the cancer as well as fear of its treatments.12
- Human nature. Many young people feel invincible and healthy and reject the need for screening. Yet, among adults younger than 50 years, rates of cancer linked to obesity are rising. Millennials born around 1985 are now twice as likely to develop 1 of 6 obesity-linked cancers as baby boomers born around 1950 were at the same age.13
- Weak referral systems. Many people present with early-stage symptoms to their primary care provider.14,15 The clinician may not recognize the symptoms or may not have access to a robust referral network.12,15
Lack of confidence in healthcare providers. This is particularly evident in Black women given the history of the medical establishment and the African American community (eg, Tuskegee syphilis study) and discrimination and racism in the healthcare system.12
Overcoming barriers to early cancer detection requires additional training of healthcare professionals, greater public awareness of the availability of screening and the signs and symptoms of cancer, and access to affordable specialty care.11 It also requires realignment of the payment structure to provide financial incentives that prioritize screening. For instance, short-term plans without preventive service benefits or coverage that requires patients to pay out of pocket if a screening becomes diagnostic provides negative financial incentives for screening.16,17 Patients may incur high out-of-pocket costs, which can be become a deterrent to screening.
Screening for Cancer
One of the most effective ways to identify early-stage cancers is by screening asymptomatic individuals.18 Current guidelines from the American Cancer Society and the US Preventive Services Task Force (USPSTF) recommend age- and population-based screening for 4 cancers: cervical, colorectal, breast, and prostate19,20 as well as screening current and former heavy smokers for lung cancer. In addition, those with hepatitis B or C infection and cirrhosis should be screened for hepatocellular cancer.21
Several considerations go into any recommendation for wide-scale screening, with one of the most important being the ability of screening to impact the disease itself. Cochrane and Holland, who wrote a seminal paper on screening in 1971, identified 3 categories for screening: (1) those who are considered scientifically and financially acceptable, (2) those for whom there is insufficient evidence to justify their routine use at present, and (3) those for whom there is possibly some benefit, at considerable cost, for relatively few people.22
The USPSTF considers several areas before recommending disease screening in a given population23:
- Evidence related to benefits and harms from randomized clinical trials and observational studies
- Whether benefits outweigh harms and, if so, by how much and in which populations
- The degree of certainty the evidence provides for both benefits and harms
- Ages and other risk factors needed to specify when to begin and when to stop offering the service and in which populations
Trends in Cancer Screening in the United States
The Healthy People 2020 goals for cancer screening for eligible individuals in the United States based on guideline recommendations are 93% for cervical screening, 81.1% for mammograms, and 70.5% for colorectal cancer.24,25 However, despite national recommendations for such screenings, as well as the elimination of out-of-pocket costs for Medicare beneficiaries and most patients with other health insurance, screening rates in the United States remain below that goal.24,26-28 In 2015, just 50.5% of women aged 50 to 64 years reported having a recent mammogram, and 63.4% of those aged 50 to 75 years reported having a recent colorectal screening test.24 In addition, the rate of mammograms between 2000 and 2015 declined by 3%. Among men aged 50 to 75 years, 61.9% reported having a recent colorectal cancer screening test.24 In 2018, 68.8% of US adults aged 50 to 75 years were up-to-date with colorectal screening, although the rate was far lower among those with no health insurance (40.1%) or without a regular healthcare provider (36.1%).28
At the same time, however, screening may be overdone. Results of 2 recent studies found a significant number of patients who did not meet the USPSTF criteria for LDCT lung cancer screening still received the test.29,30 Results of studies also find unnecessary cervical cancer screening, including too-frequent screening, screening outside the age range, and screening after hysterectomy.31 A review of 8 studies on colorectal cancer screening also found overuse. There were numerous factors impacting inappropriate testing, which included physicians who were unaware of, had low confidence in, or perceived conflict in the guidelines.32,33 Results of other studies found overuse rates for repeat screening colonoscopy in primary care of 60.8% and between 16.1% and 36.1% for prostate cancer screening with prostate-specific antigen (PSA).34-37
Screening Risks
Although screening can certainly identify cancers at an earlier stage when the malignancy is potentially more treatable, it does not come without risks, including perforation or bleeding complications from invasive procedures (ie, colonoscopy),38 false-negative and false-positive results,39 and overdiagnosis of very early cancers or precancerous lesions that might never advance, leading to overtreatment.40
False positives are some of the greatest risks from psychosocial, medical, and economic perspectives.41-43 Whereas about 12% of women undergoing screening mammograms have an abnormal result, just 5% of those have cancer.2 Results of an observational study estimated a 61.3% probability of receiving at least 1 false-positive mammogram after 10 years if annual screening began at age 40 years (95% CI, 59.4%-63.1%) and 41.6% (CI, 40.6%-43.7%) with screening biennially, with similar findings even when screening began at age 50 years. Seven percent of women who started screening at age 40 years would receive a biopsy recommendation after 10 years of annual screening and 4.8% after 10 years of biennial screening.41
Meanwhile, an analysis of 48,499 individuals in Catalonia, Spain, who received 130,134 fecal occult blood tests (FOBT) between 2000 and 2017 estimated a 16.2% false-positive result over 7 rounds of biennial screening. Those who completed 10 rounds of screening between ages 50 and 69 years had a more than 20% risk of a false positive, resulting in an unnecessary colonoscopy for follow-up.44 A similar study conducted between 1997 and 2009 in US patients aged 50 to 79 years found a 20.5% risk of at least 1 false-positive in those undergoing at least 10 years of annual FOBT and 8.8% in those undergoing 10 years of biennial FOBT.45The FDA identified a false-positive rate with Cologuard of 13.4% compared with 5.1% with fecal immunochemical test (FIT).46
False positives may result in significant stress, anxiety, and distress.47 One study investigated the psychosocial consequences of false-positive colorectal screening and found that participants were more ambivalent about future screenings in addition to the discomfort and anxiety associated with a positive test result.42 Another study found that women with false-positive mammography results were less likely to return for future screenings.48 Study results further find higher rates of depression, mood-affecting worries, and lower mental functioning in patients who receive false positives.47 False positives also increase healthcare-associated costs, with one study analyzing the associated costs in 1087 managed care members who participated in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial, a 23-year multisite randomized trial in which participants were randomized to receive either recommended cancer screenings for 6 years or usual care.43,49 The investigators found that 43% of the study sample had at least 1 false-positive test at baseline, with men more likely to receive a false positive. The majority of patients (83%) received follow-up tests, including laparoscopy, colonoscopy, flexible sigmoidoscopy, and transvaginal ultrasound. Medical costs for those with false positives were $1024 higher for women and $1171 for men (in 2000 dollars) than for those without false positives in the year following the initial screen (P <.0001).43Ong et al estimated national expenditures for breast cancer false positives in women aged 40 to 59 years at $2.8 billion per year.50
Screening and Overdiagnosis
Overdiagnosis is defined as cancers detected on screening that would not have otherwise been detected during the patient’s lifetime and represents another potential risk of cancer screening.51 One model of 1 million men undergoing PSA screening estimated that 23% of White men and 34% of Black men would be diagnosed with such very early cancers.51 Another analysis based on national PSA screenings conducted between 1985 and 2000 predicted overdiagnosis rates between 22.9% and 42%, depending on the model used.52
Screening mammography for breast cancer also results in high rates of cancer diagnoses that would not otherwise have been found during a woman’s lifetime. Bleyer et al estimated that 22% to 31% of all invasive screen-detected breast cancers were overdiagnosed.53 A systematic review published in 2014 determined that over 10 years between 3 and 14 women, out of a 1000, would be overdiagnosed and needlessly treated.54 Such instances may also lead to excessive costs. One study estimated national expenditures for these breast cancer diagnoses in women aged 40 to 59 years at $1 billion a year.50 Screening can also increase the risk of morbidity and mortality, with models estimating 2 to 11 screening-related deaths due to radiation per 100,000 women using digital mammography.47 Studies have shown that screening for colorectal cancer via colonoscopy is occurring more frequently than guidelines recommend and, because this is a more invasive procedure, there is an increased risk of complications. Major bleeding and perforations are potential harms in individuals undergoing screening colonoscopy, with complications occurring in up to 15 of 1000 patients screened.55-57
Cost-Effectiveness of Screening
Numerous studies find that population-based screening for breast, colon, and cervical cancers are cost-effective if not cost-saving.58-61 A systematic review of 33 studies evaluating the cost-effectiveness of several types of colorectal cancer screenings between 2010 and 2016 found 10-year screening with colonoscopy had the greatest cost-effectiveness in the United States, although all methods were cost-effective compared with no screening.59 Pataky et al concluded that biennial mammography screening from ages 50 to 69 years was most cost-effective, with an incremental cost-effectiveness ratio (ICER) of $28,921 per quality-adjusted life-year (QALY), while biennial screening from age 40 to 69 years demonstrated an ICER of $86,029/QALY. Researchers also found that screening women aged 70 to 74 years was less cost-effective than screening women aged 40 to 49 years, given the lower life expectancy and potential harms.62,63 There is less evidence for the cost-effectiveness of prostate cancer screening.64 Results of one study found it would be cost-effective if offered every 4 years and only if those with low-grade cancers identified on screening were followed with active surveillance.65
Liquid Biopsy for Cancer Screening
Liquid biopsies that analyze circulating tumor DNA and tumor cells in plasma are already used to identify genetic variants of tumors and guide real-time systemic therapy. They are less invasive than tissue biopsies and can provide greater information about the genetic variation of the tumor compared with a tissue biopsy.66 They may also be cost-effective, particularly if used to inform decisions regarding treatment.67 However, screening tests should not only be accurate and reliable, with high levels of sensitivity (ie, low rate of false negatives), specificity (ie, low rate of false positives), and robustness, but also should demonstrate clinical utility (ie, that screening improves outcomes compared with no screening).66 This, in turn, requires large-scale clinical trials with longitudinal follow-up, even in participants with no signs of cancer. It should also provide clear evidence of the origin of the tumor in order to minimize further testing, identify clinically insignificant early-stage tumors to reduce overdiagnosis and overtreatment, and distinguish between indolent versus lethal disease. Aravanis et al suggested that appropriately powering such a trial would require hundreds of thousands of participants.68
Results of a 2018 review of liquid biopsies found no evidence of clinical validity to suggest clinical use for screening outside of a clinical trial. The authors also noted that it is possible that the assays may detect very early circulating genomic variants that were never destined to become cancers (ie, “biologic false positives”), with the same overdiagnosis discussed above with traditional cancer screening approaches.66 Regardless, once these tests are approved and on the market, payers, regulatory agencies, and medical societies will have to develop guidelines regarding the frequency and coverage of such screening.18
Estimates are that the broad, multigene panels under investigation would cost between $5000 and $10,000 each. There are currently no published cost-effectiveness studies, and there are differences in insurance coverage.69 Currently, Medicare does not cover screenings in the absence of signs or symptoms of disease, with the exception of screenings for colorectal, breast, cervical, prostate, and lung cancers.27 Individuals undergoing a screening test for 50 cancers will not have signs and symptoms for all. Medicare also does not cover the cost of further testing and treatment if the initial test was performed in the absence of signs and symptoms.70
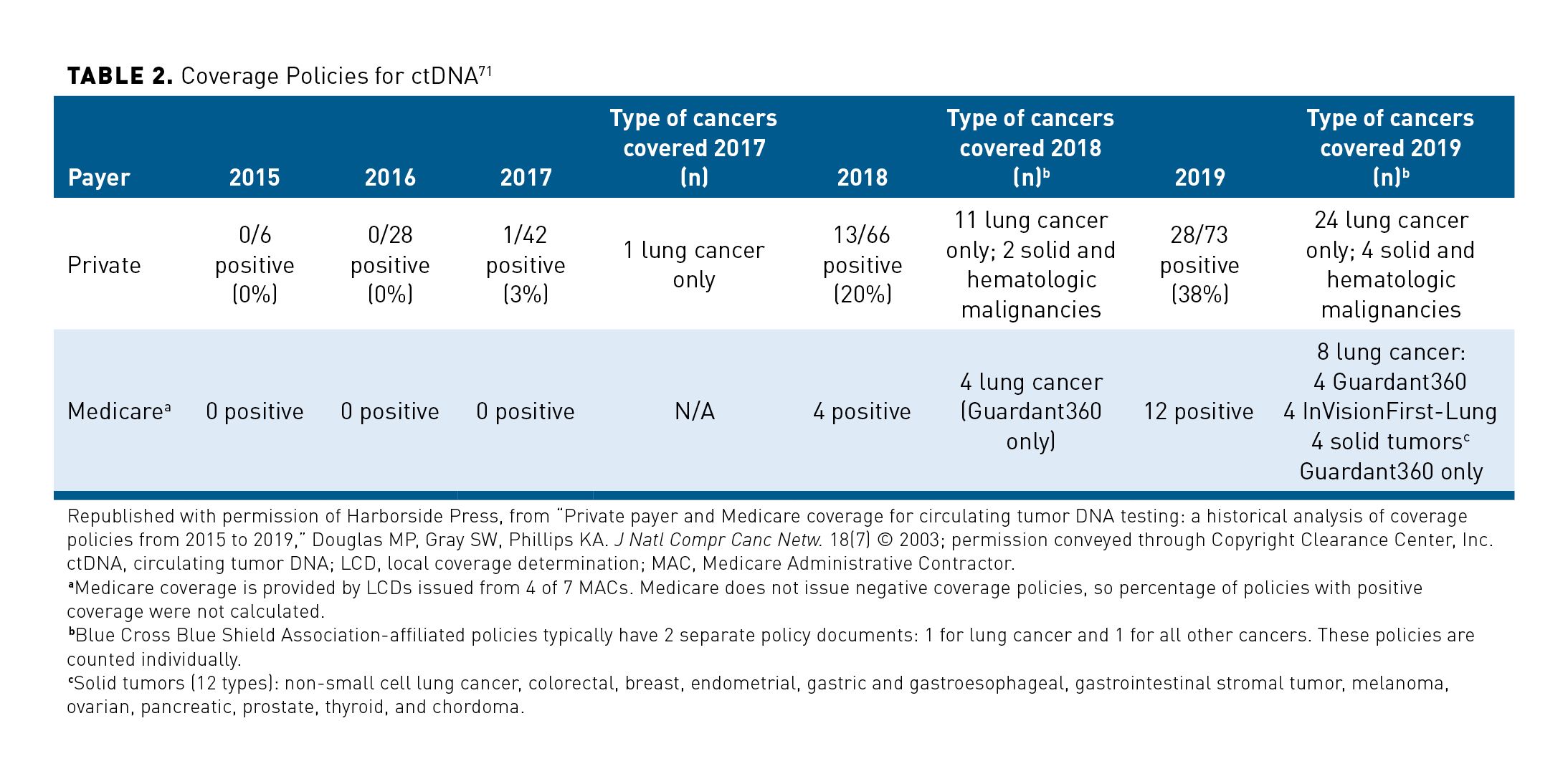
Coverage of genomic tests may provide a clue as to coverage decisions of liquid biopsies for cancer detection. Douglas et al analyzed Medicare and commercial payer coverage of circulating tumor DNA (ctDNA)-testing panels in patients already diagnosed with cancer between 2015 and 2019. By mid-2019, 65 private payers and 4 Medicare advisory committees had published policies about liquid biopsy coverage. Although no private payers covered the tests in 2016, by mid-2019, 38% covered them. On the Medicare side, there were 8 final local coverage determinations (LCDs), 2 draft LCDs, and 2 LCDs expected to become final in early 2020. Table 2 breaks down the coverage.71 Two LCDs by CMS evaluated the use of liquid biopsies to guide treatment in solid tumors and prevent organ rejection in kidney transplants.72,73 Wide divergence has been found in the coverage policies themselves. Private payers often based coverage on the cancer stage, limited coverage to certain tests, and varied on whether they covered monitoring for cancer progression. Medicare policies covered the use of liquid biopsies only for stage IIIB or IV non−small cell lung cancer (NSCLC), although private insurers covered its use for all stages. They also covered monitoring only if patients had not been previously tested or were not responding to epidermal growth factor receptor tyrosine kinase inhibitors (for NSCLC) or if there was a new primary cancer or different primacy.71 In a national coverage analysis example, CMS defined specific criteria needed to achieve to obtain coverage for blood-based biomarker tests for colorectal cancer screening to be administered once every 3 years or at the time interval designated by the FDA label for average risk, asymptomatic people aged 50 to 85 years. CMS indicated that blood-based screening tests must meet the following criteria for coverage: FDA market authorization with an indication for colorectal cancer screening, proven test performance characteristics for a blood-based screening test with both sensitivity greater than or equal to 74% and specificity greater than or equal to 90% in the detection of colorectal cancer compared with the recognized standard (colonoscopy at this time), based on pivotal studies included in the FDA labeling, and inclusion as recommended routine colorectal screening in at least one professional society guideline or consensus statement or USPSTF recommendation.74
Conclusions
Despite significant improvements in detection and treatment over the past 2 decades that have dramatically improved the 5-year mortality of many cancers, it remains the second most common cause of death in the United States. Cancer diagnosis also exerts a significant economic burden on the US healthcare system, with estimated medical costs in excess of $157 billion. Population-based screening may be responsible for mortality reductions in several cancers, particularly breast, cervical, and colorectal cancers. However, population-based screening comes with several risks, including the risk for false-positive and false-negative results as well as under- and overdiagnosis.
The advent of liquid-based biopsies that can screen for multiple cancers could revolutionize cancer screening and lead to early detection of numerous tumors, such as pancreatic and ovarian, which are typically diagnosed late in the disease course. However, their use in clinical practice does raise several questions for government, managed care organizations, payers, and medical organizations that develop screening recommendations. A useful test provides information necessary to make a clinical treatment decision that improves the net health outcome, that is, the balance of benefits and harms is better when the test is used to manage the condition than when another test or no test is used to manage the condition. The test must be technically reliable, clinically valid, and clinically useful for that purpose. Consideration must be given to whether earlier detection can lead to a change in management and an improvement in health outcomes. Cost-effectiveness, sensitivity and specificity, and clinical utility are key issues that must be considered when determining coverage and screening recommendations, as well as the impact on the healthcare system if thousands more cancers are diagnosed.
Author affiliation: Joel V. Brill, MD, FACP, is Chief Medical Officer, Predictive Health, Paradise Valley, AZ.
Funding source: This activity is supported by an educational grant from GRAIL, Inc.
Author disclosure: Dr Brill has the following relevant financial relationships with commercial interests to disclose:
Consultancies: Accomplish Health, Ambu, AnX Robotica, CapsoVision, Cernostics, Check Cap, Digma Medical, Diversatek, Dune Medical, Echosens, Endogastric Solutions, Erbe, evoEndo, Exact Sciences, Exalenz, Gala Therapeutics, Glaukos, Hello Heart, HyGIeaCare, Innovative Health Solutions, Insightec, Johnson & Johnson, Lumendi, Mainstay Medical, MaunaKea Technologies, Medtronic, Modify Health, MotusGI, Neuspera, Nuviera, Pacira, Penumbra, Perspectum, Proteus Digital Health, Reflexion, Respira Labs, Restech, Senseonics, SonarMD, StageZero Life Sciences, Sword Health, Tabula Rosa Health Care, Tusker Medical, UBC Pharma, Vertos Medical, WL Gore, Wright Medical
Authorship information: Substantial contributions to the concept and design; drafting of the manuscript; overall supervision; and critical revision of the manuscript for important intellectual content.
Address correspondence to: joel.brill@predictivehealth.com
Medical writing and editorial support: Debra Gordon, MS
REFERENCES
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7-30. doi: 10.3322/caac.21590
2. American Cancer Society. Cancer Facts & Figures, 2020. Accessed October 21, 2020. cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2020/cancer-facts-and-figures-2020.pdf
3. Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103(2):117-128. doi: 10.1093/jnci/djq495
4. Park J, Look KA. Health care expenditure burden of cancer care in the United States. Inquiry. 2019;56:46958019880696. doi: 10.1177/0046958019880696
5. National Cancer Institute. Financial burden of cancer care. March 2020. Accessed October 14, 2020. progressreport.cancer.gov/after/economic_burden
6. Ekwueme DU, Zhao J, Rim SH, et al. Annual out-of-pocket expenditures and financial hardship among cancer survivors aged 18-64 years − United States, 2011-2016. MMWR Morb Mortal Wkly Rep. 2019;68(22):494-499. doi: 10.15585/mmwr.mm6822a2
7. Altice CK, Banegas MP, Tucker-Seeley RD, Yabroff KR. Financial hardships experienced by cancer survivors: a systematic review. J Natl Cancer Inst. 2016;109(2):djw205. doi: 10.1093/jnci/djw205.
8. Islami F, Miller KD, Siegel RL, et al. National and state estimates of lost earnings from cancer deaths in the United States. JAMA Oncol. 2019;5(9):e191460-e191460. doi: 10.1001/jamaoncol.2019.1460
9. Clarke CA, Hubbell E, Kurian AW, Colditz GA, Hartman AR, Gomez SL. Projected reductions in absolute cancer–related deaths from diagnosing cancers before metastasis, 2006–2015. Cancer Epidemiol Biomarkers Prev. 2020;29(5):895-902. doi: 10.1158/1055-9965.EPI-19-1366
10. Kakushadze Z, Raghubanshi R, Yu W. Estimating cost savings from early cancer diagnosis. Data. 2017;2(30):2-16.
11. World Health Organization. Guide to cancer early diagnosis. 2017. Accessed August 8, 2020. who.int/entity/cancer/publications/cancer_early_diagnosis/en/index.html
12. Jones CE, Maben J, Jack RH, et al. A systematic review of barriers to early presentation and diagnosis with breast cancer among black women. BMJ Open. 2014;4(2):e004076. doi: 10.1136/bmjopen-2013-004076
13. Sung H, Siegel RL, Rosenberg PS, Jemal A. Emerging cancer trends among young adults in the USA: analysis of a population-based cancer registry. Lancet Public Health. 2019;4(3):e137-e147. doi: 10.1016/S2468-2667(18)30267-6
14. Yabroff KR, Gansler T, Wender RC, Cullen KJ, Brawley OW. Minimizing the burden of cancer in the United States: goals for a high-performing health care system. CA Cancer J Clin. 2019;69(3):166-183. doi: 10.3322/caac.21556
15. Neal RD, Din NU, Hamilton W, et al. Comparison of cancer diagnostic intervals before and after implementation of NICE guidelines: analysis of data from the UK General Practice Research Database. Br J Cancer. 2014;110(3):584-592. doi: 10.1038/bjc.2013.791
16. Norris L. ‘So long’ to limits on short-term plans. Healthinsurance.org.July 16, 2020. Accessed October 14, 2020. www.healthinsurance.org/so-long-to-limits-on-short-term-plans/
17. AGA: It’s time to close the Medicare colonoscopy loophole, reform Stark law. Healio Gastroenterology.April 4, 2018. Accessed October 14, 2020. healio.com/news/gastroenterology/20180404/aga-its-time-to-close-the-medicare-colonoscopy-loophole-reform-stark-law
18. Ahlquist DA. Universal cancer screening: revolutionary, rational, and realizable. NPJ Precis Oncol. 2018;2:23. doi: 10.1038/s41698-018-0066-x
19. American Cancer Society. American Cancer Society Guidelines for the Early Detection of Cancer. Revised July 30, 2020. Accessed August 10, 2020. cancer.org/healthy/find-cancer-early/cancer-screening-guidelines/american-cancer-society-guidelines-for-the-early-detection-of-cancer.html
20. US Preventive Services Task Force. A and B recommendations. 2020. Accessed August 10, 2020. uspreventiveservicestaskforce.org/uspstf/recommendation-topics/uspstf-and-b-recommendations
21. Marrero JA, Kulik LM, Sirlin CB, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases. Clin Liver Dis (Hoboken). 2019;13(1):1-1. doi: 10.1002/cld.802
22. Cochrane AL, Holland WW. Validation of screening procedures. Br Med Bull. 1971;27(1):3-8. doi: 10.1093/oxfordjournals.bmb.a070810
23. US Preventive Services Task Force. Use of decision models in the development of evidence-based clinical preventive services recommendations. May 2019. Accessed August 9, 2020. uspreventiveservicestaskforce.org/uspstf/use-decision-models-development-evidence-based-clinical-preventive-services-recommendations
24. Hall IJ, Tangka FKL, Sabatino SA, Thompson TD, Graubard BI, Breen N. Patterns and trends in cancer screening in the United States. Prev Chronic Dis. 2018;15:E97. doi: 10.5888/pcd15.170465
25. Healthy People 2020. Clinical Preventive Services. Updated October 8, 2020. Accessed October 21, 2020. healthypeople.gov/2020/leading-health-indicators/2020-lhi-topics/Clinical-Preventive-Services/data
26. Zhao J, Mao Z, Fedewa SA, et al. The Affordable Care Act and access to care across the cancer control continuum: a review at 10 years. CA Cancer J Clin. 2020;70(3):165-181. doi: 10.3322/caac.21604
27. Centers for Medicare & Medicaid Services. Preventive and screening services. 2019. Accessed July 27, 2020. medicare.gov/coverage/preventive-screening-services
28. Joseph DA, King JB, Dowling NF, Thomas CC, Richardson LC. Vital signs: colorectal cancer screening test use − United States, 2018. MMWR Morb Mortal Wkly Rep. 2020;69(10):253-259. doi: 10.15585/mmwr.mm6910a1
29. Richards TB, Doria-Rose VP, Soman A, et al. Lung cancer screening inconsistent with US Preventive Services Task Force recommendations. Am J Prev Med. 2019;56(1):66-73. doi: 10.1016/j.amepre.2018.07.030
30. Huo J, Shen C, Volk RJ, Shih YT. Use of CT and chest radiography for lung cancer screening before and after publication of screening guidelines: intended and unintended uptake. JAMA Intern Med. 2017;177(3):439-441. doi: 10.1001/jamainternmed.2016.9016
31. Alber JM, Brewer NT, Melvin C, et al. Reducing overuse of cervical cancer screening: a systematic review. Prev Med. 2018;116:51-59. doi: 10.1016/j.ypmed.2018.08.027
32. Predmore Z, Pannikottu J, Sharma R, Tung M, Nothelle S, Segal J. Factors associated with the overuse of colorectal cancer screening: a systematic review. Am J Med Qual. 2018;33(5):472-480. doi: 10.1177/1062860618764302
33. Goodwin JS, Singh A, Reddy N, Riall TS, Kuo YF. Overuse of screening colonoscopy in the Medicare population. Arch Intern Med. 2011;171(15):1335-1343. doi: 10.1001/archinternmed.2011.212
34. Krist AH, Jones RM, Woolf SH, et al. Timing of repeat colonoscopy: disparity between guidelines and endoscopists’ recommendation. Am J Prev Med. 2007;33(6):471-478. doi: 10.1016/j.amepre.2007.07.039
35. Korenstein D, Falk R, Howell EA, Bishop T, Keyhani S. Overuse of health care services in the United States: an understudied problem. Arch Intern Med. 2012;172(2):171-178. doi: 10.1001/archinternmed.2011.772
36. Welch HG, Albertsen PC. Reconsidering prostate cancer mortality − the future of PSA screening. N Engl J Med. 2020;382(16):1557-1563. doi: 10.1056/NEJMms1914228
37. Shoag JE, Nyame YA, Gulati R, Etzioni R, Hu JC. Reconsidering the trade-offs of prostate cancer screening. N Engl J Med. 2020;382(25):2465-2468. doi: 10.1056/NEJMsb2000250
38. Kim SY, Kim HS, Park HJ. Adverse events related to colonoscopy: global trends and future challenges. World J Gastroenterol. 2019;25(2):190-204. doi: 10.3748/wjg.v25.i2.190
39. American Cancer Society. Mammograms. Revised October 3, 2019. Accessed September 8, 2020. cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/mammograms/limitations-of-mammograms.html
40. National Cancer Institute. Cancer screening. Updated April 9, 2018. Accessed August 8, 2020. cancer.gov/about-cancer/screening
41. Hubbard RA, Kerlikowske K, Flowers CI, Yankaskas BC, Zhu W, Miglioretti DL. Cumulative probability of false-positive recall or biopsy recommendation after 10 years of screening mammography: a cohort study. Ann Intern Med. 2011;155(8):481-492. doi: 10.7326/0003-4819-155-8-201110180-00004
42. Toft EL, Kaae SE, Malmqvist J, Brodersen J. Psychosocial consequences of receiving false-positive colorectal cancer screening results: a qualitative study. Scand J Prim Health Care. 2019;37(2):145-154. doi: 10.1080/02813432.2019.1608040
43. Lafata JE, Simpkins J, Lamerato L, Poisson L, Divine G, Johnson CC. The economic impact of false-positive cancer screens. Cancer Epidemiol Biomarkers Prev. 2004;13(12):2126-2132.
44. Ibáñez-Sanz G, Garcia M, Milà N, et al; Adverse Effects on Colorectal Cancer Screening in Catalonia (EACC) Study Working Group. False-positive results in a population-based colorectal screening program: cumulative risk from 2000 to 2017 with biennial screening. Cancer Epidemiol Biomarkers Prev. 2019;28(11):1909-1916.
45. Hubbard RA, Ripping TM, Chubak J, Broeders MJ, Miglioretti DL. Statistical methods for estimating the cumulative risk of screening mammography outcomes. Cancer Epidemiol Biomarkers Prev. 2016;25(3):513-520. doi: 10.1158/1055-9965.EPI-15-0824
46. US Food and Drug Administration. Summary of safety and effectiveness data: Cologuard. August 11, 2014. Accessed October 21, 2020. www.accessdata.fda.gov/cdrh_docs/pdf13/P130017B.pdf
47. Nelson HD, Pappas M, Cantor A, Griffin J, Daeges M, Humphrey L. Harms of breast cancer screening: systematic review to update the 2009 US Preventive Services Task Force recommendation. Ann Intern Med. 2016;164(4):256-267. doi: 10.7326/M15-0970
48. Brett J, Austoker J. Women who are recalled for further investigation for breast screening: psychological consequences 3 years after recall and factors affecting re-attendance. J Public Health Med. 2001;23(4):292-300. doi: 10.1093/pubmed/23.4.292
49. National Cancer Institute. Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial (PLCO). Accessed August 10, 2020. prevention.cancer.gov/major-programs/prostate-lung-colorectal-and-ovarian-cancer-screening-trial
50. Ong M-S, Mandl KD. National expenditure for false-positive mammograms and breast cancer overdiagnoses estimated at $4 billion a year. Health Affairs. 2015;34(4):576-583. doi: 10.1377/hlthaff.2014.1087
51. Petitti DB, Lin JS, Burda BU. Agency for Healthcare Research and Quality. Overdiagnosis in Prostate Cancer Screening Decision Models: A Contextual Review for the US Preventive Services Task Force. AHRQ Publication No. 17-05229-EF-3. May 2018.
52. Draisma G, Etzioni R, Tsodikov A, et al. Lead time and overdiagnosis in prostate-specific antigen screening: importance of methods and context. J Natl Cancer Inst. 2009;101(6):374-383. doi: 10.1093/jnci/djp001
53. Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med. 2012;367(21):1998-2005. doi: 10.1056/NEJMoa1206809.
54. Welch HG, Passow HJ. Quantifying the benefits and harms of screening mammography. JAMA Intern Med. 2014;174(3):448-454. doi: 10.1001/jamainternmed.2013.13635
55. Vermeer NC, Snijders HS, Holman FA, et al. Colorectal cancer screening: systematic review of screen-related morbidity and mortality. Cancer Treat Rev. 2017;54:87-98. doi: 10.1016/j.ctrv.2017.02.002
56. Lieberman D, Ladabaum U, Cruz-Correa M, et al. Screening for colorectal cancer and evolving issues for physicians and patients: a review. JAMA. 2016;316(20):2135-2145. doi: 10.1001/jama.2016.17418
57. Ransohoff DF. How much does colonoscopy reduce colon cancer mortality? Ann Intern Med. 2009;150(1):50-52. doi: 10.7326/0003-4819-150-1-200901060-00308
58. Ahern CH, Shen Y. Cost-effectiveness analysis of mammography and clinical breast examination strategies: a comparison with current guidelines. Cancer Epidemiol Biomarkers Prev. 2009;18(3):718-725. doi: 10.1158/1055-9965.EPI-08-0918
59. Ran T, Cheng C-Y, Misselwitz B, Brenner H, Ubels J, Schlander M. Cost-effectiveness of colorectal cancer screening strategies—a systematic review. Clin Gastroenterol Hepatol. 2019;17(10):1969-1981.e15. doi: 10.1016/j.cgh.2019.01.014
60. Esselen KM, Feldman S. Cost-effectiveness of cervical cancer prevention. Clin Obstet Gynecol. 2013;56(1):55-64. doi: 10.1097/GRF.0b013e3182823797
61. Ratushnyak S, Hoogendoorn M, van Baal PH. Cost-effectiveness of cancer screening: health and costs in life years gained. Am J Prev Med. 2019;57(6):792-799. doi: 10.1016/j.amepre.2019.07.027
62. Walter LC, Schonberg MA. Screening mammography in older women: a review. JAMA. 2014;311(13):1336-1347. doi: 10.1001/jama.2014.2834
63. Pataky R, Ismail Z, Coldman AJ, et al. Cost-effectiveness of annual versus biennial screening mammography for women with high mammographic breast density. J Med Screen. 2014;21(4):180-188. doi: 10.1177/0969141314549758
64. Booth N, Rissanen P, Tammela TL, et al. Cost-effectiveness analysis of PSA-based mass screening: evidence from a randomised controlled trial combined with register data. PLoS One. 2019;14(11):e0224479. doi: 10.1371/journal.pone.0224479
65. de Carvalho TM, Heijnsdijk EA, de Koning HJ. Comparative effectiveness of prostate cancer screening between the ages of 55 and 69 years followed by active surveillance. Cancer. 2018;124(3):507-513. doi: 10.1002/cncr.31141
66. Merker JD, Oxnard GR, Compton C, et al. Circulating Tumor DNA Analysis in Patients With Cancer: American Society of Clinical Oncology and College of American Pathologists Joint Review. J Clin Oncol. 2018;36(16):1631-1641. doi: 10.1200/JCO.2017.76.8671
67. Uzerman MJ, Berghuis AM, de Bono JS, Terstappen LW. Health economic impact of liquid biopsies in cancer management. Expert Rev Pharmacoecon Outcomes Res. 2018;18(6):593-599. doi: 10.1080/14737167.2018.1505505
68. Aravanis AM, Lee M, Klausner RD. Next-generation sequencing of circulating tumor DNA for early cancer detection. Cell. 2017;168(4):571-574. doi: 10.1016/j.cell.2017.01.030
69. Terry M. As liquid biopsies grow, who’s going to pay? Biospace.September 20, 2018. Accessed October 21, 2020. biospace.com/article/fd1a-as-liquid-biopsies-grow-who-s-going-to-pay-/
70. Social Security Administration. Exclusions from coverage and Medicare as secondary payer. 2019. Accessed October 21, 2020. ssa.gov/OP_Home/ssact/title18/1862.htm
71. Douglas MP, Gray SW, Phillips KA. Private payer and Medicare coverage for circulating tumor DNA testing: a historical analysis of coverage policies from 2015 to 2019. J Natl Compr Canc Netw. 2020;18(7):866-872. doi: 10.6004/jnccn.2020.7542
72.Centers for Medicare & Medicaid Services. Medicare Coverage Database. Proposed Local Coverage Determination (LCD): MolDX: Liquid Biopsies for Solid Organ Transplantation (DL38582). Published 2020. Accessed October 27, 2020. cms.gov/medicare-coverage-database/details/lcd-details.aspx?LCDId=38581&ver=3&name=238*2&bc=AQAAAIAAAAAA&
73. Centers for Medicare & Medicaid Services. Medicare Coverage Database. Proposed Decision Memo for Screening for Colorectal Cancer - Blood-Based Biomarker Tests (CAG-00454N). October 16, 2020. Accessed October 27, 2020. cms.gov/medicare-coverage-database/details/nca-proposed-decision-memo.aspx?NCAId=299
74. Centers for Medicare & Medicaid Services. Medicare Coverage Database. Local Coverage Determination (LCD): MolDX: Plasma-Based Genomic Profiling in Solid Tumors (L38168). Published 2020. Accessed October 27, 2020. cms.gov/medicare-coverage-database/details/lcd-details.aspx?LCDId=38168&ver=5&Cntrctr=All&UpdatePeriod=870&bc=AAAACAAAIAAA&
2 Commerce Drive
Cranbury, NJ 08512
AJMC®
All rights reserved.