- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Profiles of COVID-19 Patients: A Study of Private Health Care Claims
Nationally and in every US census region, chronic kidney disease (CKD) and kidney failure were the most common comorbidity in hospitalized COVID-19 patients, accounting for 13% of all such patients in the period January-May 2020 (Figure 1). All regions except one resembled the nation in having type 2 diabetes as the second most common comorbidity; the exception, the South, had hypertension in that rank. These are among the findings of FAIR Health’s fourth COVID-19 study, Key Characteristics of COVID-19 Patients: Profiles Based on Analysis of Private Healthcare Claims.
FIGURE 1. Most Common Comorbidities of Patients Hospitalized for COVID-19, Nationally, January-May 2020
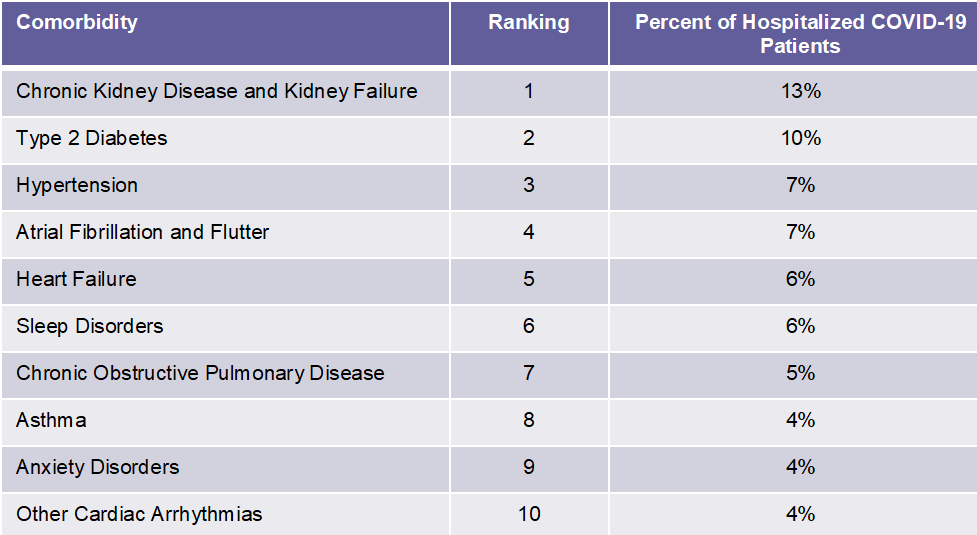
Source: FAIR Health
This study uses the nation’s largest repository of private healthcare claims to illuminate some of the key characteristics of patients diagnosed with COVID-19. These characteristics include age, gender, rural vs urban area by age, venue of care where first diagnosed, venue of care by age, comorbidities of hospitalized patients and median costs of hospitalization. The patient characteristics are analyzed nationally and also by US census region. The data studied are from the period January-May 2020.
Among the other findings:
Nationally, the median charge amount for hospitalization of a COVID-19 patient ranged from $34,662 for the 23-30 age group to $45,683 for the 51-60 age group (Figure 2). The median estimated in-network amounts ranged from $17,094 for people over 70 years of age to $24,012 for people aged 51-60 years.
FIGURE 2. Median COVID-19 Hospitalization Charge Amounts and Estimated Allowed Amounts by Age, Nationally, January-May 2020
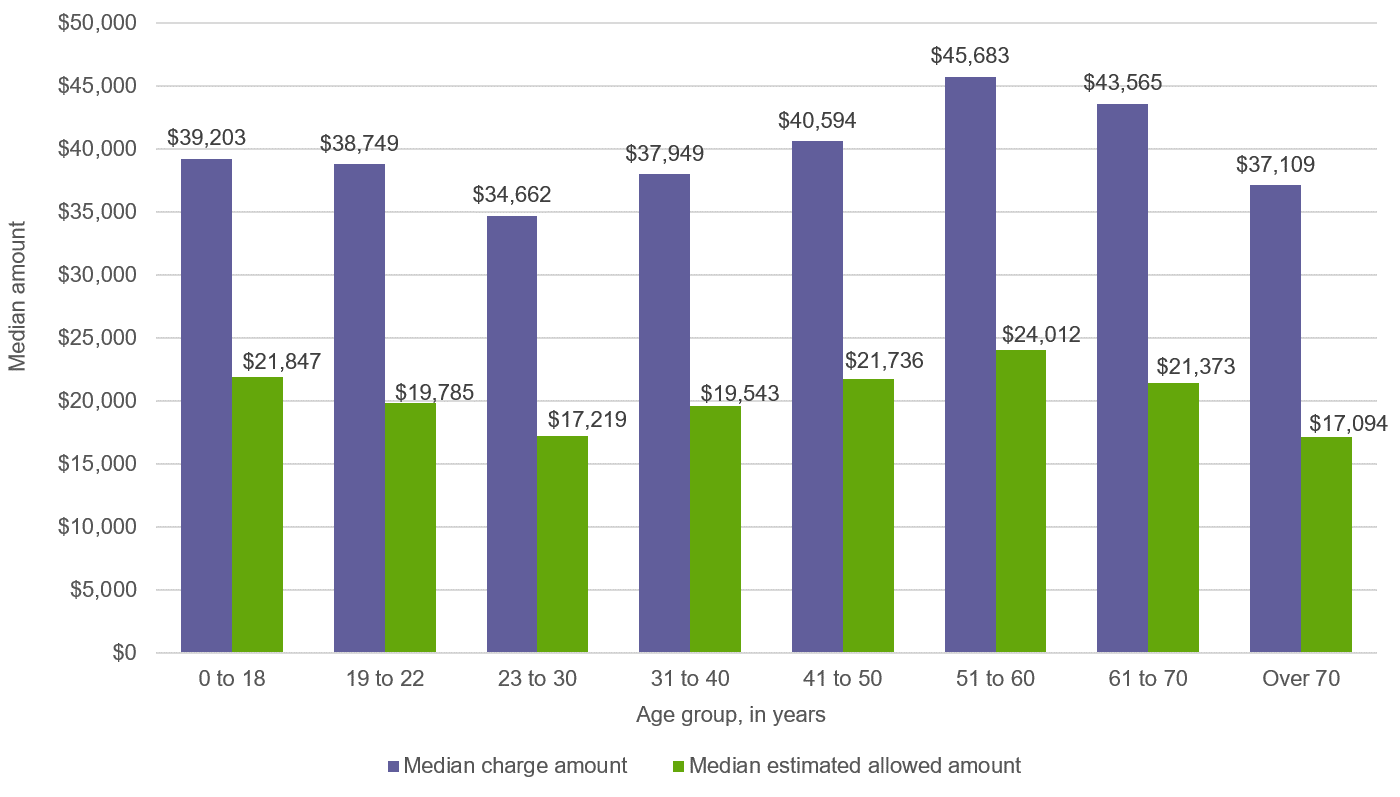
Source: FAIR Health
The West was the region with the widest range of costs for COVID-19 hospitalizations. There, median charge amounts ranged from $21,407 for the 19-22 age group to $93,459 for the over 70 age group. Median estimated in-network amounts ranged from $15,289 for the 19-22 age group to $60,205 for the over 70 age group.
Nationally, an office was the most common setting for initial presentation of patients with COVID-19: 33.3% of COVID-19 patients presented to an office and 23.0% presented to an inpatient facility (Figure 3). However, older people (age 61 and above) most commonly presented first to an inpatient setting.
FIGURE 3. Distribution of Patients with COVID-19 Diagnoses by Venue of Care Where First Diagnosed, Nationally, January-May 2020
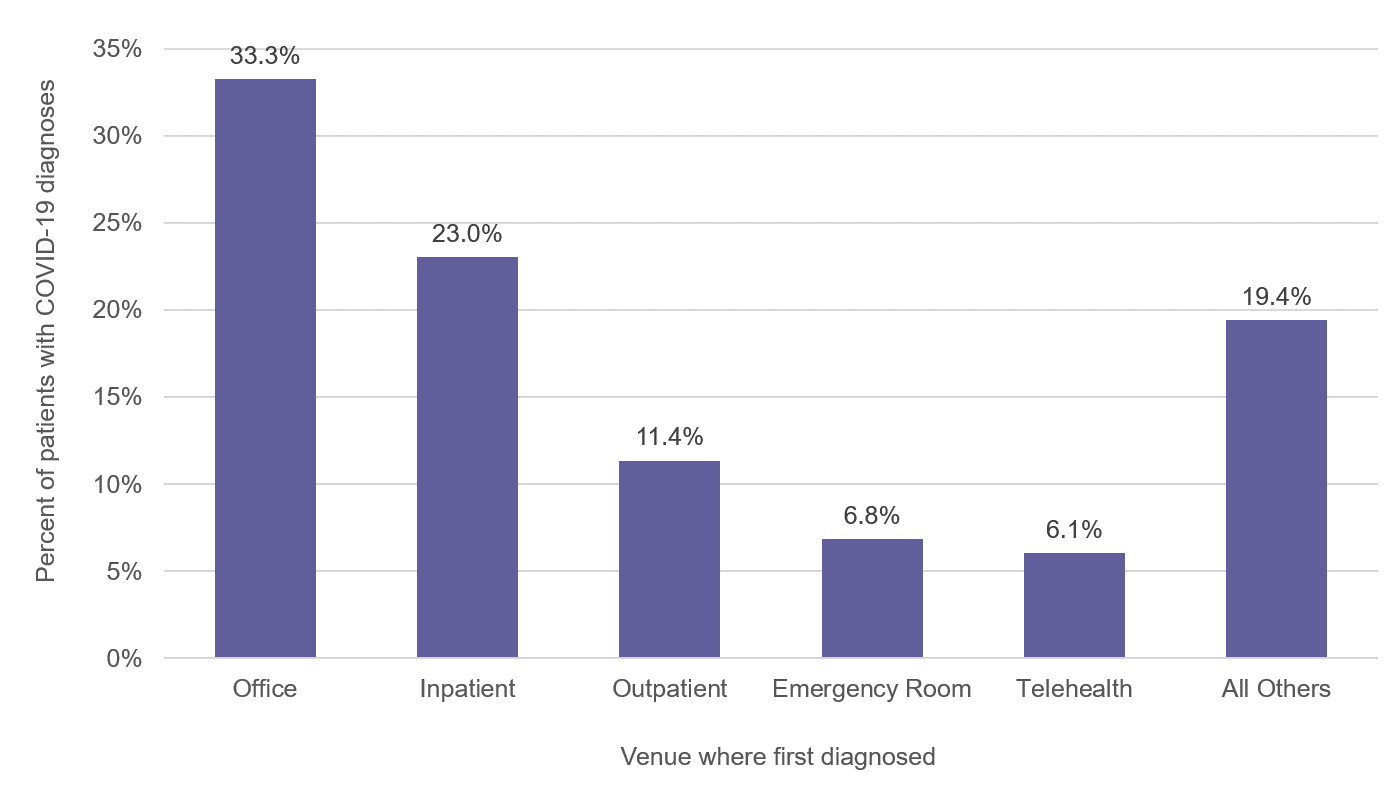
Source: FAIR Health
In the Northeast, telehealth was more common for initial diagnosis of COVID-19 than emergency rooms (6.7% vs 6.2% of COVID-19 patients). The Northeast was the region with the highest percentage of COVID-19 patients who received their initial diagnosis via telehealth.
Nationally, males were associated with a larger share (54%) of the distribution of COVID-19 claim lines than females (46%).
Nationally, during the January-May time frame, COVID-19 was most commonly associated with the age group 51-60, which accounted for 29.9% of the distribution of claim lines with this diagnosis. Children (0-18 years) accounted for the smallest share, 1.5%. (It should be noted, however, that the age distribution may be in flux, with the average age of new COVID-19 patients in the United States having dropped by about 15 years compared with a few months ago, according to recent reports.)
In the South, Midwest and West, the age groups 19-30 and 31-40 accounted for larger shares of the distribution of claim lines than in the Northeast and the nation as a whole.
Across age groups on the national level, rural and urban areas were similar in their association with COVID-19 claim lines. In the largest age group, 51-60, rural and urban areas had almost identical shares of the COVID-19 claim line distribution, respectively 30.2% and 30.3%.
Profiles of COVID-19 patients have many potential applications, including determining risk factors, influencing treatment protocols, setting priorities for eventual vaccination distribution, inspiring further research, and planning and budgeting for use of healthcare resources. FAIR Health presents this report to help support that broad range of applications by stakeholders throughout the healthcare sector.
This is the fourth in a series of briefs released by FAIR Health on the COVID-19 pandemic. The first brief examined projected US costs for COVID-19 patients requiring inpatient stays, the second the impact of the pandemic on hospitals and health systems, and the third the impact on healthcare professionals.
For the new brief, click here.
Author Information
Robin Gelburd, JD, is the President of FAIR Health, a national, independent nonprofit organization with the mission of bringing transparency to healthcare costs and health insurance information. FAIR Health possesses the nation’s largest collection of private healthcare claims data, which includes over 31 billion claim records contributed by payors and administrators who insure or process claims for private insurance plans covering more than 150 million individuals. Certified by the Centers for Medicare & Medicaid Services (CMS) as a national Qualified Entity, FAIR Health also receives data representing the experience of all individuals enrolled in traditional Medicare Parts A, B and D; FAIR Health includes among the private claims data in its database, data on Medicare Advantage enrollees. Ms. Gelburd is a nationally recognized expert on healthcare policy, data and transparency.
More Needs to Be Done to Reduce Racial Disparities in Home Dialysis
March 24th 2023On this episode of Managed Care Cast, we speak with Virginia Wang, PhD, and Matthew L. Maciejewski, PhD, who talk about their recent study on racial disparities in home dialysis, and what more needs to be done to increase uptake and reduce disparities in home dialysis for non-White patients.
Listen
