- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Preclinical Study Shows Promise of Dual Targeted Treatment Against TNBC
Early findings from a new preclinical study indicate that dual blockade of aurora-A kinase and PD-L1 signaling can inhibit tumor growth in triple-negative breast cancer (TNBC), treatment for which has historically remained limited.
Researchers of a new study say they may have unlocked a targeted approach against a hard-to-treat form of breast cancer.1
Early findings from the preclinical study indicate that dual blockade of aurora-A kinase (AURKA) and PD-L1 signaling can inhibit tumor growth in triple-negative breast cancer (TNBC), treatment for which has historically remained limited—particularly in an era of targeted treatments—due to lack of estrogen receptors (ER), progesterone receptors, and human epidermal growth factor receptor 2 expression.
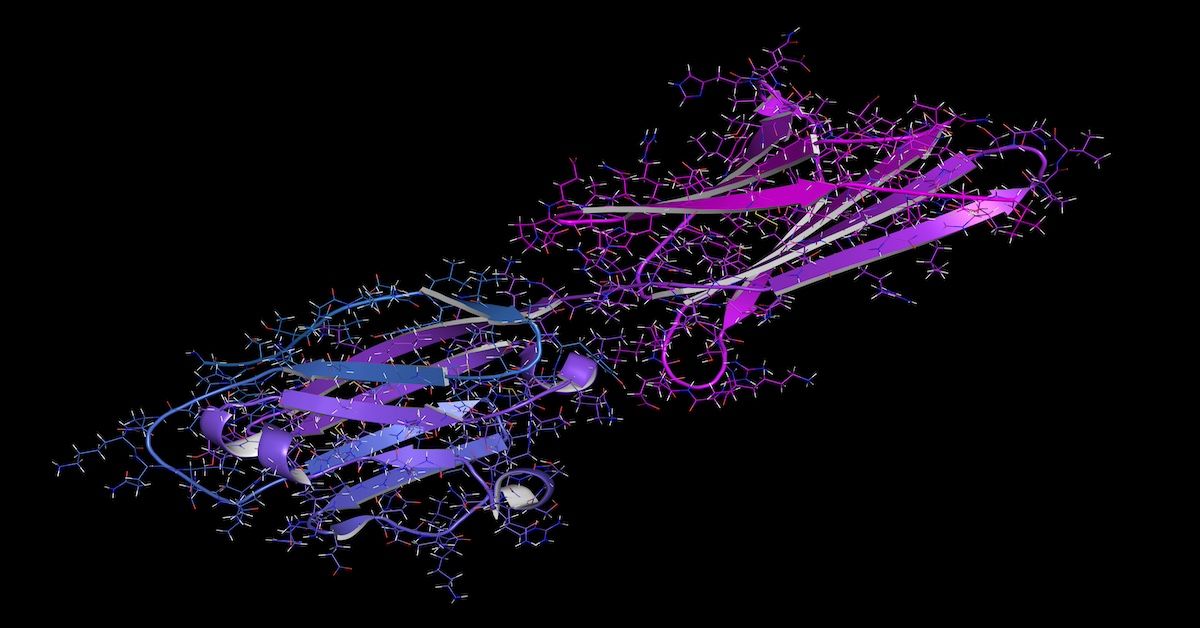
Investigators of this study found that inhibiting both aurora-A kinase and PD-L1 may inhibit tumor growth in triple-negative breast cancer | Image Credit: molekkuul.be stock.adobe.com
By blocking PD-L1, found the researchers, enrichment of ALDHhigh CSCs is hindered, thus eliminating resistance to AURKA-targeted treatment. These new findings have been published in Frontiers in Oncology.
“This study provides a strong preclinical rationale that dual AURKA and PD-L1 pharmacological blockade is an effective combinatorial therapeutic approach to inhibit TNBC progression through selective eradication of ALDHhigh cancer stem cells that are responsible for the high cancer cell plasticity and immunosuppressive activity,” wrote the researchers. “Pharmacological blockade of AURKA/PD-L1 oncogenic axis represents a major breakthrough in the treatment of metastatic TNBC, because it will lead to the development of novel combinatorial targeted therapies expected to meaningfully increase the progression-free and overall survival of patients with metastatic TNBC who are refractory to standard-of-care chemotherapy and show limited response to FDA-approved [immune checkpoint inhibitors].”
Drugs that target AURKA—a serine/threonine oncoprotein kinase associated with tumor progression and poor outcomes in TNBC—have emerged as effective options in preclinical and clinical settings of certain types of breast cancer. However, although the AURKA inhibitor alisertib has previously shown promise in ER-positive breast cancer, the treatment alone has not yielded favorable outcomes in triple-negative disease.
In line with previous findings, the researchers found worse survival associated with higher rates of AURKA expression. Among 269 samples from patients with TNBC from Mayo Clinic Cancer Center, 133 had high AURKA expression, which was significantly associated with recurrence-free survival over 5-year follow-up.
Testing the combined effect of AURKA inhibition with alisertib and PD-L1 inhibition with atezolizumab in vivo, the researchers assessed the combination against either agent alone or placebo every 3 weeks in mice with MDA-MB 23/LM tumor xenografts. Compared with placebo and either monotherapy, the combination elicited the strongest inhibition of tumor growth while being well tolerated, with no mouse losing more than 15% of its weight.
“Noteworthy, the combination of atezolizumab and alisertib triggered the reduced expression of the mesenchymal marker vimentin in tumor xenografts that was linked to lack of organ metastasis compared to atezolizumab or alisertib as monotherapy,” commented the researchers. “Because MDA-MB 231/LM tumor xenografts were established in immunocompromised NSG mice, the therapeutic efficacy of PD-L1 pharmacological blockade in enhancing alisertib efficiency was not immune-driven but it was exclusively linked to inhibition of tumor-intrinsic PD-L1 oncogenic signaling pathway.”
The group found similar findings ex vivoamong cells resistant to durvalumab, a treatment shown to improve outcomes in TNBC, including with neoadjuvant chemotherapy and in combination with datopotamab deruxtecan.2,3 When combined with either atezolizumab or durvalumab, atezolizumab resulted in the highest induction of apoptosis.
References
1. Takchi A, Zhang M, Jalalirad M, et al. Blockade of tumor cell-intrinsic PD-L1 signaling enhances AURKA-targeted therapy in triple negative breast cancer. Front Oncol. Published online May 29, 2024. doi:10.3389/fonc.2024.1384277
2. Loibl S, Schneeweiss A, Huober JB, et al. Durvalumab improves long-term outcome in TNBC: results from the phase II randomized GeparNUEVO study investigating neodjuvant durvalumab in addition to an anthracycline/taxane based neoadjuvant chemotherapy in early triple-negative breast cancer (TNBC). J Clin Oncol. 2021;39(suppl 15). doi:10.1200/JCO.2021.39.15_suppl.506
3. Schmid P, PJ Wysocki, CX Ma, et al. Datopotamab deruxtecan (dato-dxd) + durvalumab (d) as first-line (1L) treatment for unresectable locally advanced/metastatic triple-negative breast cancer (a/mTNBC): Updated results from BEGONIA, a phase Ib/II study. Ann Oncol. 2023;34(suppl 2):S337. doi:10.1016/j.annonc.2023.09.556
