- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
A Review of Current Guidelines for the Treatment of Obesity
ABSTRACT
Two guidelines—one by the American College of Cardiology (ACC)/American Heart Association (AHA)/The Obesity Society (TOS), and the other by the American Association of Clinical Endocrinologists (AACE)/American College of Endocrinology (ACE)—remain the standard of care in the management of overweight and obesity in adults. However, since the publication of the ACC/AHA/TOS document, several relevant pharmacotherapies have been approved by the FDA, a medication was withdrawn from the market, and several procedures and device types for weight loss have been recommended or FDA-approved. Simultaneously, research in obesity treatment has advanced, and leaders in the field have issued complementary guidance. This article summarizes and synthesizes the 2013 ACC/AHA/TOS and the 2016 AACE/ACE guidelines and includes updates from more recent professional association guidance. Measurement of body mass index is recommended to initiate evaluation for overweight and obesity and determine disease classification. To stage disease severity, weight-related conditions should be assessed. Although lifestyle therapy remains the cornerstone of treatment for this disease, both pharmacotherapy and metabolic and bariatric surgery produce greater and more sustained weight loss in treatment-approved populations as compared with lifestyle modifications alone. An ongoing partnership between the patient and clinician is highly recommended to manage this serious, progressive, chronic disease.
Am J Manag Care. 2022;28(suppl 15):S288-S296. doi:10.37765/ajmc.2022.89292
For author information and disclosures, see end of text.
Introduction
In 2013, the American Medical Association (AMA) designated obesity as a chronic disease.1 In 2014, the American College of Cardiology (ACC), the American Heart Association (AHA), and The Obesity Society (TOS) published clinical practice guidelines for the management of overweight and obesity in adults.2 In 2016, the American Association of Clinical Endocrinologists (AACE) and American College of Endocrinology (ACE) published evidence-based clinical practice guidelines that built upon the AMA’s designation, the AACE’s novel diagnostic paradigm that incorporated both body mass index (BMI) and weight-related complications, and the AACE’s framework that suggested that weight-related complications rather than a universal weight-loss target determine treatment modality selection.3 These 2 comprehensive documents remain the most accepted guidelines for the treatment of obesity.
However, much has changed since the development of these 2 guidelines. After the critical questions of the ACC/AHA/TOS guideline were chosen and before the AACE/ACE guidelines were published, the FDA approved 4 new medications for the long-term treatment of obesity.2-7 Further, since publication of the AACE/ACE guidelines, another long-term anti-obesity medication (AOM) was approved, an AOM was withdrawn from the market, and several procedures and device types for weight loss and weight management were recommended or FDA-approved.4,8-11 These guidelines remain cornerstones for treatment for obesity. However, since their publication, input from the Centers for Disease Control and Prevention and several professional organizations—including the Endocrine Society, the National Institute of Diabetes and Digestive and Kidney Diseases, the American Society for Metabolic & Bariatric Surgery (ASMBS), the Obesity Medicine Association, and the American Society of Anesthesiologists—have advanced our understanding of the disease.12-14
This article summarizes and synthesizes the 2013 ACC/AHA/TOS guideline and the 2016 AACE/ACE guidelines and supplements that foundation with recent guidance from the aforementioned organizations. It also highlights consensus that obesity is a serious, progressive, and chronic disease.2,15,16
Screening and Diagnosis
Both guidelines recommend that all adults be screened annually using a body mass index (BMI) measurement (body weight [kg]/height [m2]) to initiate evaluation for overweight and obesity.2,3 The guidelines recommend that although a BMI of at least 25 kg/m2 in any patient prompts further evaluation, a BMI of at least 23 kg/m2 may herald the need for such evaluation in patients of South Asian, Southeast Asian, and East Asian genetic heredity, as health risks associated with overweight and obesity typically are observed at lower BMIs in these populations.2,3,17
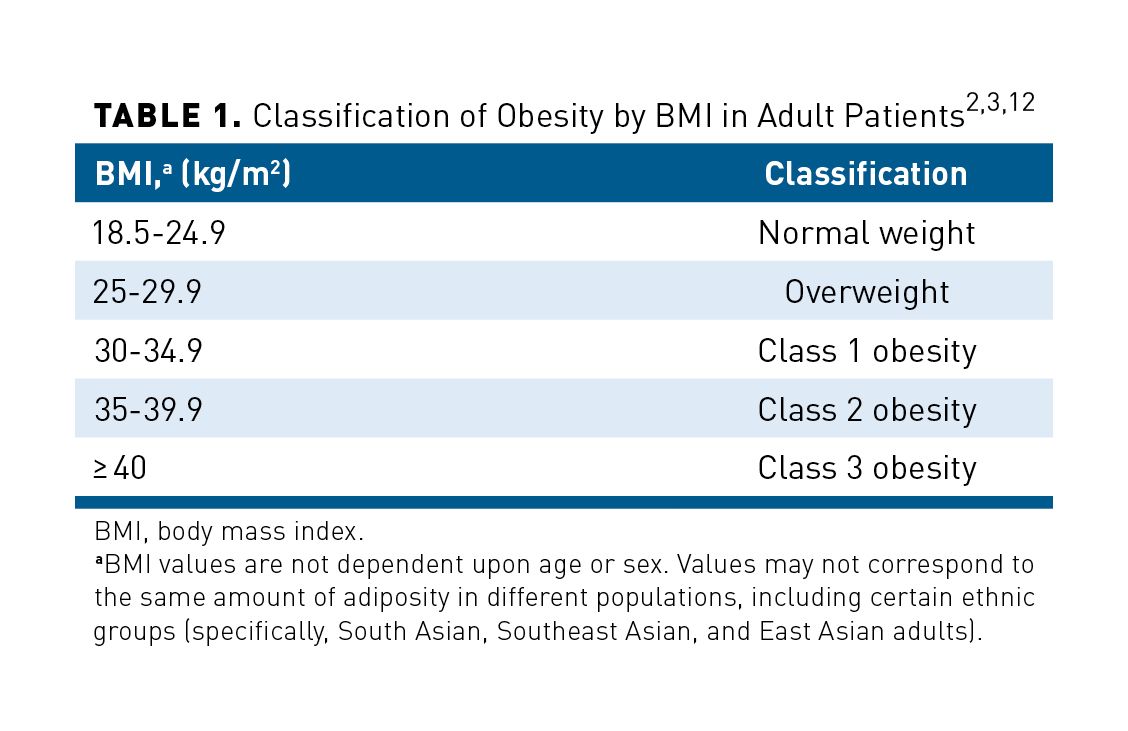
To diagnose obesity, both measurement of BMI and clinical assessment of weight-related complications are recommended.3 A BMI of 30 kg/m2 to 34.9 kg/m2 defines class 1 obesity, of between 35 kg/m2 and 39.9 kg/m2 constitutes class 2 obesity, and of at least 40 kg/m2 marks class 3 obesity (Table 1).2,3,12 However, age, sex, level of hydration, muscular composition, presence of fluid in noncirculatory (“third”) space, and presence of sarcopenia, edema, and high-volume tumors all should be considered before a classification is made.3 Classes 1, 2, and 3 are sometimes referred to as mild, moderate, and severe obesity, respectively.12,18-20 The AACE/ACE guidelines use these classes to indicate that a patient is at moderate, severe, or very severe risk of weight-related disease.3
Waist circumference also should be considered in patients having a BMI of 25 kg/m2 to 35 kg/m2. Waist circumferences of at least 102 cm (approximately 40 in.) in men and of at least 88 cm (approximately 35 in.) in women indicate abdominal obesity, which is associated with increased risk for adiposity-related disease.2,3 Lower thresholds (eg, ≥ 94 cm [≈ 37 in.] in men and ≥ 80 cm [≈ 32 in.] in women) are used outside of the United States; consideration of ethnicity and use of region-specific thresholds also may be used to measure disease risk.2,3 For instance, in patients of South Asian, Southeast Asian, and East Asian heredity, waist circumference of at least 85 cm (≈ 34 in) in men and at least 74 cm to 80 cm (29-32 in.) in women should be used to identify abdominal obesity.3,17
Clinical Assessment of Weight-Related Complications
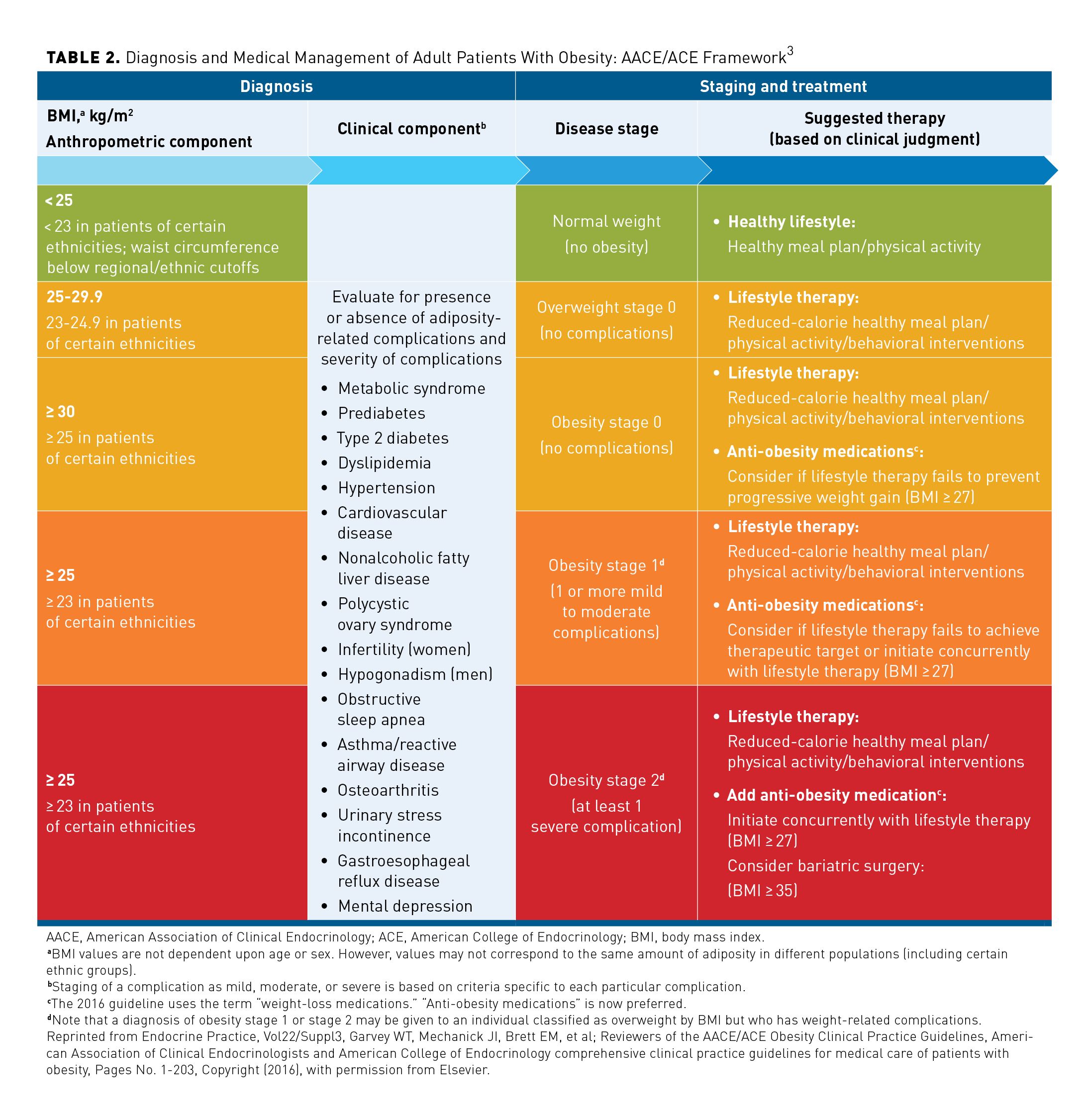
Patients with overweight or obesity should be screened for prediabetes, type 2 diabetes mellitus (T2D), dyslipidemia, hypertension, metabolic syndrome, cardiovascular disease, nonalcoholic fatty liver disease, osteoarthritis, and mental depression. These patients also should be evaluated for obstructive sleep apnea, asthma and reactive airway disease, and gastroesophageal reflux disease (Table 2).2,3
Women with overweight or obesity should be screened for urinary incontinence, and those who are premenopausal should be screened for reproductive abnormalities (eg, polycystic ovary syndrome). When suitable, women with overweight or obesity also should be advised of their heightened risk of infertility and of the lower success rates for assisted reproduction; a large body of evidence also correlates higher BMI with gestational diabetes and other obstetric and fetal complications.3,21 Men with obesity or an elevated waist circumference should be assessed for hypogonadism.3
Establishing Prevention and Treatment Targets
Measuring weight, assessing lifestyle, and taking a thorough and accurate medical history are key to assessing risk for overweight or obesity, determining whether and to what effect comprehensive lifestyle intervention and/or adjunctive therapies have been used, and evaluating therapeutic options.2,3 Patients with normal (healthy) weight (BMI, 18.5 to < 25 kg/m2) should be counseled on the health benefits of avoiding weight gain.2,12 Patients whose genetics, biomarkers, family history, ethnicity, cultural practices, or individual behaviors put them at high risk for overweight or obesity should be counseled to avoid weight gain and educated in healthy meal planning and physical activity.3
The presence and extent of weight-related complications should be evaluated among those with a BMI of at least 25 kg/m2 to establish prevention and treatment targets for each patient.2,3 Like the Edmonton Obesity Staging System, which incorporates weight-related complications into its staging of the disease, the AACE/ACE guidelines stage overweight and obesity based upon BMI and the presence, extent, and severity of these complications (Table 2).3,22 The treatment targets for patients with overweight stage 0 are to avoid additional weight gain or to lose weight and prevent both progression to obesity and development of complications.2,3
According to the ACC/AHA/TOS, patients with obesity should be assessed for their readiness to make lifestyle changes.2 Those who are ready should formulate with a clinician weight loss goals and complementary lifestyle treatment strategies.2 The recommended therapeutic targets for patients with obesity stage 0 are weight loss or prevention of additional weight gain coupled with prevention of complications.2,3 For patients with obesity stage 1 or obesity stage 2, weight loss is recommended; however, the AACE/ACE guidelines set complication-specific treatment targets (each of which includes weight loss and other clinical outcomes), whereas the ACC/AHA/TOS guideline recommends determining weight-loss goals in collaboration with the patient rather than according to weight-related complication.2,3
To prevent the progression, or lower the burden, of weight-related complications, both guidelines recommend that patients with obesity stage 1 or stage 2 lose at least 5% of their body weight; the AACE/ACE guidelines recommend a loss of at least 10% of body weight for many complication-specific targets.2,3 Because early weight loss helps predict sustained weight reduction, the AACE/ACE recommend targeting 2.5% weight loss within 1 month for all patients with overweight or obesity.3 The ACC/AHA/TOS guideline recommends that all patients with overweight or obesity achieve the realistic and meaningful goal of 5% to 10% weight loss within 6 months.2
Treatment
Managing obesity requires the ongoing partnership of a committed patient and informed clinicians.2 In patients given a diagnosis of overweight or obesity, adiposity and weight-related complications should be evaluated at regular intervals.3 Individuals with overweight or obesity who have lost weight should be advised to participate in a comprehensive weight loss maintenance program for at least 1 year.2 Weight-related complications should be managed in parallel with any treatment for overweight or obesity.2 Such management may or may not require additional therapy.3
Treatment for overweight and obesity
Weight management and weight loss are fundamental goals in treating overweight and obesity. Because an energy deficit is required for weight loss, a reduction in caloric intake forms the foundation of any weight-loss strategy.2,3 According to both guidelines, individuals with overweight or obesity who intend to lose weight should be prescribed aerobic exercise and resistance training along with a reduced-calorie diet, their active leisure-time pursuits should be promoted, and their sedentary time should be reduced.2,3 In addition, both guidelines recommend that patients pursue behavioral interventions that foster adherence to physical activity and meal plan prescriptions.2,3 Such interventions can include activities conducted by the individual (eg, goal setting, self-monitoring of food intake and physical activity), 1:1 sessions with clinicians (eg, cognitive behavioral therapy, dietary education), and group meetings (eg, gatherings with peers, use of social support structures).3 These interventions are often multidisciplinary, and they can include psychologists, psychiatrists, and dietitians; they can also be conducted remotely via telephone or Internet.3 The AACE/ACE guidelines recommend that behavioral interventions be escalated for patients who do not achieve 2.5% weight loss within 1 month of starting treatment.3
A structured and comprehensive lifestyle intervention program designed for weight loss (lifestyle therapy) that includes a healthy meal plan, physical activity, and behavioral intervention is recommended for all patients with overweight or obesity seeking to lose weight.2,3 An in-person, high-intensity program (≥ 14 sessions in 6 months) is recommended as the most effective behavioral treatment for overweight or obesity. The recommendation is based upon treatment efficacy; participation in such high-intensity programs produces approximately 5% to 10% body weight loss, on average, over 6 months.2 Especially when in-person, high-intensity intervention programs are not available, alternative programs (eg internet- or phone-based) with proven efficacy or referral to a nutrition professional may be prescribed.2
To improve adherence and outcomes, calorie-restricted diet, physical activity prescription, and behavioral lifestyle intervention should be individualized to each patient.2,3
Pharmacological treatment
Pharmacotherapy or AOMs used with lifestyle modifications produce greater and more sustained weight loss when compared with lifestyle modifications alone.2,3 The AACE/ACE guidelines recommend that this combination be considered for all individuals with a BMI of at least 27 kg/m2 if lifestyle therapy fails to halt weight gain; it is also recommended for individuals with obesity stage 2 (Table 2).3 AOM use and selection should be individualized based on clinical weight loss goals, weight-related conditions, and drug cautions and warnings.2,3
FDA-Approved Medications for the Long-Term Treatment of Obesity
At the time that the ACC/AHA/TOS guideline was being developed, only orlistat (Xenical; H-2 Pharma; OTC: Alli; GlaxoSmithKline) was FDA-approved for chronic weight management.2 Subsequently, AACE/ACE guidelines authors could offer guidance for orlistat, phentermine combined with topiramate (Qsymia; VIVUS), naltrexone combined with bupropion (Contrave; Currax Pharmaceuticals), liraglutide (Saxenda®; Novo Nordisk), and lorcaserin (Belviq; Arena Pharmaceuticals/Eisai), the last 4 of which had then been approved by the FDA for this indication.3 The Endocrine Society’s 2015 clinical practice guideline for the pharmacological management of obesity, to which the AACE/ACE guidelines refer,also considers orlistat, phentermine-topiramate, naltrexone-bupropion, liraglutide, and lorcaserin.3,23 In 2020, however, lorcaserin was withdrawn from the market due to concerns regarding adverse effects found with its use.4 In June 2021, the FDA approved semaglutide injection 2.4 mg subcutaneously once weekly (Wegovy®; Novo Nordisk) as an adjunct to a reduced calorie diet and increased physical activity for chronic weight management in patients with a BMI of at least 27 kg/m2 who have at least 1 weight-related complication or a BMI of at least 30 kg/m2.9 Thus, at the time of this publication, 5 drugs retain FDA approval for the long-term treatment of obesity (Table 3).3,5-8,23-29 A sixth medication, setmelanotide (Imcivree; Rhythm Pharmaceuticals), is only indicated for patients with 1 of 3 rare genetic disorders (POMC, PCSK1, or LR deficiency) as confirmed by genetic testing or those with Bardet-Biedl syndrome.13,30
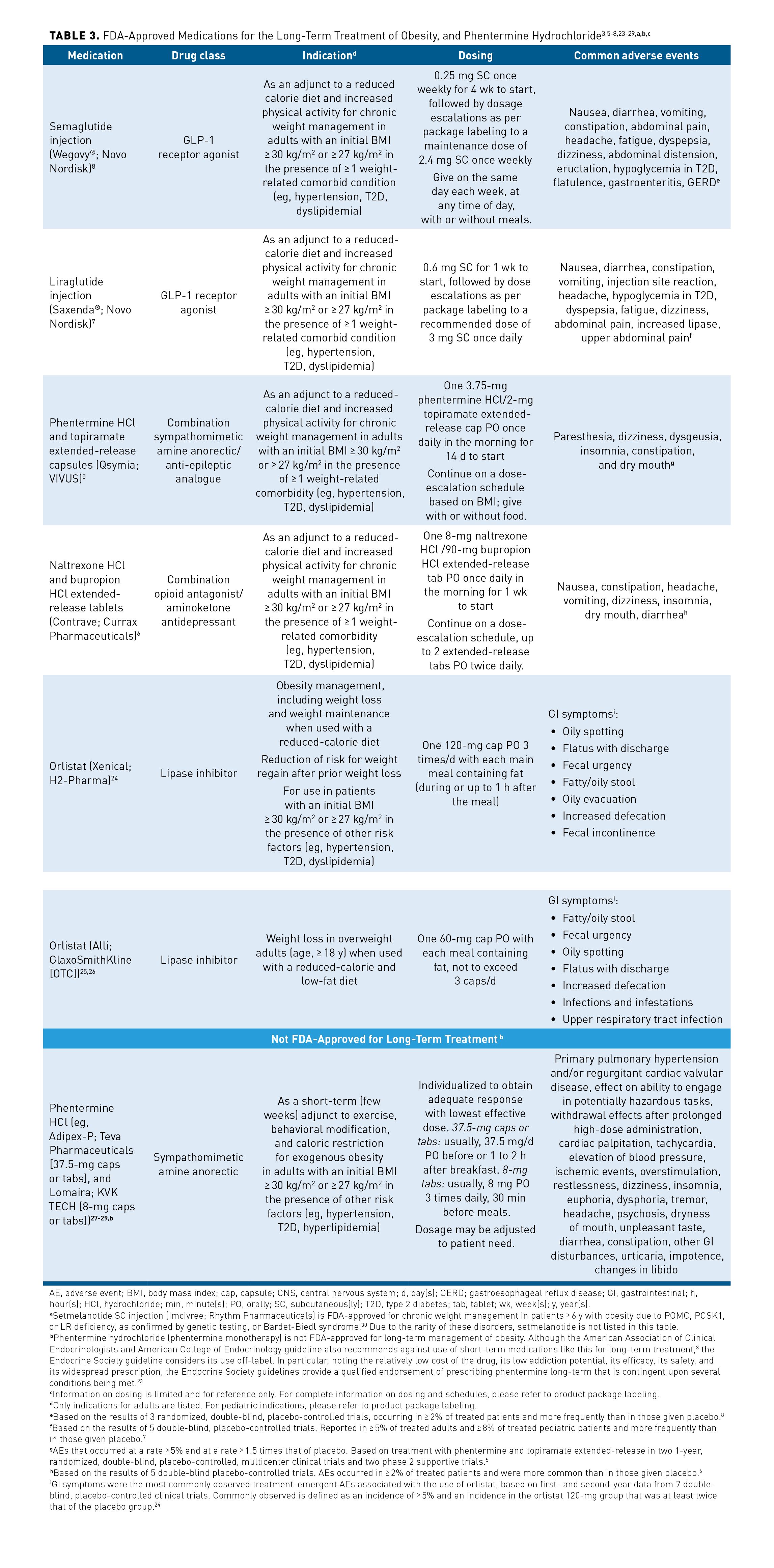
In November 2022, the American Gastroenterological Association (AGA) issued a new clinical practice guideline on pharmacological interventions for adults with obesity.31 Authors developed this guideline in response to the underuse of AOMs relative to mounting evidence from RCTs for the agents’ efficacy and to the increasing prevalence of obesity and related health conditions.31 In particular, the guideline advances those evidence-based recommendations from the ACC/AHA/TOS, the AACE/ACE, and the Endocrine Society discussed in this article with updated direction on currently available AOMs.31
The AGA guideline authors strongly recommend that an AOM be added to lifestyle intervention for adults with obesity who have had insufficient response to lifestyle intervention alone.31 Reiterating that AOM selection should be based on each patient’s needs, authors highlight that AOMs are generally used chronically to treat the chronic disease of obesity.31 Noting that total body weight loss reported in RCTs has ranged from 3.0% to 10.8% depending upon the pharmacological agent, AGA guideline authors identified that semaglutide 2.4 mg, liraglutide 3.0 mg, phentermine-topiramate extended release, and naltrexone-bupropion extended release had a balance of weight loss over harm that favored their use.31
AGA guideline recommendations are made for each AOM, and numbered.31 Table 3 reflects this order. The guideline states, “given the magnitude of net benefit, semaglutide 2.4 mg may be prioritized over other approved AOMs for the long-term treatment of obesity for most patients.”31 The guideline recommends against the use of orlistat.31
FDA-Approved Medications for Short-Term Weight Loss
Four drugs are currently available in the United States for short-term weight loss: phentermine (eg, Adipex-P; Teva Pharmaceuticals [37.5-mg capsules or tablets], and Lomaira; KVK Tech [8-mg capsules or tablets]), benzphetamine, diethylpropion, and phendimetrazine.13,32 Although the AACE/ACE guidelines recommend against use of these treatments, the Endocrine Society guideline considers the off-label use of phentermine for long-term treatment of obesity (Table 3).3,5-8,23-29 Phentermine has a relatively low cost and a low addiction potential and has shown efficacy and safety, and it is widely prescribed; the guideline provides a qualified endorsement of long-term prescription of phentermine that is contingent upon several conditions being met.23 The AGA guideline also provides a qualified endorsement of long-term prescription of phentermine, noting a low quality of evidence for this recommendation.31
Surgical Procedures and Devices for Weight Management
The ASMBS acknowledges the impact that language may have on weight bias and on treatment for obesity.33 To accurately reflect how encompassed procedures impact weight, metabolic health, and weight-related conditions, the ASBMS uses the term “metabolic and bariatric surgery” for what has been called “weight-loss surgery.”34 In patients with obesity, these procedures have led to the greatest weight loss, continuance of weight loss, and amelioration of weight-related complications and to decreased mortality.2,35 These procedures should be considered for patients with a BMI of at least 40 kg/m2 and for those with at least 1 severe weight-related condition and a BMI of at least 35 kg/m2 when therapeutic goals cannot be attained using structured lifestyle change and pharmacotherapy alone.3,14,36 Patients should be thoroughly evaluated before being recommended for a bariatric procedure.3,14 Risk, patient preferences, individualized therapy goals, and available procedural expertise should be considered when selecting a bariatric procedure.14
The AACE/ACE guidelines draw recommendations from the 2013 AACE/TOS/ASMBS clinical practice guidelines for support of the bariatric surgery patient.3 These bariatric surgery support guidelines were updated in 2019; they feature ASMBS-endorsed procedures, FDA-regulated devices, and emerging procedures and devices.14 Since then, the ASMBS has updated its recommended procedures (Table 4).10,14
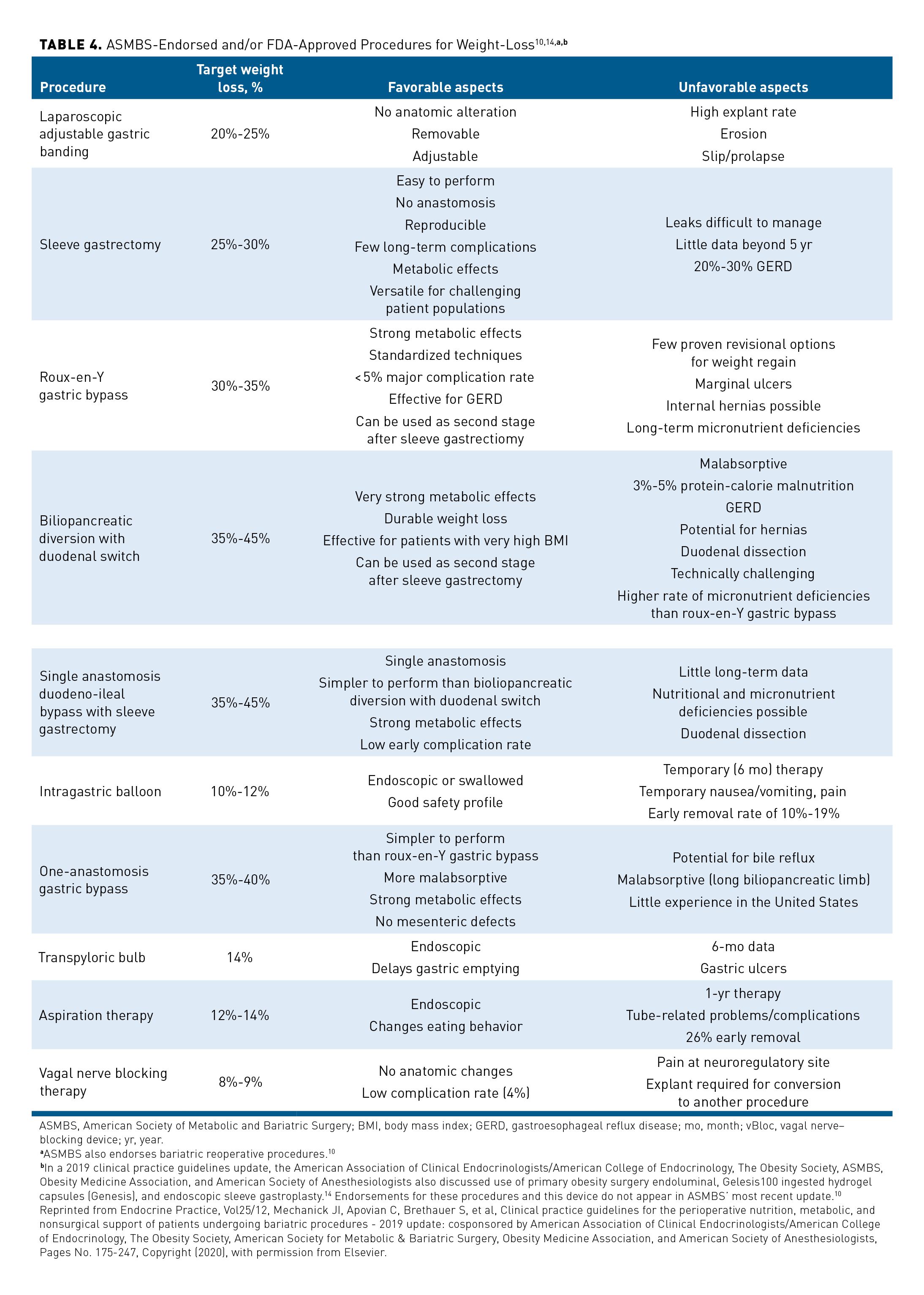
The ACC/AHA/TOS, AACE/ACE, and bariatric surgery support guidelines all recommend consideration of bariatric procedures for individuals with a BMI of at least 40 kg/m2 or a BMI of at least 35 kg/m2 with weight-related complications when such techniques would not place the patient at excessive risk.2,3,14 The AACE/ACE obesity guidelines and 2019 bariatric procedure guidelines add that patients with a BMI of at least 30 kg/m2 and T2D for whom glycemic levels remain insufficiently controlled after lifestyle therapy and pharmacotherapy also should be considered for a bariatric procedure.3,14
In a November 2022 statement, the ASMBS, along with the International Federation for the Surgery of Obesity and Metabolic Disorders, recommended that providers consider bariatric procedures for a larger patient population, including all patients with a BMI of 30 kg/m2 who do not attain and sustain desired weight loss or improvement in weight-related conditions.37 However, at the time that the current article was being written, the ACC, AHA, TOS, AACE, and ACE had not commented upon this statement. Whether other leading societies will endorse expanding eligibility for bariatric procedures remains to be seen.
Conclusions
Although much has changed in the field of obesity treatment since development of the most accepted guidelines, consensus remains: all adults should be screened annually for overweight and obesity using BMI, and weight-related complications should be assessed to formulate a diagnosis and to establish treatment targets.2,3 Lifestyle therapy that includes a healthy meal plan, physical activity, and behavioral intervention is the foundation of obesity treatment.2,3 In conjunction with lifestyle modifications, pharmacotherapy and metabolic and bariatric surgery produce greater and more sustained weight loss in treatment-approved populations when compared with lifestyle modifications alone.2,3 A sustained partnership between the patient and the clinician is necessary to manage the chronic disease of obesity.2
Acknowledgements
This peer-reviewed supplement was funded by Novo Nordisk Inc. The authors acknowledge the professional medical writing support from Clinical Communications, a division of MJH Life Sciences®, Cranbury, NJ, which received funding support from Novo Nordisk Inc, Plainsboro, NJ. Novo Nordisk Inc. provided scientific and medical accuracy review of this publication.
Author Affiliations: Medical University of South Carolina (MAC), Charleston, SC.
Funding Source: This supplement was supported by Novo Nordisk.
Author Disclosures: Dr Cornier reports serving as a paid consultant or paid advisory board member for Novo Nordisk.
Authorship Information: Concept and design (MAC); acquisition of data (MAC); analysis and interpretation of data (MAC); drafting of the manuscript (MAC); and critical revision of the manuscript for important intellectual content (MAC).
Address Correspondence to: Marc-Andre Cornier, MD, 96 Jonathan Lucas St, CSB 822, MSC 624, Charleston, SC 29425. Email: cornier@musc.edu
References
- American Medical Association House of Delegates, 2013. Recognition of obesity as a disease. Resolution 420 (A-13). National Public Radio. May 16, 2013. Accessed July 15, 2022. https://media.npr.org/documents/2013/jun/ama-resolution-obesity.pdf
- Jensen MD, Ryan DH, Apovian CM, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Obesity Society. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63(25 part B):2985-3023. doi:10.1016/j.jacc.2013.11.004
- Garvey WT, Mechanick JI, Brett EM, et al; Reviewers of the AACE/ACE Obesity Clinical Practice Guidelines. American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract. 2016;22(suppl 3):1-203. doi:10.4158/EP161365.GL
- Belviq, Belviq XR (lorcaserin) by Eisai: drug safety communication–FDA requests withdrawal of weight-loss drug. FDA. February 13, 2020. Accessed July 15, 2022. https://www.fda.gov/safety/medical-product-safety-information/belviq-belviq-xr-lorcaserin-eisai-drug-safety-communication-fda-requests-withdrawal-weight-loss-drug
- Qsymia. Prescribing information. VIVUS; 2022. Accessed July 15, 2022. https://hcp.qsymia.com/include/media/pdf/prescribing-information.pdf
- Contrave. Prescribing information. Currax Pharmaceuticals; 2021. Accessed July 15, 2022.
https://www.contravehcp.com/wp-content/uploads/Contrave_PI_MedGuide.pdf - Saxenda®. Prescribing information. Novo Nordisk; 2022. Accessed July 15, 2022. https://www.novo-pi.com/saxenda.pdf
- Wegovy®. Prescribing Information. Novo Nordisk; 2021. Accessed July 15, 2022. https://www.novo-pi.com/wegovy.pdf
- FDA approves new drug treatment for chronic weight management, first since 2014. FDA. June 4, 2021. Accessed July 15, 2022. https://www.fda.gov/news-events/press-announcements/fda-approves-new-drug-treatment-chronic-weight-management-first-2014
- ASMBS endorsed procedures and FDA approved devices. American Society for Metabolic & Bariatric Surgery (ASMBS). Updated May 11, 2022. Accessed July 13, 2022. https://asmbs.org/resources/endorsed-procedures-and-devices
- Weight-loss and weight-management devices. FDA. April 27, 2020. Accessed August 12, 2022. https://www.fda.gov/medical-devices/products-and-medical-procedures/weight-loss-and-weight-management-devices
- Defining adult overweight & obesity. Centers for Disease Control and Prevention. June 3, 2022. Accessed July 15, 2022. https://www.cdc.gov/obesity/adult/defining.html
- Prescription medications to treat overweight & obesity. National Institute of Diabetes and Digestive and Kidney Diseases. June 2021. Accessed July 15, 2022. https://www.niddk.nih.gov/health-information/weight-management/prescription-medications-treat-overweight-obesity
- Mechanick JI, Apovian C, Brethauer S, et al. Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures - 2019 update: cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic & Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Surg Obes Relat Dis. 2020;16(2):175-247. doi:10.1016/j.soard.2019.10.025
- Obesity: preventing and managing the global epidemic. Report of a WHO consultation. Geneva 2000. World Health Organ Tech Rep Ser. 2000;894:i-253. Accessed July 22, 2022. https://apps.who.int/iris/bitstream/handle/10665/42330/WHO_TRS_894.pdf?sequence=1&isAllowed=y
- Bray GA, Kim KK, Wilding JPH; World Obesity Federation. Obesity: a chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes Rev. 2017;18(7):715-723. doi:10.1111/obr.12551
- Bays HE, Shrestha A, Niranjan V, Khanna M, Kambhamettu L. Obesity pillars roundtable: obesity and South Asians. Obes Pillars. 2022;1(10006). doi.org/10.1016/j.obpill.2021.100006
- O’Brien PE, Dixon JB, Laurie C, et al. Treatment of mild to moderate obesity with laparoscopic adjustable gastric banding or an intensive medical program: a randomized trial. Ann Intern Med. 2006;144(9):625-633. doi:10.7326/0003-4819-144-9-200605020-00005
- Picot J, Jones J, Colquitt JL, Loveman E, Clegg AJ. Weight loss surgery for mild to moderate obesity: a systematic review and economic evaluation. Obes Surg. 2012;22(9):1496-1506. doi:10.1007/s11695-012-0679-z
- O’Brien PE, Brennan L, Laurie C, Brown W. Intensive medical weight loss or laparoscopic adjustable gastric banding in the treatment of mild to moderate obesity: long-term follow-up of a prospective randomised trial. Obes Surg. 2013;23(9):1345-1353. doi:10.1007/s11695-013-0990-3
- Yu CK, Teoh TG, Robinson S. Obesity in pregnancy. BJOG. 2006;113(10):1117-1125. doi:10.1111/j.1471-0528.2006.00991.x
- Sharma AM, Kushner RF. A proposed clinical staging system for obesity. Int J Obes (Lond). 2009;33(3):289-295. doi:10.1038/ijo.2009.2
- Apovian CM, Aronne LJ, Bessesen DH, et al. Pharmacological management of obesity: an endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2015;100(2):342-362. doi:10.1210/jc.2014-3415. doi:10.1210/jc.2015-1782
- Xenical. Prescribing information. H-2 Pharma; 2017. Accessed July 15, 2022. https://xenical.com/pdf/PI_Xenical-brand_FINAL.PDF
- Alli. Drug Facts. DailyMed. Revised November 2020. Accessed July 15, 2022. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=a2d3bd73-f3af-4ea5-a57c-66b0004cfe4f
- Anderson JW, Schwartz SM, Hauptman J, et al. Low-dose orlistat effects on body weight of mildly to moderately overweight individuals: a 16 week, double-blind, placebo-controlled trial. Ann Pharmacother. 2006;40(10):1717-1723. doi:10.1345/aph.1H234
- Adipex-P. Prescribing Information. Teva Pharmaceuticals USA; 2020. Accessed July 15, 2022. https://www.adipex.com/globalassets/adipex/adipex_pi.pdf
- Lomaira. Prescribing information. KVK-Tech; 2016. Accessed September 13, 2022. https://www.
lomaira.com/Prescribing_Information.pdf - Phentermine hydrochloride. Prescribing Information. 2016. DailyMed. Accessed September 22, 2022. https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=d8ddc6a0-29d0-4730-b718-1bdb2937a91c&type=displayA
- Imcivree. Prescribing information. Rhythm Pharmaceuticals; 2022. Accessed July 15, 2022. https://rhythm-vault-digital-publishing-production.s3.amazonaws.com/IMCIVREEPrescribingInformation.pdf
- Grunvald E, Shah R, Hernaez R, et al. AGA clinical practice guideline on pharmacological interventions for adults with obesity. Gastroenterology. 2022;163(5):1198-1225. doi:10.1053/j.gastro.2022.08.045
- Cohen JB, Gadde KM. Weight loss medications in the treatment of obesity and hypertension. Curr Hypertens Rep. 2019;21(2):16. doi:10.1007/s11906-019-0915-1
- Eisenberg D, Noria S, Grover B, Goodpaster K, Rogers AM; American Society for Metabolic and Bariatric Surgery Clinical Issues Committee. ASMBS position statement on weight bias and stigma. Surg Obes Relat Dis. 2019;15(6):814-821. doi:10.1016/j.soard.2019.04.031
- Bariatric surgery procedures. American Society for Metabolic & Bariatric Surgery. May 2021. Accessed July 15, 2022. https://asmbs.org/patients/bariatric-surgery-procedures
- Sjöström L, Narbro K, Sjöström CD, et al; Swedish Obese Subjects Study. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741-752. doi:10.1056/NEJMoa066254
- Shetye B, Hamilton FR, Bays HE. Bariatric surgery, gastrointestinal hormones, and the microbiome: an Obesity Medicine Association (OMA) clinical practice statement (CPS) 2022. Obes Pillars. 2022;2(1):1-20. doi:10.1016/j.obpill.2022.100015
- Eisenberg D, Shikora SA, Aarts E, et al. 2022 American Society for Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO): indications for metabolic and bariatric surgery. Surg Obes Relat Dis. 2022. Published online October 18, 2022. doi:10.1016/j.soard.2022.08.013

