- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Real-World Data Show Bevacizumab Benefits Only High-Risk Patients With Epithelial Ovarian Cancer
In line with previous clinical trial findings, real-world data show that bevacizumab improves outcomes in patients with epithelial ovarian cancer and high-risk prognostic factors.
The real-world benefit of adding bevacizumab to a first-line chemotherapy regimen for patients with epithelial ovarian cancer was limited to those with high-risk prognostic factors, according to a study published Monday in Cancer.1
In the phase 3 GOG-0218 trial (NCT00262847), adding bevacizumab to first-line chemotherapy followed by bevacizumab maintenance therapy significantly prolonged progression-free survival (PFS) in patients with newly diagnosed, incompletely resected stage 3 or 4 epithelial ovarian cancer compared with chemotherapy alone (HR, 0.72; 95% CI, 0.63-0.82).2
Similarly, the phase 3 ICON7 trial (NCT00483782) found that first-line chemotherapy plus bevacizumab followed by bevacizumab maintenance significantly improved PFS in patients with high-risk early-stage or advanced epithelial ovarian cancer compared with placebo after a median follow-up of 19 months (HR, 0.81; 95% CI, 0.70-0.94).3
However, neither trial demonstrated overall survival (OS) improvements among their patient populations.1 Despite this, post hoc analyses suggested that patients with high-risk prognostic factors, defined as having stage 4 disease or stage 3 disease with either visible residual disease or no documentation of surgery, derived greater benefit from the addition of bevacizumab to first-line chemotherapy.
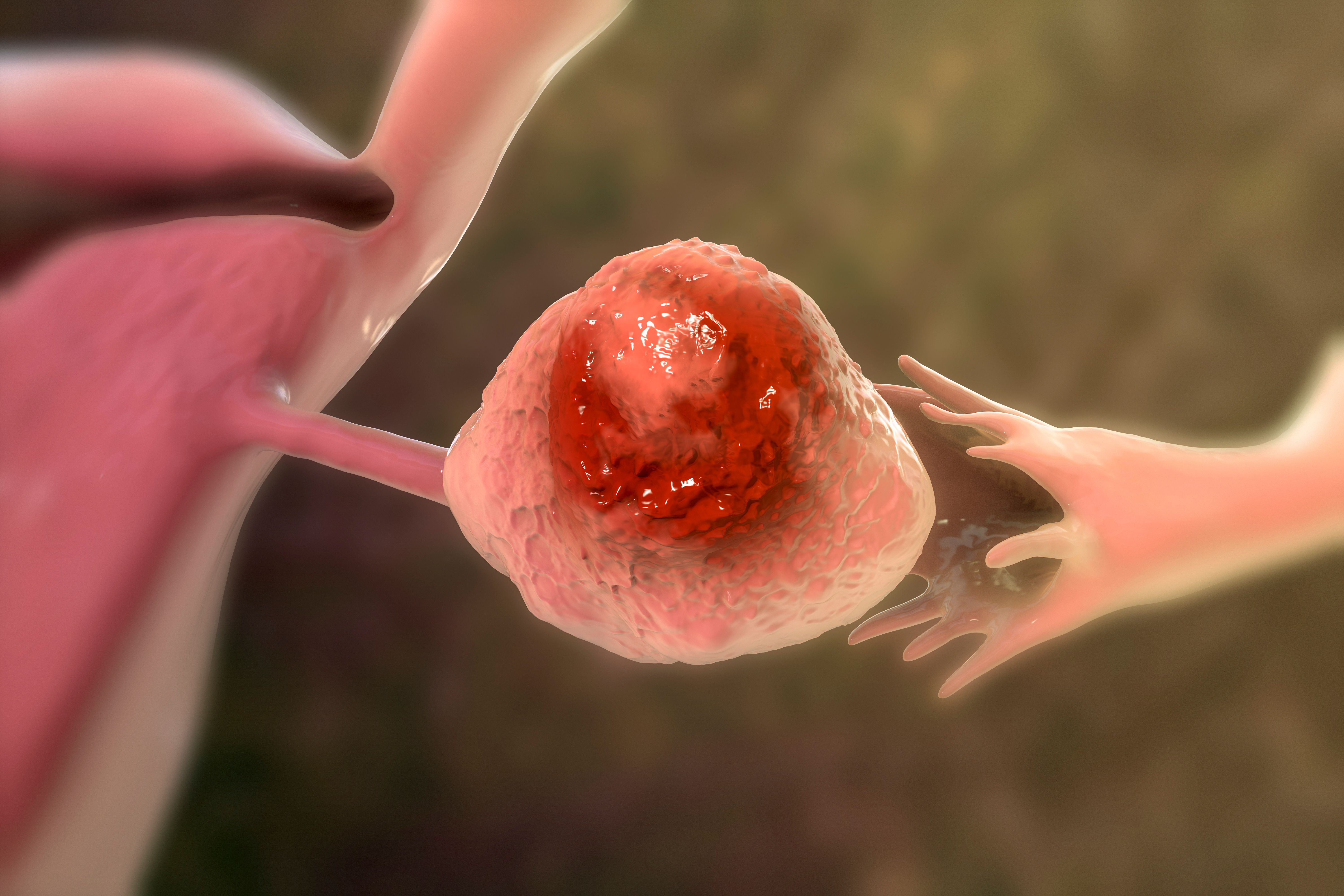
In line with previous clinical trial findings, real-world data show that bevacizumab improves outcomes in patients with epithelial ovarian cancer and high-risk prognostic factors. | Image Credit: Dr_Microbe - stock.adobe.com
The researchers explained that the treatment landscape has significantly evolved since the GOG-0218 and ICON7 trials were conducted more than 10 years ago. With additional maintenance treatment options now available, they highlighted the need for contemporary real-world data to identify which patients benefit most from bevacizumab.
To address this gap, the researchers conducted BEV1L, a real-world, retrospective, observational study designed to describe the demographic and clinical characteristics of patients with epithelial ovarian cancer treated with first-line platinum-based chemotherapy with or without bevacizumab. The study also evaluated real-world clinical outcomes associated with adding bevacizumab to first-line platinum-based chemotherapy in patients with and without high-risk prognostic factors.
The study utilized the Flatiron Health database, a nationwide, real-world data source comprising information from about 280 cancer clinics. Eligible patients were females diagnosed with ovarian cancer on or after January 1, 2016. Additional inclusion criteria required patients to be aged 18 or older, have confirmed epithelial histology, and present with stage 3 or 4 disease at diagnosis.
All patients received a first-line platinum-based chemotherapy regimen, initiated between January 1, 2017, and May 31, 2023, with or without bevacizumab. The researchers categorized patients into cohorts based on bevacizumab use, which they further stratified by the presence or absence of high-risk prognostic factors.
Median real-world time to next treatment and real-world OS, indexed to the start of first-line therapy, was estimated using Kaplan-Meier methods. The index was defined as the date of first-line treatment initiation, and follow-up continued until death, the last electronic health record activity, or the study end date (August 31, 2023), whichever occurred first.
The study included 1753 patients who met all eligibility criteria. The median (IQR) age was 68 (60-75) years, and the median (IQR) follow-up duration was 18.5 (8.0-36.6) months.
Among the study population, 1240 patients (70.8%) received first-line chemotherapy alone, while 512 (29.2%) received first-line chemotherapy plus bevacizumab. Of the 1208 patients with high-risk prognostic factors, 826 (68.4%) received first-line chemotherapy alone and 382 (31.6%) received first-line chemotherapy plus bevacizumab.
In patients with high-risk prognostic factors, the observed median real-world time to next treatment was significantly longer in the bevacizumab group compared with chemotherapy alone (13.6 months [95% CI, 12.7-15.9] vs 11.7 months [95% CI, 10.6-12.6]; HR, 0.85; 95% CI, 0.73-0.99; P = .03). In contrast, no significant difference in real-world time to next treatment was observed for patients without high-risk prognostic factors.
Additionally, the observed median real-world OS was numerically longer for patients with high-risk prognostic factors in the bevacizumab group than for those who received chemotherapy alone (31.1 months [95% CI, 27.7-37.5] vs 27.4 months [95% CI, 25.1-31.2]). However, the difference did not reach statistical significance (HR, 0.84; 95% CI, 0.70-1.00; P = .052).
Among patients without high-risk prognostic factors, the researchers observed no benefit in OS with the addition of bevacizumab. More specifically, the observed median real-world OS was 61.4 months (95% CI, 48.3-not reached) for those who received first-line chemotherapy plus bevacizumab compared with 63.2 months (95% CI, 55.1-not reached) among patients who received chemotherapy alone (HR, 1.03; 95% CI, 0.68-1.55; P = .90).
Lastly, the researchers acknowledged several limitations to their analysis, one being that the database primarily comprised community oncology centers and only included patients treated in the US. As a result, the findings may not be generalizable to patients receiving care at academic centers or outside of the US. Despite their limitations, they expressed confidence in their results and highlighted the need for further research.
“…these real-world results remain consistent with findings from the ICON7 and GOG-0218 trials and suggest that the clinical benefit from the addition of bevacizumab to 1L [first-line] chemotherapy may be largely limited to patients with high-prognostic factors,” the authors concluded. “These results also suggest a need to better understand why the addition of bevacizumab provides a greater clinical benefit in specific patient subgroups.”
References
- Duska LR, Lim J, Boyle ATC, et al. The BEV1L study: do real-world outcomes associated with the addition of bevacizumab to first-line chemotherapy in patients with ovarian cancer reinforce clinical trial findings? Cancer. 2025;e35821. doi:10.1002/cncr.35821
- Burger RA, Brady MF, Bookman MA, et al. Incorporation of bevacizumab in the primary treatment of ovarian cancer. N Engl J Med. 2011;365(26):2473-2483. doi:10.1056/nejmoa1104390
- Perren TJ, Swart AM, Pfisterer J, et al. A phase 3 trial of bevacizumab in ovarian cancer. N Engl J Med. 2011;365(26):2484-2496. doi:10.1056/nejmoa1103799
