- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Quality of Life Lower in Patients Without Rectal Cancer Recurrence Receiving Radiotherapy
Patients who received radiotherapy without a recurrence of rectal cancer had significantly lower quality of life compared with patients who did not receive radiotherapy.
Patients who did not receive radiotherapy (RT) during the follow-up period after surgery for rectal cancer were found to have a significantly higher quality of life (QOL) compared with patients who received radiotherapy without recurrence, according to a study published in BJS Open.1
Rectal cancer is often treated with neoadjuvant RT, as it can reduce local recurrence rates through reducing the tumor burden prior to resection.2 However, overall survival (OS) has been limited. The proportion of patients who receive RT differs by country, and is as low as 33% of patients in Norway and as high as 76% of patients in the Netherlands, according to 2019 data. Long-term effects of RT on QOL have not been studied previously, which prompted the researchers of this study to focus on the long-term effects on QOL in patients who had curative treatment of rectal cancer. This study also aimed to assess the impact of RT on QOL.
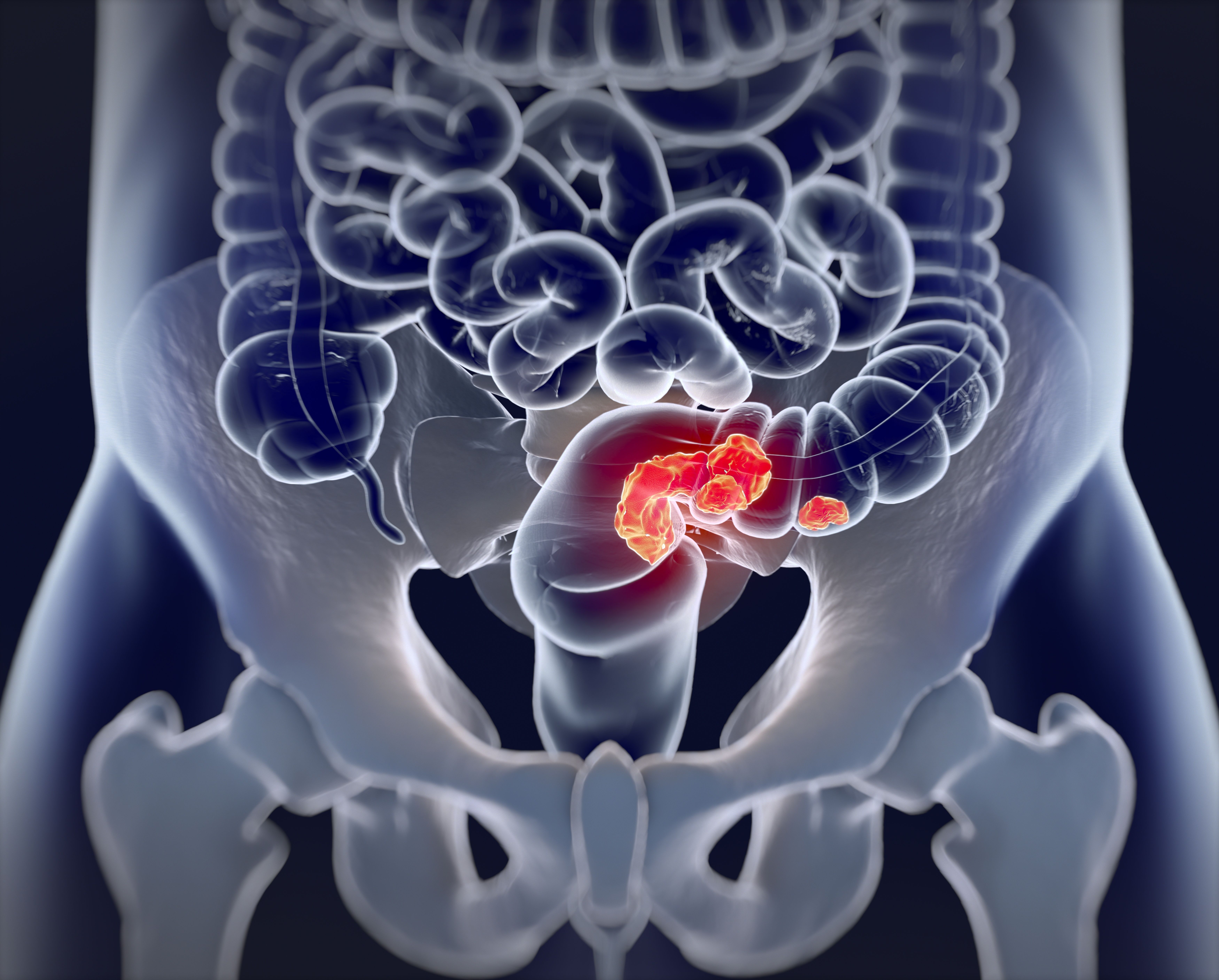
Radiotherapy can affect quality of life in patients receiving surgery for rectal cancer | Image credit: Anatomy Insider - stock.adobe.com
The researchers performed a retrospective cross-sectional cohort study based on data from the Norwegian Patient Registry. Patients were eligible if they had a surgery for rectal cancer between September 30, 2007, and October 1, 2020, and were 75 years or older. Patients with dementia, any recurrence, or distant metastasis at diagnosis were excluded from the study. Patients participated by completing an online questionnaire, which they were invited to take part in through invitations sent in October of 2021.
The primary outcome measure was the Gastrointestinal QoL Index (GIQLI), which was made up of 36 items, each scored on a scale of 0 to 4. The best QOL was indicated by a score of 144 whereas the worst QoL was indicated by a score of 0. Other questionnaires completed by the participants included the Short Form Health Survey, Scale for Chemotherapy-Induced Long-Term Neurotoxicity, and Low Anterior Resection Syndrome. Data on sex, age, operation date, time since surgery, tumor location, and American Society of Anesthesiologists classification were collected.
There were 2142 patients who had surgery for rectal cancer without recurrence and who answered the questionnaire who were included in the study. RT was received by 36% of the patients, the mean (SD) follow-up time was 6.4 (3.5) years, and 40.4% were women. The mean age of the patients was 62 years.
Patients without a stoma had significantly different mean GIQLI scores (RT, 102.8 [18.6] vs no RT, 110.9 [19.4]; mean difference, –8.1; 95% CI, –10.53 to –5.67). The result remained statistically significant in patients with a stoma (RT, 105.4 [20.6] vs no RT, 111.0 [20.4]; mean difference, –5.7; 95% CI, –8.73 to –2.59). Patients who had or had not received RT had significantly different GIQLI scores overall (mean difference, –7.0; 95% CI, –8.72 to –5.19). The Short Form Health Survey also found that 7 of the 8 domains were lower in patients who received RT.
There were some limitations to this study. There was a response rate of only 43%, which was low, and the main baseline characteristics had only small differences between the participants. Some of the values in the registry data also were missing, including tumor location.
The researchers concluded that the frequent use of RT in patients with rectal cancer should be reevaluated given these data on the decrease in perceived QOL. Patients with a lower risk of recurrence should have other options in the neoadjuvant setting and in treatment regimens intended to preserve their organs.
References
1. Malik YG, Benth JS, Hamre HM, Færden AE, Schultz JK. Effect of radiotherapy on long-term quality of life in recurrence-free rectal cancer survivors (LaTE study): nationwide inverse probability of treatment-weighted registry-based cohort study and survey. BJS Open. 2024;8(5):zrae091. doi:10.1093/bjsopen/zrae091
2. Feeney G, Sehgal R, Sheehan M, et al. Neoadjuvant radiotherapy for rectal cancer management. World J Gastroenterol. 2019;25(33):4850-4869. doi:10.3748/wjg.v25.i33.4850
