- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Rheumatoid Arthritis Is a Risk Factor for Aortic Stenosis, Study Finds
Researchers add to evidence suggesting that inflammatory factors contribute to increased risk for valvular heart diseases, such as aortic stenosis, in patients with rheumatoid arthritis.
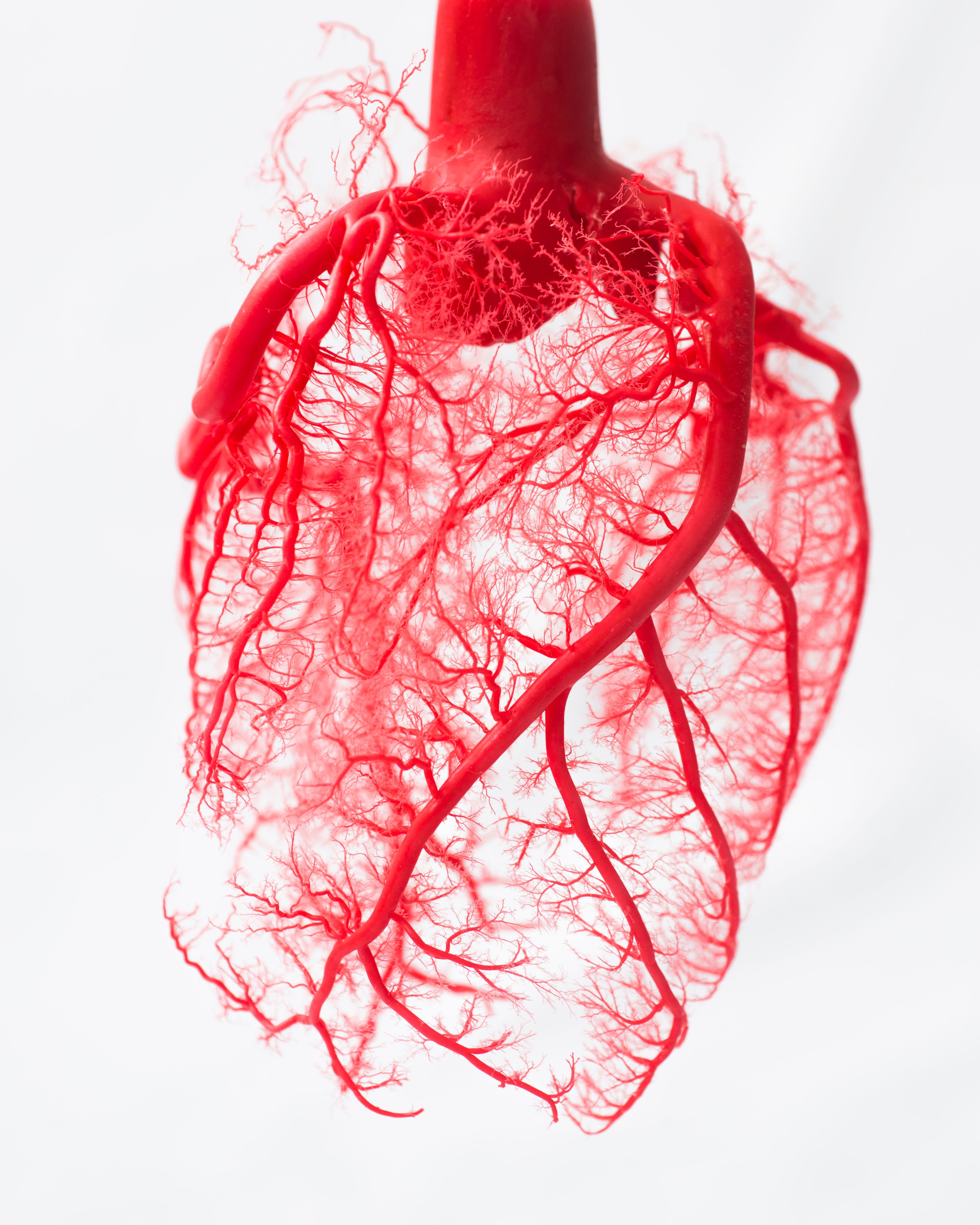
Heart Vessels | image credit: grieze - stock.adobe.com
Patients with rheumatoid arthritis (RA) were found to have an increased risk for developing aortic stenosis (AS), according to a study published in JAMA Internal Medicine.
The multitude of inflammatory factors brought on by RA has been affiliated with higher risk of cardiovascular disease (CVD). On top of this, CVD is the top contributing factor to mortality in patients with RA.
The authors note that patients with RA endure a 75% increased rate of death at the hands of valvular heart disease. The most common cause of valvular heart disease–related death, and the reason most associated with valve replacement, is AS. Although many past studies have correlated RA with forms of CVD, AS has yet to be sufficiently evaluated.
Given that a patient with RA’s vulnerability to developing AS is unknown, the researchers conducted a matched-cohort study to assess the risk of AS-related outcomes—such as aortic valve intervention—and disease development in these individuals.
Data were gathered between January 1, 2000, and December 31, 2019, from the national Veterans Health Administration (VHA) and CMS databases. Patients identified with RA were matched with up to 10 patients without RA (controls) according to age, sex, and year of enrollment in the virtual databases. Individuals were excluded if they had a history of aortic valve intervention or AS, and all were followed until the earliest AS outcome, end of the study period, or death.
AS risk factors were measured with test results for RA-related autoantibodies (rheumatoid factor [RF] and anti-cyclic citrullinated protein [anti-CCP]), erythrocyte sedimentation rates (ESR), and C-reactive protein (CRP) levels. Primary outcomes included AS incidence (official diagnosis, record of related death, or aortic valve intervention); secondary outcomes were concerned with the individual interventions that took place and AS-related death outcomes.
In total, 73,070 patients with RA were identified alongside 639,268 controls. By the end of the study period, 16,109 composite AS outcomes were registered that spanned 6,223,150 person-years. Of these, 2303 events were experienced by patients with RA.
The mean age of RA incidence between the RA group and controls were fairly similar (74.9 vs 75.5 years, respectively). For every 1000 person-years, having RA resulted in a 1.52-fold risk increase for AS-related events: 3.97 (95% CI, 3.81-4.13) vs 2.45 (95% CI, 2.41-2.49). Additionally, RA was associated with higher rates of composite AS (adjusted HR [aHR], 1.48; 95% CI, 1.41-1.55), aortic valve intervention (aHR, 1.34; 95% CI, 1.22-1.48), and AS-related death (aHR, 1.26; 95% CI, 1.04-1.54).
At baseline, 68.9% of patients with RA registered seropositive tests for RF or anti-CPP, and 47% had elevated CRP or ESR levels. In the authors’ results, these elevated levels and/or a seronegative test were linked with higher risk of developing AS. They found this important to note; however, they mentioned that these factors were not statistically significant in the outcomes.
The researchers’ findings aligned with those of previous RA cohorts that demonstrated these patients carried higher risks for developing other forms of CVD, such as ischemic heart disease. Their study further confirms the RA-CVD association and highlights that “valvular heart disease, specifically AS, may be an overlooked CVD complication in RA.”
While their research confirmed the increased risks carried by patients with RA, the authors concluded by expressing the need for further research on this matter to verify the role of conditions like AS in the CVD-related complications that coincide with RA.
Reference
Johnson TM, Mahabir CA, Yang Y, et al. Aortic stenosis risk in rheumatoid arthritis. JAMA Intern Med. 2023;183(9):973-981. doi:10.1001/jamainternmed.2023.3087
