- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
PROSPERO Identifies Key Risk Factors for Gallstones in Crohn Disease
The findings from the PROSPERO study reveal that multiple hospitalizations, long-term disease duration, prior surgeries, and factors like corticosteroid use and total parenteral nutrition significantly increase the risk of gallstone disease in patients with Crohn disease.
A history of multiple hospitalizations and long-term disease duration were identified as some of the biggest risk factors for gallstone disease in patients with Crohn disease, according to the PROSPERO study.1
The literature review, published in Digestive Diseases and Sciences, used data from 3 major databases through September 10, 2023, to pull together a comprehensive list that providers can identify in their patients with Crohn disease and prevent gallstone development and complications.
Although the 2 subtypes of inflammatory bowel disease are similar, Crohn disease occurs in the digestive tract, while ulcerative colitis manifests in the colon and rectum. | Image credit: Crystal light - stock.adobe.com
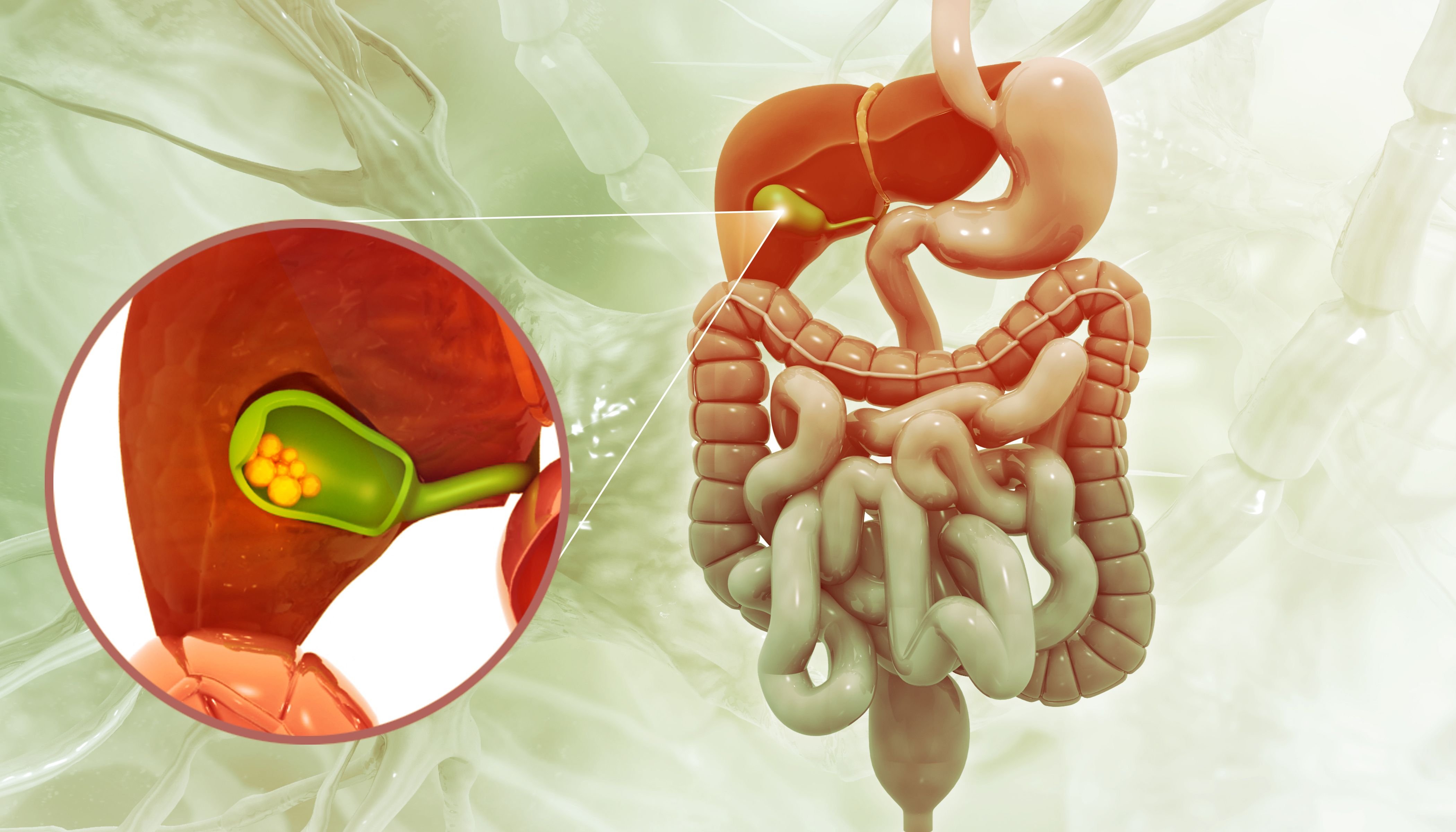
Crohn disease is a subtype of inflammatory bowel disease (IBD), along with ulcerative colitis.2 Although the 2 subtypes are similar, Crohn disease occurs in the digestive tract, while ulcerative colitis manifests in the colon and rectum.
One study found that the prevalence of IBD in Western regions ranges from 12 to 26 per 100,000 people and is expected to stay high, potentially reaching 1% in some areas by 2030.3 IBD can present with intestinal and extraintestinal manifestations, with gallstone disease having strong associations with Crohn disease.2 A review of cohort studies on gallstone disease prevalence found an annual incidence of 0.60% to 1.39% for the general population, which rose to 1.44% in those with Crohn disease.4
Past research has suggested that patients with Crohn disease may be at risk for gallstone disease due to factors like female sex, prior surgery, and total parenteral nutrition (TPN), but the findings have been inconsistent, and the underlying mechanism remains unclear, highlighting the need for a comprehensive meta-analysis.1
A systematic search of PubMed, Embase, and Web of Science identified studies on gallstone risk factors in patients with Crohn disease. Two independent reviewers screened and selected studies based on predefined eligibility criteria, extracting key data on prevalence, risk factors, and study characteristics. The quality assessment was conducted using the Newcastle–Ottawa Scale, with publication bias evaluated via funnel plots and Egger’s test. Researchers used the Review Manager and Stata to calculate odds ratios and weighted mean differences for the statistical analysis. Heterogeneity was assessed through Cochran’s chi-square test and the I² statistic, with sensitivity and subgroup analyses addressing variability.
A total of 11 studies were included in the meta-analysis, with gallstone disease prevalence in patients with Crohn disease ranging from 9.8% to 29.8%. A pooled prevalence of 14.9% was estimated, though high heterogeneity (I² = 92.3%) was observed. Stratified analyses revealed that prevalence varied based on gallstone definition (10.6% for existing gallstones vs 20% when including prior cholecystectomy) and study design (17.2% in cohort studies vs 10.6% in case-control studies).
The results found several factors influence the risk of gallstone disease among patients with Crohn disease:
- Age
- Hospitalizations
- Stenosis
- Disease location
- Ileocolic Crohn disease
- Lifetime Surgery
- Multiple Corticosteroid Treatments (≥ 3 times)
- Immunomodulator Therapy
- TPN History
- Multiple TPN Instances
A history of more than 2 hospitalizations was strongly associated with a higher risk (OR, 4.26; P < .00001), while having Crohn disease for more than 15 years also substantially elevated the likelihood of gallstone formation (OR, 3.01; P < .0001). Patients who had multiple instances of TPN experienced a further increased risk (OR, 2.93, P < .0003), and those with a history of TPN usage were also significantly affected (OR, 2.66, P < .008). A medication history of at least 3 corticosteroid treatments were linked with a notable rise in gallstone risk (OR, 2.65; P = .0006), and prior bowel resection surgeries significantly contributed to gallstone development (OR, 2.50; P < .00001).
Moderate risk factors included ileocecal Crohn disease, which increased the likelihood of gallstones (OR, 1.93; P = .01), and the use of immunomodulator therapy, which was also associated with a higher risk (OR, 1.94; P = .02). Additionally, patients with ileocolic Crohn disease (L3) had an elevated gallstone risk (OR, 1.38; P = .03).
In contrast, some factors showed minimal or no significant impact on gallstone disease. No meaningful differences were observed in gallstone prevalence between males and female patients (OR, 1.16; P = .43), and body mass index (whether overweight or low weight) did not significantly affect gallstone risk (OR, 1.39; P = .34). Furthermore, Crohn disease limited to the ileum (Ileocecal Crohn disease) was not considered a significant risk factor (OR, 0.89; P = .42). These findings highlighted the most influential contributors to gallstone development in Crohn disease patients, emphasizing the importance of monitoring high-risk individuals.
The study has several limitations, including potential biases due to its reliance on observational designs, which prevent establishing causal relationships, and publication bias affecting gallstone prevalence analysis. Most data were from Europe, with a lack of studies from Asia and Africa. Further multicenter studies are needed to address these issues and explore gallstone risk factors more comprehensively.
References
1. Risk factors for gallstones in Crohn’s disease: a systematic review and meta-analysis. Dig Dis Sci. 2024;69:4187-4202. doi:10.1007/s10620-024-08597-1
2. Crohn’s & ulcerative colitis: know the difference? WebMD. Updated April 12, 2023. Accessed February 3, 2025. https://www.webmd.com/ibd-crohns-disease/crohns-colitis-difference
3. Kaplan GG, Windsor JW. The four epidemiological stages in the global evolution of inflammatory bowel disease. Nat Rev Gastroenterol Hepatol. 2021;18:56-66. doi:10.1038/s41575-020-00360-x
4. Shabanzadeh DM. Incidence of gallstone disease and complications. Curr Opin Gastroenterol. 2018;34:81-89. doi:10.1097/MOG.0000000000000418
Corticosteroid Premedication for Infliximab Remains Unnecessarily Common
July 8th 2025Although use of corticosteroid premedication prior to infliximab infusions is declining, it remains unnecessarily high despite limited benefit and the risk of serious adverse events from corticosteroids.
Read More
