
- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Regional Benchmarking or Regional Bonus? Sustainability in the Medicare Shared Savings Program
In healthcare, the “volume-to-value” movement seeks to align the interests of healthcare providers with the societal triple aim of better care, better health, and lower costs. The devil, as always, is in the details.
The goal of good policy in a market economy is to align individual incentives with societal good. Successful policy creates an environment where public welfare is furthered not only by direct government action and grants, but also by private organizations acting in their own interests.
In healthcare, the “volume-to-value” movement seeks to align the interests of healthcare providers with the societal triple aim of better care, better health, and lower costs. The devil, as always, is in the details. If providers are to be credited for generating savings, then we must answer the question: “Compared to what?”
Many, including myself here in this space and elsewhere, have advocated that the best representation of new value creation is a “difference-in-difference” approach to calculating savings. To measure savings, as researchers at Harvard have done, we should ask whether a Medicare beneficiary had lower cost trends in the accountable care organization (ACO) than he or she would have not in the ACO.
In 2016, CMS responded by introducing a regional benchmarking methodology for ACOs that enter a second or third contract in the Medicare Shared Savings Program. Unfortunately, CMS made a small decision with large implications that were not initially appreciated. It included the ACO’s own population in the comparison group. This has 2 effects, which ramp up as the ACO’s share of the county population increases.
First, in order to demonstrate recognized savings, ACOs must fight against the very progress they are creating. A rural ACO with 50% market share would have to generate 6% real savings in order to be recognized for a 3% savings against regional trend. Second, the ill effects of this policy are further amplified by a policy that caps an ACO’s risk score but incorporates any increase in the risk and complexity profile of an ACO’s population in the region’s risk score. Every ACO loses calculated savings compared to regional trends whether their risk score increases or decreases. These policies systematically disadvantage rural ACOs compared with urban ones, discourage ACOs from moving to 2-sided risk, and reduce the social good created by the Medicare Shared Savings Program. Thankfully both situations are relatively straightforward for CMS to address.
First, let’s dig into the policy weeds.
Fighting Against Their Own Progress
The year before an ACO starts its contract performance, CMS compares the risk-adjusted costs of ACO beneficiaries in a given year with the risk-adjusted costs of all assignable beneficiaries, including those in the ACO in the same region. By including the ACO’s beneficiaries, CMS decreases any regional efficiency of the ACO in direct proportion to its market share in the region.
For example, if an ACO with market share of 30% and risk-adjusted costs of $9000 is in a region where other beneficiaries have risk-adjusted costs of $10,000, the ACO should have a $1000 regional efficiency factor. But by including the ACO’s beneficiaries in the regional comparison group, the regional average drops to $9700 lowering the ACO’s true regional efficiency by exactly 30%. In a large urban area with 5% market share this could be hand waved away; however, in rural areas, where even a small ACO can have significant market share, it can be devastating to an ACO’s financial prospects. This is then further compounded each year by the regional trend factor.
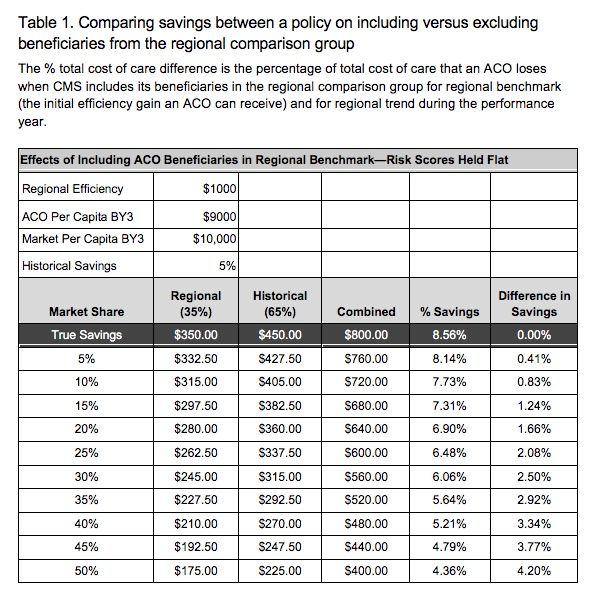
If our ACO then reduces costs by 5% in its performance year, it is giving 1.5% (5% x market share) of its savings back to CMS through its inclusion in the regional trend factor. The combined effect on regional benchmark and regional trend means that our ACO with 30% market share loses out on 2.7% of its savings against total cost of care, which could easily be the difference between meeting the minimum savings rate and receiving no shared savings check at all. Table 1 shows the effects of this policy at various levels of market share.
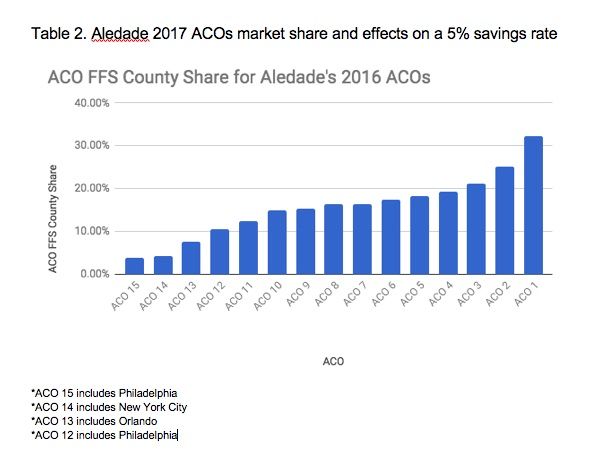
For some real-life perspective, Aledade operated 15 ACOs in 2017 with a range of 3.8% to 32.2% market share (Table 2).
This is a very solvable problem for CMS. Simply do not include the ACO beneficiaries in the regional comparison. The only specific reason CMS gave for doing so was concern over small numbers in certain rural areas. Medicare Advantage has dealt successfully with this problem for many years by expanding the region. It is the rural areas that are most harmed by this policy, so it should not be that they are the excuse for policy that secrets away savings from ACOs.
ACO Risk Score Cap
Example: If the ACO’s risk score increases, then the region’s risk score increases in proportion to the ACO’s market share. This creates a negative regional trend lowering the ACO’s benchmark. In an equitable situation, the ACO’s benchmark would increase due to ACO’s risk adjustment, more than offsetting the negative regional trend. But CMS will not allow the risk score to increase for the ACO’s continuously enrolled population, creating a no-win situation for the ACO.
If the ACO’s risk score decreases, then its benchmark decreases proportionally due to risk adjustment. If the ACO’s risk score increases, then its benchmark decreases due to regional trends. Heads CMS wins, tails the ACO loses.
To fix the effects this has on the regional trend, CMS should apply the same risk methodology to both the ACO and its regional comparison group.
The second policy that distorts regional benchmarking is capping the risk score for the ACO, but not for the comparison group. The math here is even more challenging for a blog post, but conceptually this is how it would work. A population with a risk score of 1.1 and a per capita cost of $10,000 is considered 10% more efficient than a population with a risk score of 1.0 and a per capita cost of $10,000. In the below example, we assume that costs and non­-ACO risk scores stay constant for the region and the ACO:
There is also more at stake when it comes to risk than shifting savings from the ACO to CMS using the regional trend. By capping the risk score for the ACOs, CMS is saying it does not trust that the increases in an ACO’s risk score reflect an increase in the real risk of the population. However, CMS then uses the increase when it benefits the agency to do so. If CMS is truly concerned that some ACO risk growth is due to coding and not underlying morbidity, it could again follow MA’s lead and do an industry-wide, across-the-board offset to coding increases, but still recognize relative differences in risk scores among ACOs. This would not only fix the regional trend issue but also make better use of risk scoring in the entire Medicare Shared Savings Program.
In conclusion, CMS creates a proxy of regional benchmarking. CMS said it created the regional benchmark to improve the incentives for ACOs to generate savings, but these 2 policies clearly undercut that purpose. This is particularly concerning giving the all-or-nothing approach of the MSR and the much greater harm imposed on rural areas through this policy. Thankfully these are 2 policy decisions that are straightforward to correct within the existing framework.
2 Commerce Drive
Cranbury, NJ 08512
AJMC®
All rights reserved.