- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Review Highlights Potential for Bispecific Antibodies in DLBCL
Investigators are optimistic about bispecific antibodies (BsAbs) for patients with diffuse large B-cell lymphoma (DLBCL), especially the possibility of combining different BsAbs with distinct targets for stronger treatment outcomes.
Bispecific antibodies (BsAbs) have emerged as promising options for patients with diffuse large B-cell lymphoma (DLBCL) in recent years, including for those who are unable to receive or have progressed on CD19-directed chimeric antigen receptor (CAR) T-cell therapies, according to a review published in Blood Cancer Journal.
DLBCL is the most common type of non-Hodgkin lymphoma, and incidence is rising annually along with average population age, the investigators wrote. Despite improvements in treatment options, 30-40% of diagnosed patients will die due to disease complications, emphasizing the need for a strong front-line treatment option.
CD19-directed CAR T-cell therapies are a preferred option for patients with relapsed or refractory DLBCL, with 2 products—axicabtagene ciloleucel (axi-cel) and lisocabtagene maraleucel (liso-cel)—approved for second-line treatment and 1 product, tisagenlecleucel (tisa-cel), approved in the third line or later. Notably, axi-cel and liso-cel demonstrated superior progression-free survival (PFS) compared with standard chemoimmunotherapy, according to the investigators.
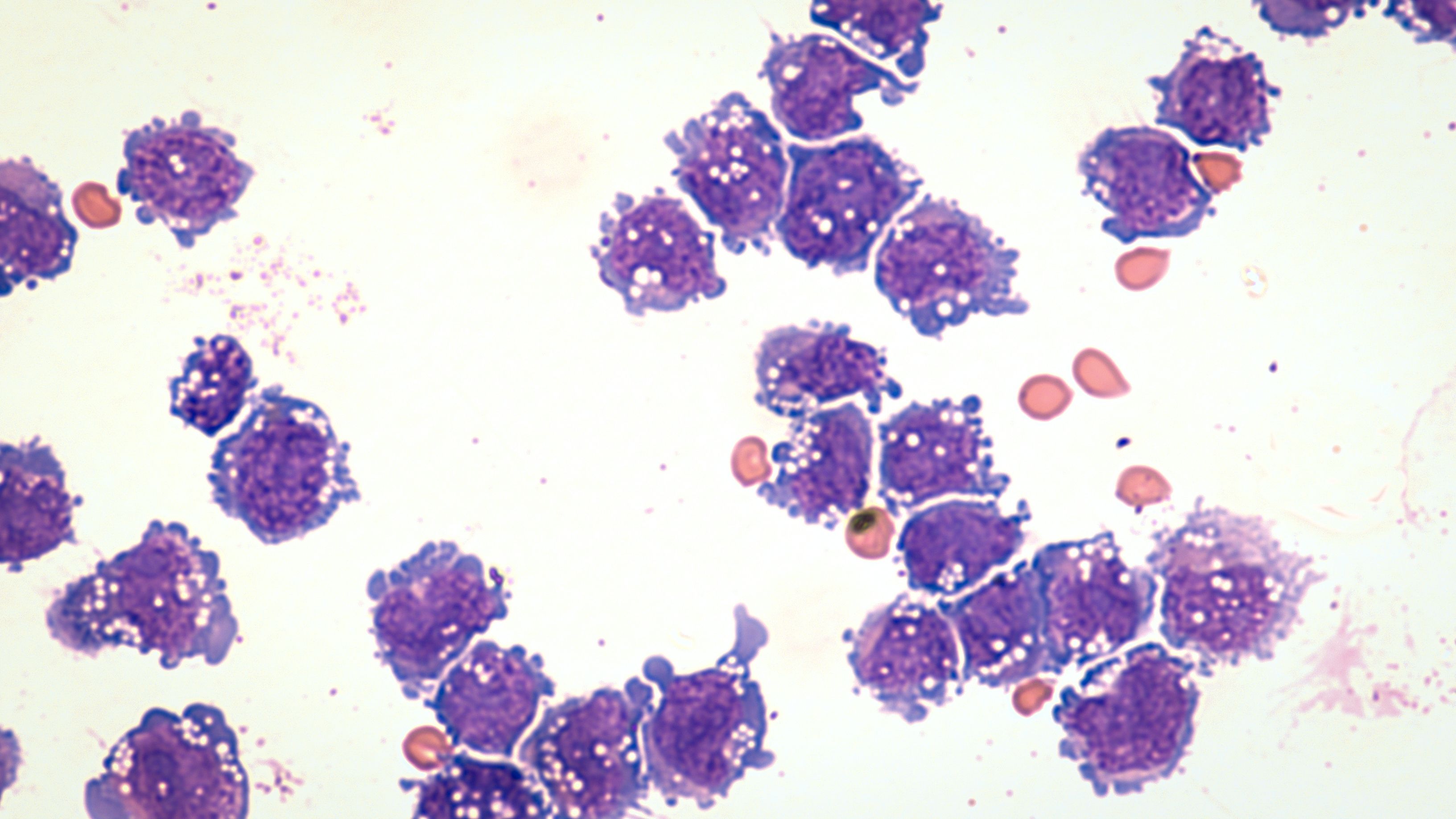
Microscopic image of diffuse large B-cell lymphoma | Image credit: David A Litman - stock.adobe.com
The strong PFS and accompanying long-term data have illustrated the curative potential of CAR T-cell therapies, but the treatment option has shortcomings related to logistical challenges and potentially serious adverse events (AEs), the investigators wrote.
Disparities in treatment also exist due to a lack of access to CAR T-cell therapies stemming from geographic and socioeconomic factors. Furthermore, it can be an exhaustive process to be certified to utilize CAR T-cell treatment at a center, with certification taking 6-18 months. Further, recent guidance from the FDA highlights a risk for secondary T-cell malignancies after CAR T-cell therapy, the investigators wrote.
These shortcomings have made the study of BsAbs in treating DLBLC of increased importance. Two bispecifics, epcoritamab and glofitamab, were granted approval in 2023, making them the first BsAbs to be approved for DLBCL, according to the investigators.
Epcoritamab treatment resulted in a strong overall response rate (ORR) of 75%, with no grade 3 toxicities reported, the investigators wrote. Additionally, glofitamab was successful in targeting DLBCL, leading to complete responses (CRs) in 78% of patients in a study at 12 months. The investigators discussed the development and clinical testing of other BsAbs, such as odronextamab and mosunetuzumab, that are nearing FDA approval.
Given these results, the reviewers determined that BsAbs are safe and efficacious in patients with DLBCL, including in historically hard-to-treat populations of patients following treatment with CAR T cells. The authors wrote that BsAbs appear to have less AEs, potentially making them a safer option for sicker patients, and that they could be ideal for use in combination with other treatments—a concept that they note has not been thoroughly explored.
Another consideration for patients and payers would be cost. The authors of the review discussed the prospect of a full BsAb treatment regimen being comparable in cost—or perhaps more expensive—than a single CAR T-cell treatment dose after factoring in the costs of ancillary health care and direct treatment. The investigators advocated for future direct cost-effectiveness comparisons between the two treatments.
Instead of targeting CD20, as most BsAbs currently approved or under development do, some trials have reported on novel targets such as CD47 or simultaneous targeting of CD19 on B-cells and 4-1BB on T-cells. These could allow patients to receive multiple BsAbs with different targets during their treatment. Trials have shown promising results so far, but the study authors cautioned that further studies are required to determine the long-term feasibility of such treatments.
Overall, the investigators are optimistic of the potential around BsAbs for patients with DLBCL, especially the possibility of combining different BsAbs for stronger treatment outcomes.
“With varying targets, it’s conceivable patients may be able to receive multiple BsAbs during their cancer treatment journey, with the ultimate goal of prolonging the lives of patients with DLBCL,” the review authors concluded.
Reference
Trabolsi A, Armumov A, Schatz JH. Bispecific antibodies and CAR-T cells: dueling immunotherapies for large B-cell lymphomas. Blood Cancer J. 14, 27 (2024). doi:10.1038/s41408-024-00997-w
Frameworks for Advancing Health Equity: Pharmacy Support for Non-Hodgkin Lymphoma
December 19th 2024Rachael Drake, pharmacy technician coordinator, University of Kansas Health System, explains how her team collaborates with insurance companies and providers to support treatment access for patients with non-Hodgkin lymphoma.
Listen
Fixed-Duration Epcoritamab Shows Strong Responses in Older, Chemo-Ineligible Patients With LBCL
December 27th 2025In the EPCORE DLBCL-3 study, fixed-duration epcoritamab monotherapy delivered deep, durable responses with manageable toxicity in older, chemotherapy-ineligible patients with LBCL.
Read More
Study Identifies Key Predictors of Successful CD3+ Cell Apheresis for CAR T Manufacturing in DLBCL
December 9th 2025A small set of pre-apheresis biological factors can reliably predict whether patients with DLBCL will achieve the T cell collection efficiency needed for successful CAR T manufacturing
Read More
