
- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Review Outlines Shared Pathways Between CKD, VHD
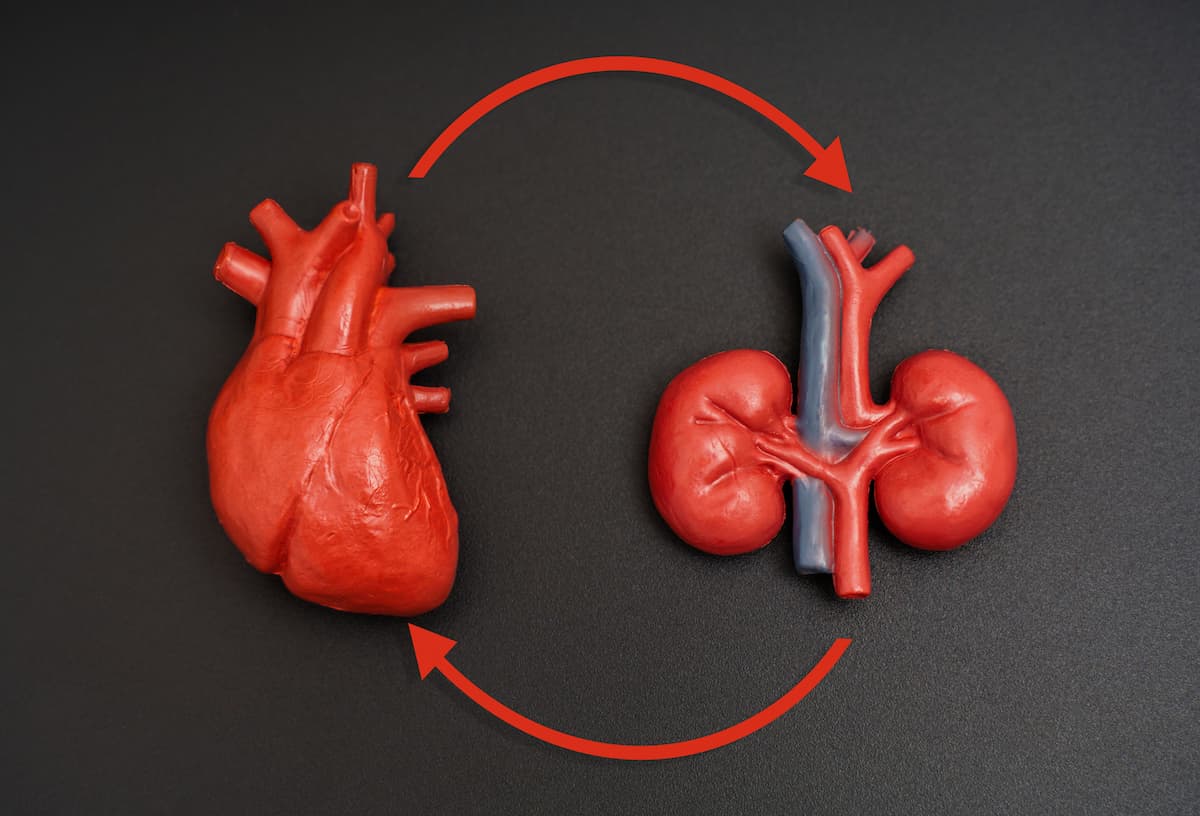
Overlapping metabolic mechanisms drive both chronic kidney disease (CKD) and valvular heart disease (VHD), a new review outlined.
Chronic kidney disease (CKD) and valvular heart disease (VHD) are increasingly recognized as interconnected conditions that amplify each other’s progression and worsen patient outcomes. In a new review appearing in Physiological Reports, researchers have outlined current evidence on how the 2 diseases share overlapping metabolic, inflammatory, and fibrotic pathways that drive their parallel progression.1
Managing metabolic disturbances early in CKD appears to be the most effective approach for reducing the risk of valvular complications. | Image credit: Katie Chizhevskaya - stock.adobe.com
CKD affects nearly 1 in 10 adults worldwide and is a known risk factor for cardiovascular disease, the leading cause of death in this population. Similarly, VHD is becoming more prevalent with aging populations, with over 5 million people in the US receiving a diagnosis each year.2 As populations age and CKD prevalence rises, addressing the interplay between these 2 diseases represents an urgent priority for improving cardiovascular outcomes worldwide.
Together, the 2 diseases pose significant diagnostic and management challenges. Patients often present late, and conventional imaging techniques may underestimate disease severity due to the atypical hemodynamics of uremic cardiomyopathy. Moreover, patients with CKD are less likely to undergo valve replacement surgery because of higher perioperative risks, frailty, and poor postoperative recovery. Yet delaying intervention can lead to rapid deterioration. The review emphasizes that decision-making in this setting must balance surgical risks with the high mortality associated with untreated valvular disease.
Throughout the review, published in Physiological Reports, the researchers outlined how the 2 disorders create a cycle of metabolic and hemodynamic stress where kidney dysfunction accelerates cardiac valve degeneration, and cardiac dysfunction worsens renal impairment.
The researchers call for a more integrated model of care, recognizing CKD and VHD as manifestations of a single systemic process rather than isolated diseases. They explain how the coexistence of CKD and VHD creates a non-coincidental interdependence rooted in shared molecular pathways. In CKD, the dysregulation of mineral metabolism, notably elevations in phosphate, fibroblast growth factor 23, and parathyroid hormone, promotes calcium deposition in vascular and valvular tissue. Oxidative stress and endothelial dysfunction further contribute to tissue remodeling and calcific degeneration.
The group explained that chronic inflammation, fueled by uremic toxins and cytokine release, accelerates fibroblast activation and extracellular matrix deposition in both kidneys and cardiac valves. Together, these processes establish a chronic inflammatory–fibrotic state that blurs the boundaries between renal and cardiac pathology.
In CKD, patients often develop calcification of the aortic and mitral valves as valvular interstitial cells transform into bone-like cells under uremic conditions. This process, driven by phosphate retention, oxidative stress, and inflammation, causes valve stiffening, blood flow obstruction, and increased strain on the heart.
The team of researchers called on the need for a multidisciplinary approach involving nephrologists, cardiologists, and surgeons to identify high-risk patients early and guide optimal timing for interventions such as transcatheter aortic valve replacement or surgical repair. Advances in biomarker research, including circulating calcification inhibitors like matrix Gla protein and fetuin-A, may also help stratify patients by progression risk.
Treatment options for these patients remain limited. Traditional cardiovascular drugs, such as statins, angiotensin-converting enzyme inhibitors, and phosphate binders, have shown mixed results in preventing calcification. The review notes growing interest in non-calcium-based phosphate binders, vitamin K supplementation, and agents targeting FGF23 or oxidative pathways, though large-scale trials are still lacking.
“The potential of non-calcium-based phosphate binders, vitamin D modulation (with attention to its biphasic effects), and antiresorptive therapies warrants further investigation, especially in targeted subgroups,” noted the researchers.
Managing metabolic disturbances early in CKD, including through pharmacologic control of phosphate and parathyroid hormone and strict blood pressure regulation, appears to be the most effective approach for reducing the risk of valvular complications.
References
1. Saltarocchi S, D’Abramo M, De Orchi P, et al. Chronic kidney disease and valvular heart disease: state of the art. Physiol Rep. 2025;13(18):e70544. doi:10.14814/phy2.70544
2. About heart valve disease. CDC. Published online September 30, 2024. Accessed October 26, 2025. https://www.cdc.gov/heart-disease/about/heart-valve-disease.html
2 Commerce Drive
Cranbury, NJ 08512
AJMC®
All rights reserved.