- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Rates of Elevated LDL-C Have Decreased, but Awareness, Treatment Still Suboptimal
The prevalence of severely elevated low-density lipoprotein cholesterol (LDL-C) has declined in recent decades, but 1 in 17 US adults in a recent analysis had levels of LDL-C that would warrant consideration of pharmacotherapy, and 1 in 48 had high levels of LDL-C that are indicated for medication.
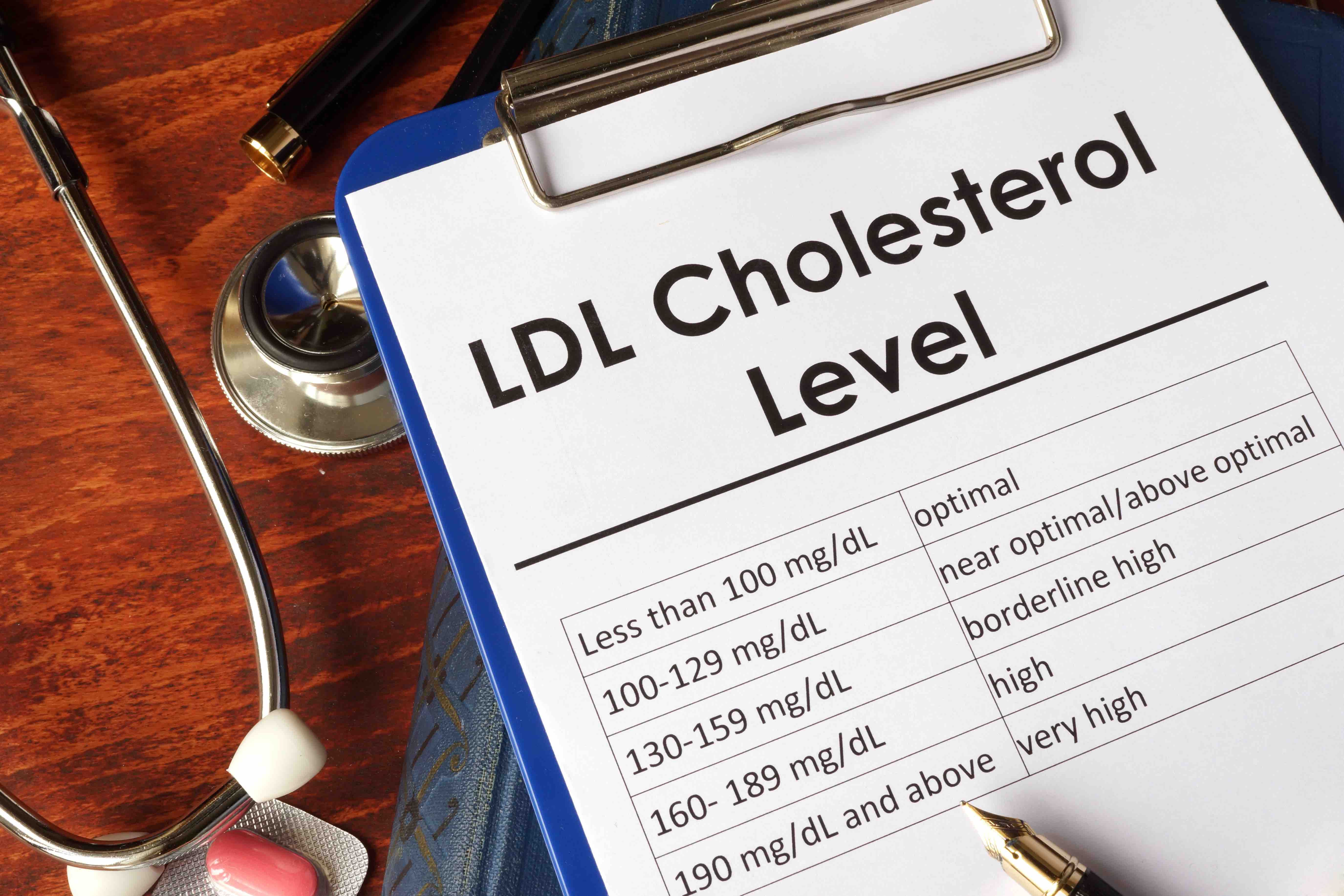
LDL cholesterol chart | Image credit: Vitalii Vodolazskyi - stock.adobe.com
Despite longstanding recommendations for the management of low-density lipoprotein cholesterol (LDL-C), a recent study found a lack of awareness and treatment of LDL-C in the United States, particularly among non-Hispanic Black, Hispanic, and socioeconomically disadvantaged persons. The findings were published in a research letter in JAMA Cardiology.1
The prevalence of severely elevated LDL-C has declined, the authors noted, but 1 in 17 US adults in the analysis had levels of LDL-C that would warrant consideration of pharmacotherapy, and 1 in 48 had high levels of LDL-C that are indicated for medication.
The cross-sectional study included data from 23,667 participants in 10 consecutive cycles of the National Health and Nutrition Examination Survey between 1999 and 2020. The survey combines interviews and examinations to monitor the health and nutritional status of US adults and children.2 In the study, participants were stratified by awareness and treatment levels, and logistic regression analysis was used to investigate temporal trends.1
Among participants who were unaware if their LDL-C had been measured or were never informed of having elevated LDL-C and those classified as untreated (meaning medications did not include a statin, ezetimibe, bile acid sequestrant, or proprotein convertase subtilisin/kexin type 9 inhibitor), the prevalence of being unaware or untreated was also assessed by age, sex, self-reported race and ethnicity, highest level of education, poverty index, and insurance status.
Overall, 1851 (7.8%) participants had an LDL-C level of 160 to 189 mg/dL, which is high enough to consider pharmacotherapy, and 669 (2.8%) had an LDL-C level higher than 190 mg/dL, which is indicated for pharmacotherapy.
Adjusting for age, the prevalence of having an LDL-C level between 160 and 189 mg/dL declined from 12.4% (95% CI, 10.0%-15.3%) from 1999 to 2000 to 6.1% (95% CI, 4.8%-7.6%) in the 2017-2020 survey cycle (P < .001). The prevalence of an LDL-C level of 190 mg/dL or higher also declined, with a rate of 3.8% (95% CI, 2.8%-5.2%) in 1999-2000 vs 2.1% (95% CI, 1.4%-3.0%) in 2017-2020 (P = .001).
The proportion of participants who were unaware and untreated for an LDL-C level of 160 to 189 mg/dL dropped from 52.1% (95% CI, 41.0%-63.0%) in 1999-2000 to 42.7% (95% CI, 33.6%-52.3) in 2017-2020. The proportion of those with an LDL-C level of 190 mg/dL or higher who were unaware and untreated also declined, with a rate of 40.8% (95% CI, 26.9%-56.3%) in the 1999-2000 survey and 26.8% (95% CI, 12.6%-48.2%) in the 2017-2020 survey cycle.
Younger adults, men, racial and ethnic minority groups, individuals with lower education attainment, lower-income individuals, and uninsured individuals were more commonly unaware and untreated for elevated LDL-C.
“This lack of awareness and treatment may be due to difficulties accessing primary care, low rates of screening in primary care, lack of consensus on screening recommendations, insufficient emphasis on LDL-C as a quality measure, and hesitance to treat asymptomatic individuals,” the authors wrote.
Although the study was limited by a small number individuals whose cholesterol was above 190 mg/dL, potential nonresponse bias, and the reliance on patient reporting of whether LDL-C was measured previously, the authors concluded that awareness and treatment of LDL-C elevation is suboptimal in the United States despite improvements in recent decades.
Reference
1. Sayed A, Navar AM, Slipczuk, et al. Prevalence, awareness, and treatment of elevated LDL cholesterol in US adults, 1999-2020. JAMA Cardiol. Published online November 1, 2023. doi:10.1001/jamacardio.2023.3931
2. National Health and Nutrition Examination Survey. CDC. Updated October 31, 2023. Accessed November 5, 2023. https://www.cdc.gov/nchs/nhanes/index.htm
