- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Psoriasis Associated with Being Overweight, Obesity, Study Finds
In a new study, patients with psoriasis had a 39.46% prevalence of being overweight and 37.41% prevalence of obesity—83.56% patients also dismissed the importance of having healthy balanced eating habits.
This article was originally published in HCPLive® and has been lightly edited.
Psoriasis’ association with being overweight and obese puts a health burden on patients and affects the disease course and safety, according to a new study.1
Psoriasis, a common, chronic, inflammatory skin disease, is known to lead to many comorbid disorders, such as obesity, hypertension, diabetes, metabolic syndrome, cardiovascular disease, and depression. Epidemiological studies repeatedly demonstrated a strong, bidirectional relationship between psoriasis and obesity. Both psoriasis and obesity worsen the severity and progression of the other.
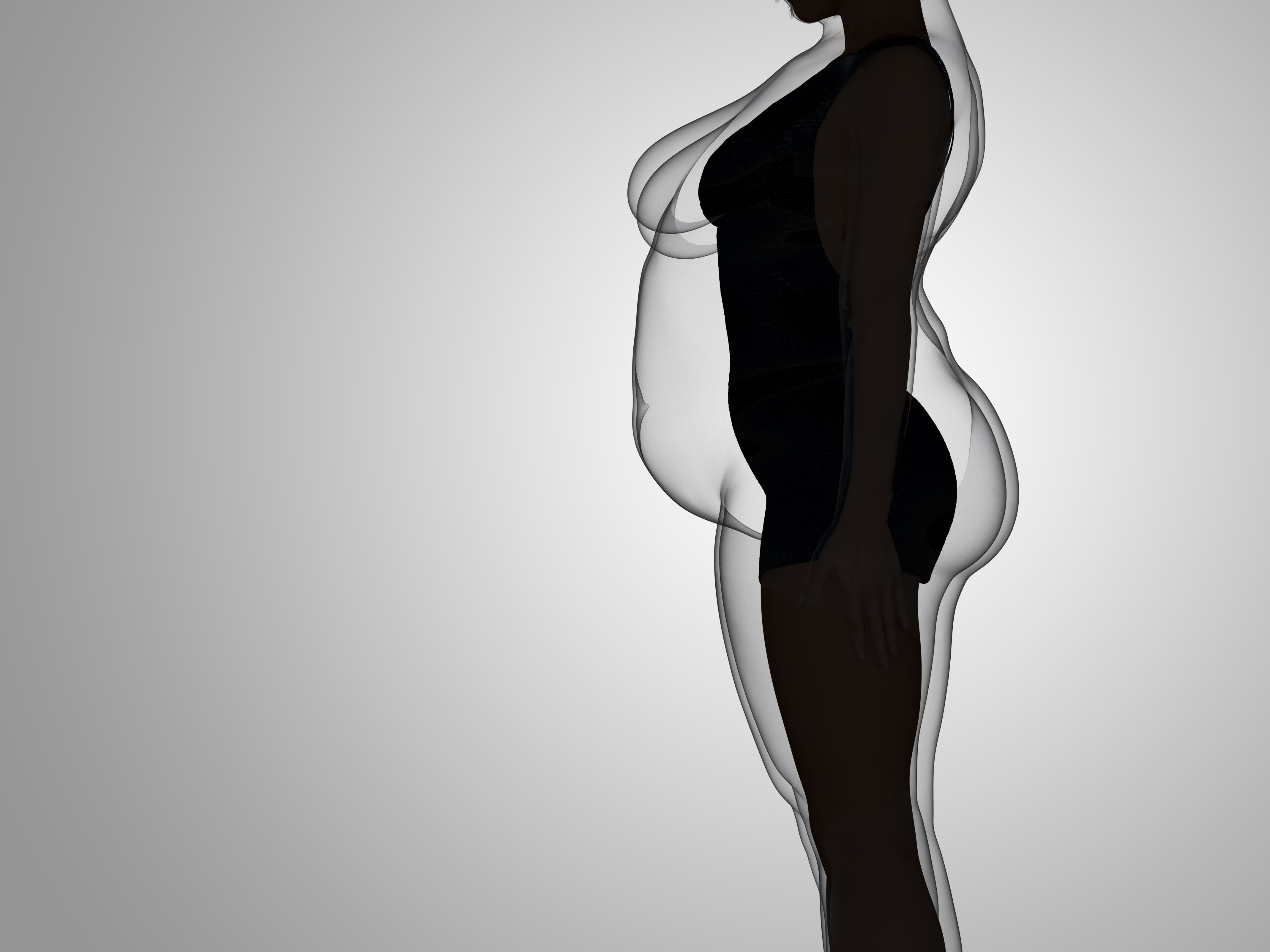
Obesity Concept | image credit: high_resolution - stock.adobe.com
According to a 2018 study, losing weight through diet and exercise can decrease the severity and size of psoriasis patches—and can make psoriasis medications more effective. Though, it remains unknown whether weight loss can prevent psoriasis.2
A new observational study, led by Anna Czarnecka, MD, from the department of dermatology, venerology, and allergology at Medical University of Gdansk, sought to evaluate the issue of overweight and obesity among psoriasis patients in terms of prevalence and influence on the disease course. The study was conducted between 2021 and 2023, including a participant sample of 147 adults with chronic plaque psoriasis. The age range was from 18 – 83 years, and 29.25% were female (n = 43).1
“Our study provided relevant evidence that overweightness and obesity constitute a major health burden among psoriatic patients by influencing the disease course and severity,” investigators wrote. “Enhanced understanding of the phenomenon may directly translate into improving disease management and overall patient care.”
The investigators collected data on psoriasis onset, clinical manifestations of psoriasis, lifestyle factors (including diet and smoking), presence of psoriatic arthritis, the severity of psoriasis (defined by the psoriasis area and severity index and the body surface area), the impact of psoriasis on the quality of life (evaluated using dermatological life quality index), and anthropometric measurements such as height and body weight. Body weight was calculated by formalized criteria: < 18.5 kg/m2 (underweight), 18.5 to 24.9 kg/m2 (normal weight), 25.0 to 29.9 kg/m2 (overweight), and > 30.0 kg/m2 (obesity).
Psoriasis type 1 included participants who had an onset < 40 years old, and psoriasis type II had an onset > 40 years old. The psoriasis area and severity index were scaled as followed: < 10 points (mild), 10 to 15 points (moderate), and > 15 points (severe). The body surface area scores were 0 to 1 points (no effect), 2 to 5 points (small effect), 6 to 10 points (moderate effect), 11 to 20 points (very large effect), and 21 to 30 points (extremely large effect).
Most (83.56%) of psoriatic patients said they disregarded the importance of having a balanced and nutritious diet. Also, 55.78% reported being past or current smokers—which was more prevalent for women (62.50%) than men (39.53%).
“Our findings revealed a noteworthy shift in smoking habits, with the majority of women (62.50%) having a history of past or current smoking,” the investigators wrote. “This trend could be indicative of changing societal norms and the impact of public health campaigns, which have historically been primarily directed towards men.”
For overweight and obese patients, 77% had psoriasis nail involvement and 77.77% had psoriatic arthritis. Psoriasis nail involvement and psoriatic arthritis were more common than for people who had a normal weight.
“It is possible that nail psoriasis might be indirectly linked to obesity, due to the elevated prevalence of psoriatic arthritis, a condition associated with both comorbidities,” the investigators wrote. “An elevated BMI index is linked to an increased susceptibility to psoriatic arthritis and its early onset.”
In a correlation analysis between the BMI and the psoriasis area and severity index for psoriatic patients, a normal weight had a BMI < 25 (n = 34); P = .917997 and an abnormal weight had a BMI of > 25 (n = 112); P = .016.
The investigators found patients with psoriasis had a 39.46% prevalence of overweight and 37.41% prevalence of obesity, demonstrating a “strong predisposition of psoriatic patients for abnormal body mass.”
“The association is strong, especially in the context of obesity, when compared to the latest reports on the prevalences of overweightness and obesity among the general population of Poland,” the investigators wrote.
Meanwhile, in a correlation analysis between the BMI and the dermatological quality of life index for psoriatic patients, a normal weight had a BMI of < 25 (n = 34); P = .075070 and an abnormal weight had a BMI of > 25 (n = 112); P = .36.
“The decrease in functional ability associated with psoriatic arthritis leads to a reduction in physical activity, which in turn promotes weight gain and consecutive mechanical trauma to tissues,” the investigators wrote. “This underscores the importance of body mass prevention and early treatment among patients with psoriasis and psoriatic arthritis.”
References
- Czarnecka A, Zabłotna M, Purzycka-Bohdan D, Nowicki RJ, Szczerkowska-Dobosz A. An Observational Study of 147 Psoriasis Patients: Overweightness and Obesity as a Significant Clinical Factors Correlated with Psoriasis. Medicina. 2023; 59(11):2006. https://doi.org/10.3390/medicina59112006
- Askinazi, O. Is There a Link Between Psoriasis and Obesity? Healthline. June 16, 2022. https://www.healthline.com/health/psoriasis-and-obesity#1. Accessed November 21, 2023.
