- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Pulmonary Arterial Hypertension: Updates in Epidemiology and Evaluation of Patients
Abstract
Group 1 pulmonary hypertension (or pulmonary arterial hypertension) is a rare, highly complex, and progressive disorder that is incurable and ultimately can lead to premature death. PAH causes significant physical, social, work, and emotional burdens among affected patients and their caregivers. Early diagnosis and initiation of treatment is required for best outcomes; however, the clinical presentation of PAH is nonspecific and frequently overlaps with several other conditions, often leading to a delay in diagnosis or misdiagnosis. In the past decades, increased understanding of the pathobiology of PAH has led to changes in its definition. Additionally, contemporary PAH registries have shown greater survival rates among patients with PAH and have allowed for the development of risk calculator tools that are now used to drive therapeutic goals. To date, multiple PAH-specific therapies have been developed, and all currently target one of 3 pathways that contribute to the endothelial dysfunction pathogenesis of PAH (prostacyclin, endothelin, and nitric oxide pathways). Because PAH is classified into 7 subgroups, it is essential that individuals are grouped appropriately for the efficacy of treatment and avoidance of harm. As health-related quality of life for PAH is multifactorial, it is important that patients are involved in the clinical decision-making process and have access to multidisciplinary care. The purpose of this review is to update healthcare professionals on the management of PAH with the most current information on epidemiology, pathophysiology, clinical presentation, and diagnostic considerations.
Am J Manag Care. 2021;27(3):S35-S41. https://doi.org/10.37765/ajmc.2021.88609
Introduction
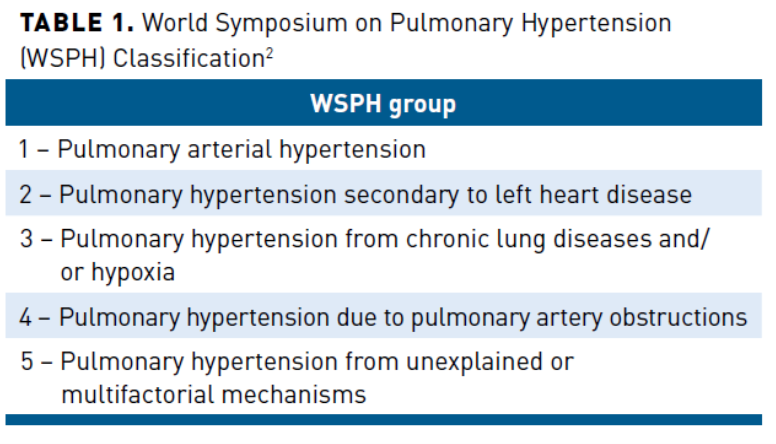
Pulmonary hypertension (PH) describes a group of severe pulmonary vascular disorders characterized by elevated mean pulmonary arterial pressure (mPAP) at rest.1 The World Symposium on Pulmonary Hypertension (WSPH) categorizes pulmonary hypertension into 5 groups (Table 1).2 Pulmonary arterial hypertension (PAH), which corresponds to group 1 PH, and a focus of this article, is a complex and devastating disease that causes progressive vasoconstriction and vascular remodeling of the distal pulmonary arteries.3 Currently, there is no cure, and the majority of patients with PAH go on to develop right heart dysfunction leading to death. Due to the progressive nature of PAH, it is crucial that the disease is diagnosed early with an accurate classification. Patients with PAH also must undergo a thorough evaluation to ascertain the severity of disease and future risk, and ideally have access to treatment at specialized care centers.1
The past 2 decades have been marked by significant advancements leading to novel therapeutics and improved understanding of the pathogenesis of PAH. As a result, the management of PAH is rapidly evolving.
Classification and Etiology of PAH
PAH includes several subgroups, all having similar pulmonary vascular pathobiology, clinical characteristics, and management strategies (Table 2).4-6 PAH can be idiopathic, heritable, caused by drugs or toxins, or associated with other conditions such as connective tissue disease, congenital heart disease, or pulmonary hypertension.1 Idiopathic PAH is responsible for more than 50% of all PAH cases. It requires extensive investigation (diagnosis of exclusion), whereas heritable PAH results from gene mutations or familial cases regardless of mutations.7 The 6th WSPH updated the group 1 pulmonary hypertension classification to include new drugs and toxins as known agents associated with PAH.6 For example, amphetamines, methamphetamines, and dasatinib were added to the definite association category.8 Leflunomide, bosutinib, and direct-acting antivirals for hepatitis C virus (eg, sofosbuvir) were added as agents having a possible association.9-15
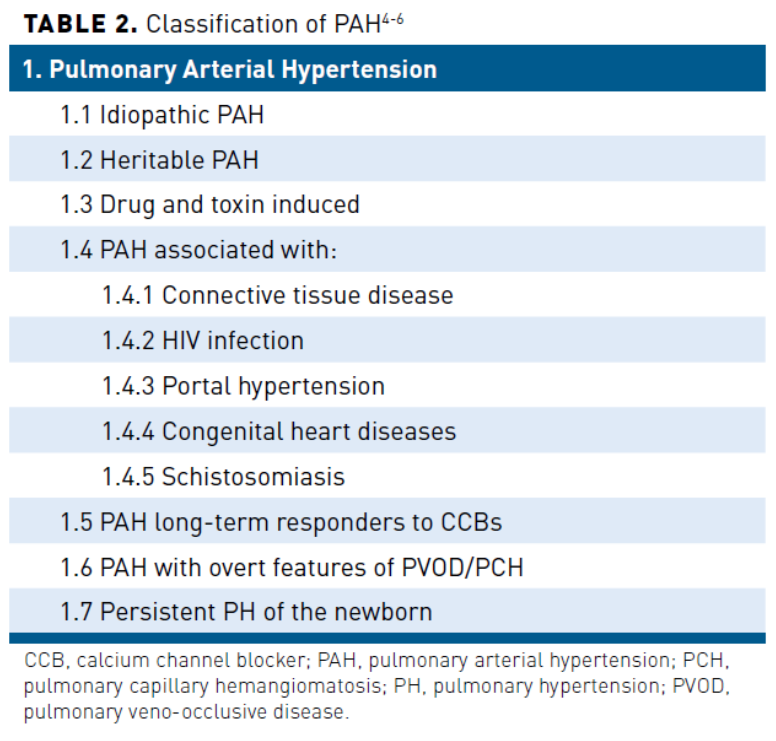
A small subset of patients with PAH presenting with overt features of venous/capillary involvement was also recognized as a distinct category. Pulmonary veno-occlusive disease and/or pulmonary capillary hemangiomatosis (PVOD/PCH) were moved to a subset within group 1 as opposed to the prior iteration of the WSPH, where they were designated as group 1.1,2 Typically, individuals with PVOD/PCH have similar clinical presentations and hemodynamic profiles as those with PAH; however, they have poorer prognosis, limited response to PAH treatment, and are at high risk for developing pulmonary edema from PAH therapeutics.16 A separate group of individuals with long-term response to calcium channel blockers was included in the updated clinical classification based on accumulating improved survival data in this small subset of patients.1,17
Epidemiology
PAH is a rare disorder found in 15 to 50 persons per million within the United States and Europe.1 Idiopathic, heritable, and anorexigen-induced PAH make up 52.6% of all PAH cases. Generally, PAH affects women aged between 30 and 60 years. However, it can occur in males and is often associated with worse clinical outcomes.7 The National Institutes of Health (NIH) was a landmark registry that collected PAH data between 1981 and 1985.5,18 This registry included 187 individuals having PAH of various etiologies. The registry largely consisted of females, found a mean age of PAH presentation of 36 years, and was primarily Caucasian. PAH-specific therapies were not available at this time, and registry participants had a median survival of 2.8 years (1 year, 68%; 3 year, 48%; and 5 year, 34%).5,18
Significant progress in the field of PAH pathophysiology and treatment have occurred in the 2 decades since the NIH registry. Contemporary PAH registries vary in their study populations, study design, and cohorts. The 2002 French Network on Pulmonary Arterial Hypertension (French PAH) registry included 674 people with PAH.19 The French PAH registry found an estimated survival rate among those with idiopathic/familial/anorexigen-associated PAH of 82.9% at 1 year and 58.2% at 3 years.20 This is a markedly higher survival rate compared with the NIH registry but consistent with other more recent PAH registry findings.5,18,21
REVEAL (Registry to Evaluate Early and Long-Term PAH Disease Management) is a contemporary, multicenter, observational, US-based registry that began in 2006.22 In contrast to the NIH registry, REVEAL was specifically designed to ascertain demographics, longitudinal clinical course, and management of PAH from a current US perspective.21,23 Baseline characteristics for the 2967 individuals who met traditional hemodynamic criteria included a mean age of 53 (±14 years) and female sex in 79.5% with a female-to-male ratio of 4.8:1.24 In addition, 46% of individuals had idiopathic PAH, 25% were associated with connective tissue diseases, and 10% were associated with congenital heart diseases. There was also a mean duration between symptom onset and diagnosis of 2.8 years.25 Results of the REVEAL Registry showed a 1-year survival rate of 91% among 2716 individuals who were enrolled consecutively.26 An additional analysis assessing long-term survival (N = 2635, between March 2006 and December 2009) found survival rates of 85% at year 3, 68% at year 5, and 49% at year 7 from time of diagnosis.19 These increases in survival were attributed to various factors, including changes in treatment, increased patient support, and potentially, a difference in the PAH population cohort.
Pathogenesis
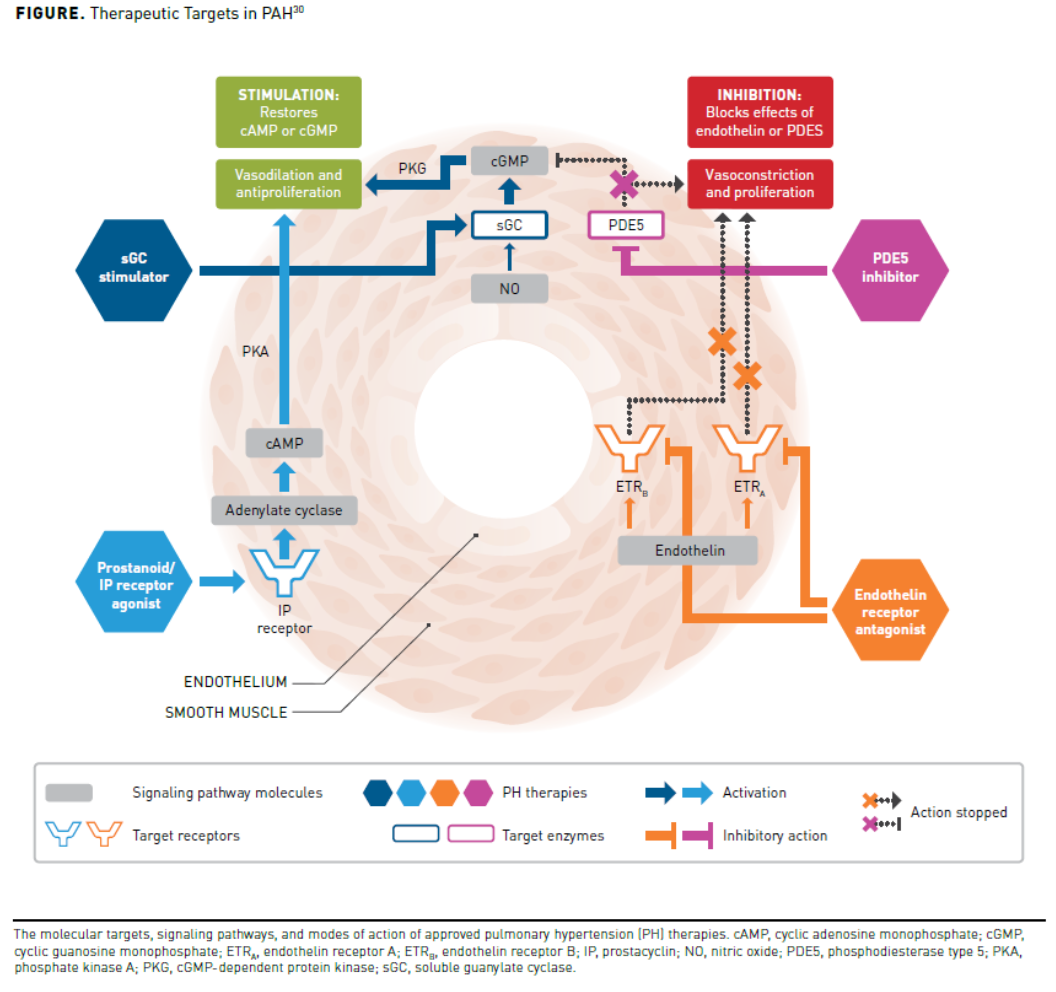
The triggering etiology that initiates the pathogenesis of PAH is likely multifactorial, including inappropriate angiogenesis, metabolic derangements, DNA damage, genetic mutations, and impaired vasoreactivity.3 Endothelial cell injury along with impaired vascular regeneration, abnormal vascular remodeling, and loss of the small pulmonary arteries are all known to occur as part of the PAH pathogenesis.27,28 Once endothelial dysfunction occurs, progressive vascular remodeling of the distal pulmonary arteries ensues, causing significant proliferation and resistance to apoptosis of pulmonary artery resident cells.3 As a result, pulmonary vascular lumen occlusion occurs, leading to increased pulmonary vascular resistance (PVR) and mPAP.3,29 The abnormal PVR and mPAP lead to right ventricle dilation and dysfunction, which can ultimately lead to a decreased cardiac output (CO). Additionally, an imbalance exists between vasodilation and vasoconstriction favoring vasoconstriction with an increase in circulating vasoconstrictors (ie, thromboxane, endothelin, and serotonin) and a decrease in circulating vasodilators (ie, prostacyclin, nitric oxide [NO], and vasoactive intestinal polypeptide).5 The improved understanding of the pathophysiology of PAH has led to development of therapies targeting the NO pathway, prostacyclin pathway, and endothelin pathway (Figure30).The pathology of PAH had previously been thought to be limited to the small pulmonary arteries; however, recent evidence suggests that systemic vascular manifestations also occur.31 For example, patients with PAH exhibit impaired brachial artery flow-mediated dilation, abnormal cerebral blood flow, skeletal myopathy, and intrinsic kidney disease. Although some of these manifestations can be explained as a consequence of right ventricular dysfunction, Nickel et al argue that there is also evidence to support a mechanistic link with PAH pathophysiology. More research is needed to fully understand the systemic effects of PAH.31 Tragically, as the disease progresses,thecompensatory mechanisms of the right heart can fail, and lead to premature death.3 Autoantibodies, proinflammatory cytokines, and inflammatory infiltrates have also been implicated in the pathogenesis of PAH. Individuals with PAH have increased von Willebrand factor levels, plasma fibrinopeptide A, plasminogen activator inhibitor-1, serotonin (5-HT), and thromboxane.32 In addition, tissue plasminogen activator, thrombomodulin, NO, and PGI2 are decreased, creating an imbalance that favors thrombosis.32
Genetics
Over the past 20 years, there have been significant advancements in the understanding of the genetics of PAH.33,34 Approximately 6% to 10% of persons with PAH have a family history.35 Those who were previously identified as having idiopathic sporadic PAH are now known to have a genetic cause and would fall into the heritable PAH group instead. The most well-known genetic mutation associated with PAH is the bone morphongenetic protein receptor 2 (BMPR2) mutation. Seventy percent to 80% of patients with heritable PAH and 10% to 20% of individuals with idiopathic PAH have the BMPR2 mutation.35 Presence of this genetic mutation markedly increases the risk of developing heritable PAH and guidelines recommend genetic counseling for families and patients.36-38 Additional mutations that are implicated in PAH development involve ligands of BMPR2 and include GDF2 (encoding BMP9), type I receptor (ACVRL1), and SMAD9 (encoding Smad8). Potassium channel subfamily K member 3 (KCNK3) mutations and caveloin-1 (CAV1) mutations have also been identified along with many others.5 Interestingly, PAH mutations are autosomal dominant with low penetrance. As a result, some patients may never exhibit disease, further supporting the assertion that the trigger of disease is multifactorial.1
Mitochondrial metabolism impairments have also been associated with development of PAH.36 The female preponderance in PAH may be explained by the link between sex hormone metabolism differences and right ventricular function.36 More research is needed to elucidate this theory entirely. BMPR2 mutation penetrance also varies significantly, 14% of men and 42% of women, further suggesting that sex hormones and their metabolism may be associated with the pathogenesis of PAH.1
Clinical Presentation and Diagnosis
A thorough history, physical examination, and complete workup is imperative to determine if a patient truly has PAH. The first presenting symptoms include exertional dyspnea, fatigue, and weakness.7,39,40 As the disease progresses, dyspnea may occur at rest, and other symptoms such as chest pain, presyncope, syncope, lower extremity edema, jugular venous distension, and abdominal bloating and distension may occur.7 Less common symptoms include cough, hemoptysis, and hoarseness. The assessment of symptoms includes placing the patient in a World Health Organization functional class (WHO-FC) based on level of impairment in physical activity. Patients in WHO-FC I have no limitation of physical activity; WHO-FC II is characterized by slight limitation in physical activity with ordinary activity causing undue dyspnea, fatigue, chest pain, or near syncope; WHO-FC III is characterized by marked limitation of physical activity with no discomfort at rest but less than ordinary physical activity causing undue dyspnea, fatigue, chest pain, or near syncope; finally, WHO-FC IV is characterized by an inability to perform any physical activity without symptoms with signs of right ventriculat failure and symptoms at rest with discomfort increasing by any physical activity. In addition to a thorough history and physical examination, initial tests such as chest radiography and electrocardiography should be done. If findings from the workup or clinical findings suggest the presence of PH and right ventricular dysfunction, a 2-dimensional transthoracic echocardiography (TTE) with doppler should be employed as an initial screening measure. TTE is the best test to screen for possible PH and PAH, but only a right heart catheterization (RHC) can assess the pulmonary hemodynamics needed to diagnose PH and PAH. The RHC is required to assess the mPAP, PVR, and CO. It is the gold standard and used to confirm a diagnosis of PH.7,40
Historically, PAH has been defined by an mPAP of greater than or equal to 25 mm Hg at rest plus a pulmonary wedge pressure (WP) less than or equal to 15 mm Hg, and PVR greater than or equal to 3 Wood units (WU) using RHC.41 However, at the 6th WSPH, the expert task force recommended to lower the hemodynamic definition for the first time since the inception of the WSPH in 1973 based on accumulated evidence suggesting a normal resting mPAP of 14 ± 3.3 mm Hg and that the upper limit of normal (or 2 standard deviations) for mPAP is greater than 20 mm Hg.1,42 The change in hemodynamic criteria was primarily driven by increasing evidence suggesting that those who fall within the 20 to 24 mm Hg mPAP range exhibited poorer outcomes and tended to progress to overt PH (especially those with systemic sclerosis, chronic thromboembolic pulmonary hypertension, and family history of PAH-causing genes) more often than those with an mPAP less than or equal to 20 mm Hg.43-47 The change in hemodynamic criteria has not occurred without opposition by some experts who argue that the 2 standard deviation argument is not consistent because pulmonary arterial WP and PVR cutoff values do not follow the same criteria. They suggest that the new hemodynamic criteria could create yet another cohort of individuals who could be “missed” by the previous and current cutoffs.48 Still, the evidence is clear that an mPAP greater than 20 mm Hg is considered above normal, and more research is required in patient cohorts to further elucidate the relationship between clinical presentation and long-term outcomes.1
Risk Stratification
PAH treatment is based on the severity of disease at diagnosis and assessing how the individual will respond to treatment using multiple factors to stratify risk based on predicted mortality.1 Other treatment considerations include patient/clinician preference, drug interactions, tolerability, and potential adverse effects.49 Several risk stratification tools (RSTs) have been developed using retrospective analysis of large patient registries to aid in determining prognosis and guiding therapy for patients with PAH (Table 349). The RSTs use multiple data points such as demographics, functional status, laboratory values, and hemodynamic information to stratify patients into low, intermediate, or high risk. The categories are then used as a baseline for initiating treatment, determining prognosis, and monitoring response and disease progression long term.1,48
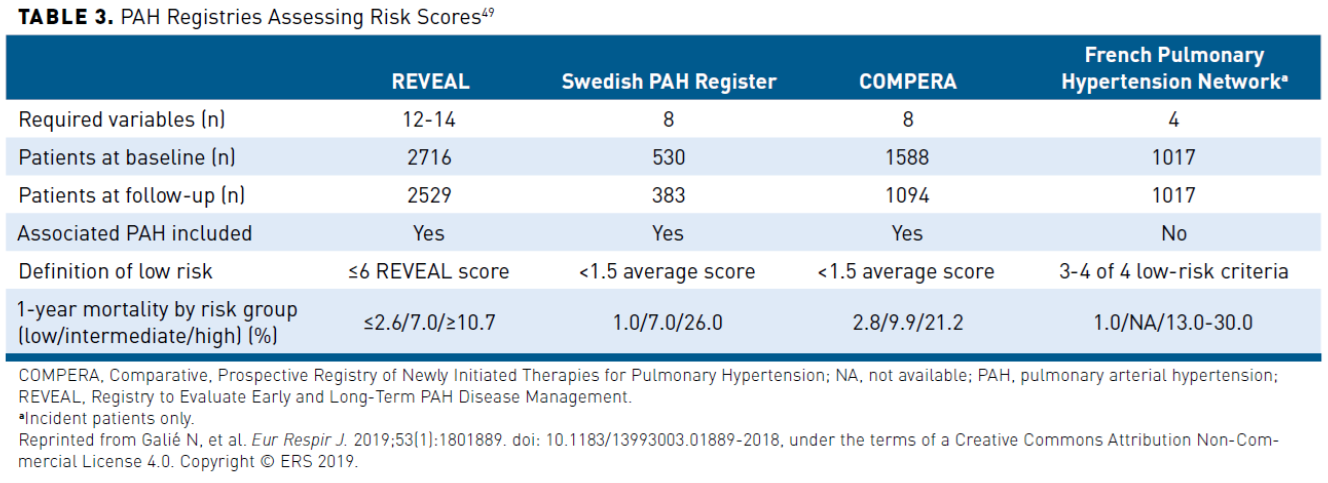
The REVEAL RST consists of 12 to 14 variables used to determine the risk of 1-year mortality. The RST has been validated for predicting survival at baseline, 1-year follow-up, and at 5 years.19,48,50,51 The most recent REVEAL 2.0 calculator can also predict clinical worsening and mortality among those who have survived PAH for a minimum of 1 year from their initial enrollment by including hospitalizations in the past 6 months and estimated glomerular filtration rate.1,48
Another RST, COMPERA, was developed by a European group and uses fewer data points than REVEAL but classifies individuals similarly. The 2015 European Society of Cardiology (ESC)/European Respiratory Society (ERS) PH guidelines RST uses a multidimensional approach that focuses on the most frequent determinants of prognosis.39 All of the variables do not have to be assessed at each visit, but should include FC determination and at least one exercise capacity measurement (eg, 6-minute walking distance). It is also recommended to assess RV function by measuring brain natriuretic peptide (BNP)/N-terminal pro-brain BNP (NT-proBNP) or by echocardiography. Patients are then stratified into low, intermediate, and high risk based on determinants assessed. The RST can assist in guiding therapeutic decisions; however, application to individual patients should be done with care. A comprehensive assessment that also includes other risk factors such as signs of right heart failure, syncope, and comorbidities should be included to optimize clinical decision making.39
The Swedish PAH Register and the French Pulmonary Hypertension Network have also developed RSTs from large registries. Regardless of which RST is used, all have similar efficacy in identifying individuals at high risk. It is important to note that the tools utilize retrospective data and have some limitations, including measurement of nonmodifiable risk factors and inclusion of data points that are not routinely collected in PAH. Thus, despite which tool is selected, RSTs can help clinicians determine which individuals with PAH are at high risk for 1-year mortality, prioritization of therapies, and referral for transplant.48
Quality of Life
The impact of PAH disease symptoms on a person’s functional mobility and psychosocial state adversely affects health-related quality of life (HRQOL).52 Although there have been significant advancements in the understanding of PAH and targeted therapies that have decreased mortality, these improvements have not necessarily been paralleled from the perspective of individuals with PAH.1 PAH affects all parts of a person’s daily life that influence their HRQOL, including physical activity, well-being, and emotional and social functioning.52 The debilitation level experienced by patients is considered at least as severe as chronic obstructive pulmonary disease and renal failure.52
A report from the European Pulmonary Hypertension Association (PHA Europe) found that 83% (n = 326) of people with PAH surveyed reported difficulty climbing stairs, and 97% stated PAH affected their ability to participate in sports and exercise to some degree.52 Similarly, the FDA Patient Voice survey (≈85 participants) reported that breathlessness and fatigue were also restrictive on daily physical activities. Both surveys also found that reduced physical activity had negative implications for long-term outcomes among persons with PAH.52
PAH also has considerable psychological effects, such as feelings of social isolation, lack of understanding or knowledge about the disease in the community (not a “visible” disease), and friends and family.53 A study also found that 48% of individuals with PAH experienced mild to extremely severe symptoms of anxiety, 32.6% had symptoms of depression, and 27.6% had symptoms of stress.54 As the psychological impact of PAH is often underrecognized, it is vital to assess patients during all encounters, especially if and when functional class worsens.
In addition, patients with PAH are also frequently affected by a loss of household income due to loss of work or inability to remain working.53 A European PHA survey found that 73% of patients who had to give up work or needed assistance to maintain employment had a loss in average household income. Moreover, 1 in 6 reported their income decreasing by half. Also, 35% of caregivers reported a reduction in income to care for the individual with PAH.53
Age has contributed to the burden of patients with PAH.55 The prevalence of PAH is increasing among people aged 50 to 65 years who are more likely to be diagnosed with advanced stages of disease, and have lower exercise capacity and a higher number of comorbidities. Multiple comorbidities are associated with a delay in diagnosis among older patients and could explain the challenge of disease recognition in earlier years among this patient population.55 Women of childbearing age are also at increased risk of complications during pregnancy due to poor tolerance of hemodynamic and physiologic changes that can cause right ventricular failure and arrhythmias.56 Due to a significantly higher associated mortality rate, it is recommended that women with PAH avoid pregnancy.39
Multiple factors contribute to an individual’s perception of their overall well-being. Therefore, the WSPH expert task force recommends that management of individuals with PH should occur at specialized care centers with a patient-centered multidisciplinary team that focuses on quality of life, shared clinical decision making, and access to palliative care. Although numerous studies have demonstrated that PH treatments improve HRQOL, it is important to recognize that HRQOL is one component and may not capture the depth and complexity of psychosocial issues experienced by patients and caregivers. In other words, both individual and patient population-level perspectives should be considered.1 Several patient-reported outcome (PRO) instruments have been developed to evaluate the effect of PAH therapies on patient symptoms and the impact of the symptoms on patients’ lives and use of these are recommended to be incorporated as secondary end points in clinical trials. Two of these instruments are the psychometric validation of the pulmonary arterial hypertension-symptoms and impact (PAH-SYMPACT) questionnaire and the emphasis-10 questionnaire.57,58
The WSPH task force encourages clinicians to participate in narrative medicine where individuals with PAH can express their concerns and challenges related to their individual health.1 Patients with PAH also need improved access to palliative care, as they may experience low HRQOL and high disease burden.59 Concerning the population level, continued support for patient groups and associations, patient education, and public awareness are needed.1 The interdisciplinary healthcare team can help patients navigate intolerable adverse effects and make recommendations for treatment adjustments and avoidance of drug interactions as required to optimize therapy and treatment acceptance and/or adherence.
Conclusions
PAH is a devastating life-limiting progressive disorder. Over the past 20 years, significant advancements have occurred due to an improved understanding of PAH pathogenesis and specific therapies that help decrease mortality. As more evidence has accumulated, changes to the evaluation and management of PAH have occurred. Contemporary registries continue to provide crucial information to help risk-stratify patients, determine prognosis, and monitor and manage therapeutic goals. Patients with PAH experience significant effects on their HRQOL, which is correlated to their functional, emotional, work, and social abilities. Healthcare providers should assess a patient’s HRQOL during each encounter to improve patient satisfaction. Furthermore, as the factors that affect individual HRQOL are multifactorial, it is important that patients are involved in the clinical decision-making process. A multidisciplinary approach with multiple layers of support should be available to all patients, and importantly, they must be aware of the existence of such services.
Author affiliation: Deborah Jo Levine, MD, FCCP, is professor of medicine, pulmonary and critical care, and director of pulmonary hypertension, University of Texas Health, San Antonio, TX.
Funding source: This activity is supported by an educational grant from United Therapeutics Corporation.
Author disclosure: Dr Levine has no relevant financial relationships with commercial interests to disclose.
Authorship information: Substantial contributions to concept and design; drafting of the manuscript; and critical revision of the manuscript for important intellectual content.
Address correspondence to: levinedj@uthscsa.edu
Medical writing and editorial support: Brittany Hoffmann-Eubanks, PharmD, MBA
REFERENCES
1. Beshay S, Sahay S, Humbert M. Evaluation and management of pulmonary arterial hypertension. Respir Med. 2020;171:106099. doi: 10.1016/j.rmed.2020.106099
2. Simonneau G, Gatzoulis MA, Adatia I, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2013;62(25 suppl):D34-D41. doi: 10.1016/j.jacc.2013.10.029
3. Bourgeois A, Omura J, Habbout K, et al. Pulmonary arterial hypertension: new pathophysiological insights and emerging therapeutic targets. Int J Biochem Cell Biol. 2018;104:9-13. doi: 10.1016/j.biocel.2018.08.015
4. Klinger JR, Elliott CG, Levine DJ, et al. Therapy for pulmonary arterial hypertension in adults: update of the CHEST Guideline and Expert Panel Report [Erratum appears in Chest. 2021;159(1):457]. Chest. 2019;155(3):565-586. doi: 10.1016/j.chest.2018.11.030
5. Prins KW, Thenappan T. World Health Organization group I pulmonary hypertension: epidemiology and pathophysiology. Cardiol Clin. 2016;34(3):363-374. doi: 10.1016/j.ccl.2016.04.001
6. Simonneau G, Montani D, Celermajer DS, et al. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur Respir J. 2019;53(1):1801913. doi: 10.1183/13993003.01913-2018
7. McLaughlin VV, Shah SJ, Souza R, Humbert M. Management of pulmonary arterial hypertension. J Am Coll Cardiol. 2015;65(18):1976-1997. doi: 10.1016/j.jacc.2015.03.540
8. Zamanian RT, Hedlin H, Greuenwald P, et al. Features and outcomes of methamphetamine-
associated pulmonary arterial hypertension. Am J Respir Crit Care Med. 2018;197(6):788-800.
doi: 10.1164/rccm.201705-0943OC
9. Hickey PM, Thompson AA, Charalampopoulos A, et al. Bosutinib therapy resulting in severe deterioration of pre-existing pulmonary arterial hypertension. Eur Respir J. 2016;48(5):1514-1516. doi: 10.1183/13993003.01004-2016
10. Renard S, Borentain P, Salaun E, et al. Severe pulmonary arterial hypertension in patients treated for hepatitis C with sofosbuvir. Chest. 2016;149(3):e69-e73. doi: 10.1016/j.chest.2015.09.018
11. Riou M, Seferian A, Savale L, et al. Deterioration of pulmonary hypertension and pleural effusion with bosutinib following dasatinib lung toxicity. Eur Respir J. 2016;48(5):1517-1519. doi: 10.1183/13993003.01410-2016
12. Seegobin K, Babbar A, Ferreira J, Lyons B, Cury J, Seeram V.. A case of worsening pulmonary arterial hypertension and pleural effusions by bosutinib after prior treatment with dasatinib. Pulm Circ. 2017;7(4):808-812. doi: 10.1177/2045893217733444
13. Alvarez PA, Saad AK, Flagel S, Mazzocchi O, Blanco MV. Leflunomide-induced pulmonary hypertension in a young woman with rheumatoid arthritis: a case report. Cardiovasc Toxicol. 2012;12(2):180-183. doi: 10.1007/s12012-012-9153-3
14. Coirier V, Lescoat A, Chabanne C, et al. Pulmonary arterial hypertension in four patients treated by leflunomide. Joint Bone Spine. 2018;85(6):761-763. doi: 10.1016/j.jbspin.2017.12.014
15. Savale L, Chaumais MC, Montani D, et al. Direct-acting antiviral medications for hepatitis C virus infection and pulmonary arterial hypertension. Chest. 2016;150(1):256-258. doi: 10.1016/j.chest.2016.04.031
16. Mandel J, Mark EJ, Hales CA. Pulmonary veno-occlusive disease. Am J Respir Crit Care Med. 2000;162(5):1964-1973. doi: 10.1164/ajrccm.162.5.9912045
17. Rich S, Kaufmann E, Levy PS. The effect of high doses of calcium-channel blockers on survival in primary pulmonary hypertension. N Engl J Med. 1992;327(2):76-81. doi: 10.1056/nejm199207093270203
18. Rich S, Dantzker DR, Ayres SM, et al. Primary pulmonary hypertension. A national prospective study. Ann Intern Med. 1987;107(2):216-223. doi: 10.7326/0003-4819-107-2-216
19. Benza RL, Miller DP, Barst RJ, Badesch DB, Frost AE, McGoon MD. An evaluation of long-term survival from time of diagnosis in pulmonary arterial hypertension from the REVEAL Registry. Chest. 2012;142(2):448-456. doi: 10.1378/chest.11-1460
20. Humbert M, Sitbon O, Chaouat A, et al. Survival in patients with idiopathic, familial, and anorexigen-associated pulmonary arterial hypertension in the modern management era. Circulation. 2010;122(2):156-163. doi: 10.1161/circulationaha.109.911818
21. Benza RL, Gomberg-Maitland M, Miller DP, et al. The REVEAL Registry risk score calculator in patients newly diagnosed with pulmonary arterial hypertension. Chest. 2012;141(2):354-362. doi: 10.1378/chest.11-0676
22. McGoon MD, Miller DP. REVEAL: A contemporary US pulmonary arterial hypertension registry. Eur Respir Rev. 2012;21(123):8-18. doi: 10.1183/09059180.00008211
23. McGoon MD, Krichman A, Farber HW, et al. Design of the REVEAL registry for US patients with pulmonary arterial hypertension. Mayo Clin Proc. 2008;83(8):923-931. doi: 10.4065/83.8.923
24. Frost AE, Badesch DB, Barst RJ, et al. The changing picture of patients with pulmonary arterial hypertension in the United States: how REVEAL differs from historic and non-US contemporary registries. Chest. 2011;139(1):128-137. doi: 10.1378/chest.10-0075
25. Badesch DB, Raskob GE, Elliott CG, et al. Pulmonary arterial hypertension: baseline characteristics from the REVEAL Registry. Chest. 2010;137(2):376-387. doi: 10.1378/chest.09-1140
26. Benza RL, Miller DP, Gomberg-Maitland M, et al. Predicting survival in pulmonary arterial hypertension: insights from the Registry to Evaluate Early and Long-Term Pulmonary Arterial Hypertension Disease Management (REVEAL). Circulation. 2010;122(2):164-172. doi: 10.1161/circulationaha.109.898122
27. Ranchoux B, Harvey LD, Ayon RJ, et al. Endothelial dysfunction in pulmonary arterial hypertension: an evolving landscape (2017 Grover Conference Series). Pulm Circ. 2018;8(1):2045893217752912. doi: 10.1177/2045893217752912
28. Yuan JX, Rubin LJ. Pathogenesis of pulmonary arterial hypertension: the need for multiple hits. Circulation. 2005;111(5):534-538. doi: 10.1161/01.CIR.0000156326.48823.55
29. Humbert M, Guignabert C, Bonnet S, et al. Pathology and pathobiology of pulmonary hypertension: state of the art and research perspectives. Eur Respir J. 2019;53(1):1801887. doi: 10.1183/13993003.01887-2018
30. Humbert M, Ghofrani HA. The molecular targets of approved treatments for pulmonary arterial hypertension. Thorax. 2016;71(1):73-83. doi: 10.1136/thoraxjnl-2015-207170
31. Nickel NP, Yuan K, Dorfmuller P, et al. Beyond the lungs: systemic manifestations of pulmonary arterial hypertension. Am J Respir Crit Care Med. 2020;201(2):148-157. doi: 10.1164/rccm.201903-0656CI
32. Schermuly RT, Ghofrani HA, Wilkins MR, Grimminger F. Mechanisms of disease: pulmonary arterial hypertension. Nat Rev Cardiol. 2011;8(8):443-455. doi: 10.1038/nrcardio.2011.87
33. Deng Z, Morse JH, Slager SL, et al. Familial primary pulmonary hypertension (gene PPH1) is caused by mutations in the bone morphogenetic protein receptor-II gene. Am J Hum Genet. 2000;67(3):737-744. doi: 10.1086/303059
34. Lane KB, Machado RD, Pauciulo MW, et al; International PPH Consortium. Heterozygous germline mutations in BMPR2, encoding a TGF-beta receptor, cause familial primary pulmonary hypertension. Nat Genet. 2000;26(1):81-84. doi: 10.1038/79226
35. Morrell NW, Aldred MA, Chung WK, et al. Genetics and genomics of pulmonary arterial hypertension. Eur Respir J. 2019;53:1801899. doi: 1183/13993003.0189-2018
36. Evans JD, Girerd B, Montani D, et al. BMPR2 mutations and survival in pulmonary arterial hypertension: an individual participant data meta-analysis. Lancet Respir Med. 2016;4(2):129-137. doi: 10.1016/S2213-2600(15)00544-5
37. Loyd JE, Primm RK, Newman JH. Familial primary pulmonary hypertension: clinical patterns. Am Rev Respir Dis. 1984;129(1):194-197. doi: 10.1164/arrd.1984.129.1.194
38. Galiè N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Rev Esp Cardiol (Engl Ed). 2016;69(2):177. doi: 10.1016/j.rec.2016.01.002
39. Galiè N, Humbert M, Vachiery JL, et al; ESC Scientific Document Group. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension: the Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J. 2016;37(1):67-119. doi: 10.1093/eurheartj/ehv317
40. Frost A, Badesch D, Gibbs JS, et al. Diagnosis of pulmonary hypertension. Eur Respir J. 2019;53(1):1801904. doi: 10.1183/13993003.01904-2018
41. Condon DF, Nickel NP, Anderson R, Mirza S, de Jesus Perez VA. The 6th World Symposium on Pulmonary Hypertension: what’s old is new. F1000Res. 2019;8:F1000. doi: 10.12688/f1000research.18811.1
42. Kovacs G, Berghold A, Scheidl S, Olschewski H. Pulmonary arterial pressure during rest and exercise in healthy subjects: a systematic review. Eur Respir J. 2009;34(4):888-894. doi: 10.1183/09031936.00145608
43. Maron BA, Hess E, Maddox TM, et al.Association of borderline pulmonary hypertension with mortality and hospitalization in a large patient cohort: insights from the Veterans Affairs clinical assessment, reporting, and tracking program. Circulation. 2016;133(13):1240-1248. doi: 10.1161/CIRCULATIONAHA.115.020207
44. Assad TR, Maron BA, Robbins IM, et al. Prognostic effect and longitudinal hemodynamic
assessment of borderline pulmonary hypertension. JAMA Cardiol. 2017;2(12):1361-1368.
doi: 10.1001/jamacardio.2017.3882
45. Douschan P, Kovacs G, Avian A, et al. Mild elevation of pulmonary arterial pressure as a predictor of mortality. Am J Respir Crit Care Med. 2018;197(4):509-516. doi: 10.1164/rccm.201706-1215OC
46. Valerio CJ, Schreiber BE, Handler CE, Denton CP, Coghlan JG. Borderline mean pulmonary artery pressure in patients with systemic sclerosis: transpulmonary gradient predicts risk of developing pulmonary hypertension. Arthritis Rheum. 2013;65(4):1074-1084. doi: 10.1002/art.37838
47. Coghlan JG, Wolf M, Distler O, et al. Incidence of pulmonary hypertension and determining factors in patients with systemic sclerosis. Eur Respir J. 2018;51(4):1701197. doi: 10.1183/13993003.01197-2017
48. Thomas CA, Anderson RJ, Condon DF, de Jesus Perez VA. Diagnosis and management of pulmonary hypertension in the modern era: insights from the 6th World Symposium. Pulm Ther. 2020;6(1):9-22. doi: 10.1007/s41030-019-00105-5
49. Galiè N, Channick RN, Frantz RP, et al. Risk stratification and medical therapy of pulmonary arterial hypertension. Eur Respir J. 2019;53(1):1801889. doi: 10.1183/13993003.01889-2018
50. Benza RL, Miller DP, Foreman AJ, et al. Prognostic implications of serial risk score assessments in patients with pulmonary arterial hypertension: a Registry to Evaluate Early and Long-Term Pulmonary Arterial Hypertension Disease Management (REVEAL) analysis. J Heart Lung Transplant. 2015;34(3):356-361. doi: 10.1016/j.healun.2014.09.016
51. Farber HW, Miller DP, Poms AD, et al. Five-year outcomes of patients enrolled in the REVEAL Registry. Chest. 2015;148(4):1043-1054. doi: 10.1378/chest.15-0300
52. Delcroix M, Howard L. Pulmonary arterial hypertension: the burden of disease and impact on quality of life. Eur Respir Rev. 2015;24(138):621-629. doi: 10.1183/16000617.0063-2015
53. European Pulmonary Hypertension Association. The impact of pulmonary arterial hypertension (PAH) on the lives of patients and carers: results from an international survey. Published September 2012. Accessed January 8, 2021. phaeurope.org/wp-content/uploads/PAH_Survey_FINAL.pdf
54. M M Vanhoof J, Delcroix M, Vandevelde E, et al. Emotional symptoms and quality of life in patients with pulmonary arterial hypertension. J Heart Lung Transplant. 2014;33(8):800-808. doi: 10.1016/j.healun.2014.04.003
55. Hoeper MM, Gibbs JS. The changing landscape of pulmonary arterial hypertension and implications for patient care. Eur Respir Rev. 2014;23(134):450-457. doi: 10.1183/09059180.00007814
56. Tabarsi N, Levy R, Rychel V, et al. Pregnancy among women with pulmonary arterial hypertension: a changing landscape? Int J Cardiol. 2014;177(2):490-491. doi: 10.1016/j.ijcard.2014.08.059
57. Chin KM, Gomberg-Maitland M, Channick RN, et al. Psychometric validation of the Pulmonary Arterial Hypertension-Symptoms and Impact (PAH-SYMPACT) Questionnaire: results of the SYMPHONY trial. Chest. 2018;154(4):848-861. doi: 10.1016/j.chest.2018.04.027
58. Yorke J, Corris P, Gaine S, et al. emPHasis-10: development of a health-related quality of life measure in pulmonary hypertension. Eur Respir J. 2014;43(4):1106-1113. doi: 10.1183/09031936.00127113
59. Swetz KM, Shanafelt TD, Drozdowicz LB, et al. Symptom burden, quality of life, and attitudes toward palliative care in patients with pulmonary arterial hypertension: results from a cross-sectional patient survey. J Heart Lung Transplant. 2012;31(10):1102-1108. doi: 10.1016/j.healun.2012.08.010
