- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
PI3K Inhibitors Face Challenges in Hematologic Malignancies
The PI3K cell-signaling network has been an important therapeutic target in oncology research for nearly 40 years ago, but the use of PI3K inhibitors in hematologic malignancies has come under scrutiny amid concerns about efficacy and safety.
A version of this article was originally published in OncologyLive. This version has been lightly edited.
The PI3K cell-signaling network has been an important therapeutic target in oncology research since its role in promoting multiple cancer types was first elucidated nearly 40 years ago.1 Such efforts began to pay off in 2014 when idelalisib (Zydelig) became the first PI3K inhibitor to gain FDA approval, with indications in relapsed follicular lymphoma (FL), small lymphocytic lymphoma (SLL), and chronic lymphocytic leukemia (CLL). The FDA subsequently approved 4 additional PI3K inhibitors for oncology indications.2
During the past year, however, the use of PI3K inhibitors in hematologic malignancies has come under scrutiny amid concerns about efficacy and safety.3 Since December 2021, pharmaceutical companies have voluntarily withdrawn indications for idelalisib in FL and SLL and for duvelisib (Copiktra) in FL; umbralisib (Ukoniq), which was approved in FL and marginal zone lymphoma (MZL), was completely withdrawn from the market.4,5
Further, the FDA’s Oncologic Drugs Advisory Committee (ODAC) voted in September 2022 against retaining indications for duvelisib for patients with relapsed or refractory (R/R) CLL or SLL after at least 2 prior therapies.6 Meanwhile, copanlisib (Aliqopa) maintains its indication as monotherapy for the treatment of adults with relapsed FL after at least 2 prior therapies; however, Bayer has withdrawn a supplemental new drug application pending analysis for the combination of copanlisib plus rituximab (Rituxan) in patients with relapsed indolent non-Hodgkin lymphoma (iNHL).7,8
Of note, questions about PI3K inhibitors in hematologic malignancies have not been raised about alpelisib (Piqray), which is approved in combination with fulvestrant (Faslodex) for patients with hormone receptor–positive,HER2-negative breast cancer harboring PIK3CA mutations.3,9 In April 2022, the FDA approved alpelisib under the trade name Vijoice for adult and pediatric patients with PIK3CA-related overgrowth spectrum, a set of rare genetic disorders caused by mutations in PIK3CA.10,11
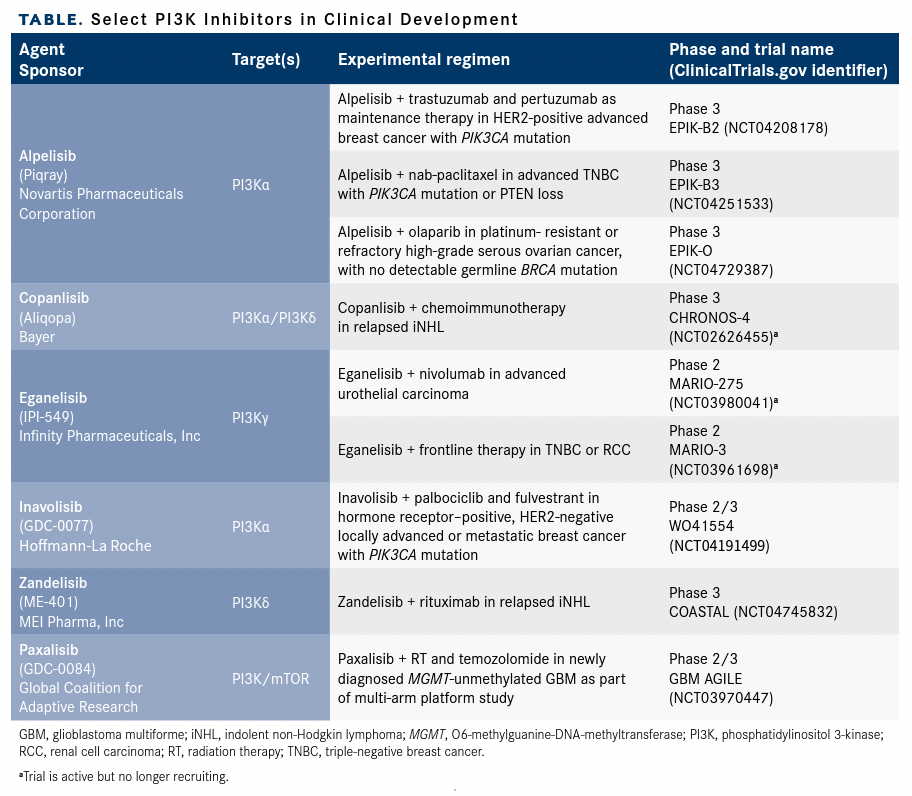
Investigators continue to explore PI3K inhibitors in hematologic settings. Additionally, the development of currently approved and emerging PI3K inhibitors continues in breast cancer and other solid tumors, according to a search of ClinicalTrials.gov (Table).
Table. Select PI3K Inhibitors in Clinical Development
Concerns About a Class of Agents
The FDA’s concerns about the class of PI3K inhibitors that have been approved for treating patients with hematologic malignancies involve 4 main issues: unfavorable trends in overall survival (OS) data, toxicity profiles, questions about inadequate dose optimization, and the use of single-arm trials.3
Despite initial FDA approvals based on progression-free survival (PFS) or overall response rate (ORR), findings from 6 postmarketing randomized clinical trials have prompted concerns about the impact of these agents on OS, FDA officials said in briefing documents prepared for an ODAC meeting in April 2022.3 At that meeting, the ODAC panel voted 16 to 0 (with 1 abstention) to require randomized studies of future PI3K inhibitors in hematologic malignancies rather than basing approval decisions on the results of single-arm studies.12
Idelalisib
The postapproval studies that the FDA cited include 3 randomized trials—GS-US-312-0123 (NCT01980888), GS-US-313-0124 (NCT01732913), and GS-US-313-0125 (NCT01732926)— evaluating idelalisib-containing combinations vs placebo-controlled regimens for patients with CLL or iNHL.3
In 312-0123, the HR for idelalisib plus bendamustine and rituximab vs bendamustine/ rituximab alone in patients with untreated CLL was 3.34 (95% CI, 1.08-10.39), and deaths in the 2 arms were 8% vs 3%, respectively. In 313-0124, the HR for idelalisib plus rituximab vs rituximab alone in patients with previously treated iNHL was 4.74 (95% CI, 0.6-37.12), and deaths were 5% and 1%, respectively. In 313-0125, the HR for idelalisib plus bendamustine and rituximab vs bendamustine/rituximab in patients with previously treated iNHL was 1.51 (95% CI, 0.713.23), and deaths were 8% vs 6%, respectively.4
The trials were halted due to increased deaths or toxicities in March 2016.3
The FDA initially granted an accelerated approval for idelalisib for R/R FL or SLL after 2 prior therapies and regular approval for relapsed CLL in 2014. Gilead Sciences, Inc voluntarily withdrew the FL and SLL indications in February 2022.4,13
Meanwhile, idelalisib retains its indication in combination with rituximab in patients with relapsed CLL for whom rituximab alone would be considered appropriate therapy due to other comorbidities.13 The combination showed an improvement in PFS, the primary end point, over placebo plus rituximab in study GS-US-312-0116 (NCT01539512), an earlier trial of idelalisib that supported the combination’s regular approval for CLL in 2014.3
At the final analysis, the updated median PFS was 19.4 months (95% CI, 12.3-not reached) with idelalisib vs 6.5 months (95% CI, 4.0-7.3) in the control arm, which translated into an HR of 0.15 (95% CI, 0.09-0.24; P < .0001).13 The study was not designed to assess OS, but an exploratory analysis “indicated a potential survival benefit in the idelalisib-plus-rituximab arm,” with an HR of 0.34 (95% CI, 0.19-0.60; P = .0001), according to the FDA.3
Duvelisib
FDA officials also noted a pattern of declining benefit for other PI3K inhibitors. In September 2018, the FDA granted regular approval to duvelisib for patients with R/R CLL or SLL after at least 2 prior therapies and accelerated approval for adults with R/R FL after at least 2 prior systemic therapies. The indications were based on findings from the phase 3 DUO study (NCT02004522), in which adult patients were randomly assigned to treatment with duvelisib or ofatumumab (Arzerra). The trial recruited patients whose disease had relapsed after 1 prior therapy; most of the participants (312 of 319) had CLL.14,15
The benefit-risk profile was deemed greater in patients with at least 2 prior therapies. Among these patients, the median PFS with duvelisib was 16.4 months compared with 9.1 months with ofatumumab (HR, 0.40; SE, 0.2). The ORR was 78% and 39% for the duvelisib and ofatumumab arms, respectively.14,15
Findings for OS, a key secondary end point, were immature when the primary analysis was conducted. However, final 5-year data favored the control arm, FDA officials said in their briefing document. The HRs for the total study population were 1.09 (95% CI, 0.79-1.51) for the total study population and 1.06 (95% CI, 0.71, 1.58) for participants with 2 or more prior therapies. Deaths also were higher with duvelisib than ofatumumab among patients who had received 1 prior therapy (50.0% vs 44.0%, respectively) and among those with 2 or more therapies (55.8% vs 48.5%, respectively).3
In response, Secura Bio, Inc, which is developing duvelisib, argued that the final OS results do not reflect negatively on the drug. Most patients on the ofatumumab arm crossed over to duvelisib, and none of the participants remained on either study drug at the 5-year mark, according to David Sidransky, MD, a clinical adviser to Secura Bio.16 Sidransky is director of Head and Neck Cancer Research in the Department of Otolaryngology Head and Neck Surgery at Johns Hopkins University in Baltimore, Maryland.
Moreover, the OS findings were neutral at the interim and final analyses, Sidransky maintained. At 3 years, when most patients who were still on the study had received duvelisib, the OS rate was comparable at 59% with duvelisib and 60% with ofatumumab, he said.16
The FDA has not announced a final decision on the CLL/SLL indication for duvelisib following the ODAC meeting. Meanwhile, Secura Bio voluntarily withdrew the indication for duvelisib in R/R FL in December 2021, which was based on findings from a single-arm trial (NCT02204982).14,17 The treatment landscape for FL has changed since duvelisib gained accelerated approval more than 4 years ago, casting doubts on the merits of the logistics, cost, and timing of a confirmatory study, the company said.17
At the same time, Secura Bio is continuing the development of duvelisib in hematologic malignancies, with ongoing phase 2 studies in R/R peripheral T-cell lymphoma, R/R CLL, iNHL, and other tumor types. The PRIMO trial (NCT03372057) evaluating duvelisib as a single agent in R/R peripheral T-cell lymphoma is fully enrolled.18
Copanlisib
In September 2017, the FDA granted an accelerated approval for copanlisib for treating adults with R/R FL who have received at least 2 prior therapies based on ORR data from the single-arm, phase 2 CHRONOS-1 trial (NCT01660451).3,4
The FDA has raised concerns about findings from the phase 3 CHRONOS-3 trial (NCT02367040), in which patients with previously treated iNHL were randomly assigned to receive rituximab with or without copanlisib.
The copanlisib combination demonstrated an improvement vs rituximab plus placebo in PFS, the primary end point, in the intention-to-treat (ITT) population with iNHL. The median PFS with the copanlisib regimen was 21.5 months (95% CI, 17.8-33.0) vs 13.8 months (95% CI, 10.2-17.5) with rituximab alone (HR, 0.52; 95% CI, 0.39-0.69). A PFS benefit also was seen in the subsets of patients with FL (HR, 0.58; 95% CI, 0.40-0.83) and MZL (HR, 0.48; 95% CI, 0.25-0.92).3
However, an updated analysis of OS, an exploratory end point of the study, “raised concern for a potentially higher risk of death in the copanlisib-plus-rituximab arm,” the FDA said. With a data cutoff of August 2021, the HRs for OS were 0.87 (95% CI, 0.57-1.35) for the ITT population, 0.95 (95% CI, 0.52-1.74) for participants with FL, and 1.07 (95% CI, 0.38-3.00) for the MZL subgroup. The median OS was not estimable for any of the cohorts due to a low number of observed deaths. Death rates for the copanlisib combination were 18% for the ITT population, 16% for patients with FL, and 20% for participants with MZL compared with 21%, 18%, and 17%, respectively, with rituximab alone.3
“While the wide confidence intervals of the OS HR and the survival percentage difference indicated estimate uncertainty, potential harm to patients in the copanlisib-plus-rituximab arm cannot be ruled out,” FDA officials said in the briefing document.3
Bayer submitted a supplemental new drug application for the copanlisib combination in relapsed iNHL based on the CHRONOS-3 data in May 2021 but withdrew the application in December 2021.3 The company said existing and additional data would be analyzed and the potential for a resubmission would be assessed.8 The designated confirmatory trial for FL, CHRONOS-4 (NCT02626455), is ongoing. The phase 3 study, which is active but no longer recruiting participants, is testing standard chemoimmunotherapy with or without copanlisib in patients with R/R FL or MZL.3
Umbralisib
In February 2021, the FDA granted accelerated approvals for umbralisib for treating adults with R/R MZL who have received at least 1 anti–CD20based regimen and for patients with R/R FL after at 3 prior lines of systemic therapy based on ORR and duration-of-response rates in the single-arm phase 2/3 UNITY-NHL trial (NCT02793583).19
A year later, however, the FDA issued a warning about the potential for an increased risk of death with umbralisib therapy after an initial review of data from the phase 3 UNITY-CLL trial (NCT02612311).20
The study was evaluating the combination of umbralisib plus ublituximab, an anti-CD20 monoclonal antibody, compared with obinutuzumab (Gazyva), which also is directed at CD20, plus chlorambucil in patients with previously untreated and R/R CLL.
Data from UNITY-CLL were submitted in March 2021 to support a supplemental new drug application for the combination in this population.3 The findings showed that median PFS, the primary end point, was 31.9 months (95% CI, 28.235.8) with the umbralisib combination compared with 17.9 months (95% CI, 16.6-22.6) with the obinutuzumab regimen (HR, 0.546; 95% CI, 0.4130.720; P < .0001).
Despite the PFS benefit, the interim OS outcomes favored the control arm (HR, 1.23), and patients who received the novel combination experienced more serious adverse events (AEs).4,20 The possibility of a higher incidence of deaths due to the novel combination prompted the FDA to place multiple clinical trials involving the 2 drugs on hold.3 In April 2022, TG Therapeutics, Inc notif ied the agency that it would voluntarily withdraw the indications for FL and MZL.20
Toxicity Profiles
Overall, the findings suggest that the toxicity profiles of PI3K inhibitors have a detrimental impact on OS in patients with CLL or iNHL, the FDA said. As monotherapies, the 4 PI3K inhibitors that the FDA analyzed have demonstrated rates of AEs of grade 3 or greater severity ranging from 51% to 85%, including infection (20%-27%) and neutropenia (17%-43%).4
“The consistent findings of decrements in overall survival in 6 randomized trials in the setting of an advantage or potential advantage in PFS [are] unprecedented in oncology,” FDA officials stated in the April briefing document.3 “The overall survival information is early and represents a low number of events, yet we have the same pattern observed across multiple trials. Further, in each trial, there was a higher rate of death due to adverse events in the PI3K inhibitor arm, suggesting the potential detriment in overall survival may be due to toxicity.”
The toxicity profiles observed with PI3K inhibitors in hematological settings are associated with the agents’ distinct mechanisms of action, which vary according to the target isoform of PI3K. Each of the agents inhibits the PI3Kδ isoform, and duvelisib and copanlisib also inhibit PI3Kγ and PI3Kα, respectively.21 Copanlisib also has been described as a pan-PI3K inhibitor because it shows activity against all 4 PI3K isoforms.2
Inhibitors of the δ and γ isoforms, which are preferentially expressed on leukocytes, are associated with infections and immune-mediated toxicities. “Infection may occur in part because of treatment-related cytopenias, but also because of the modulation of the immune system by the PI3 kinase inhibitor,” Nicholas C. Richardson, DO, MPH, said during an FDA webcast about PI3K inhibitors presented May 12, 2022.21 Richardson is a clinical team leader in the Division of Hematologic Malignancies II in the FDA’s Office of Oncologic Diseases.
He said infections include pneumonia, opportunistic infections such as Pneumocystis jirovecii, and cytomegalovirus reactivation. Immunerelated toxicities may result from a decrease in regulatory T-cell activity, causing damage to healthy tissue, with AEs such as hepatitis, pneumonitis, colitis, and rash.
Inhibition of the α isoform may cause hyperglycemia and hypertension. “The α isoform is ubiquitously expressed and is essential to cellular growth and metabolism and glucose homeostasis,” Richardson said.
Moreover, the establishment of optimal doses across this class of agents also has been problematic, particularly because there is a narrow difference between an effective dose and toxic exposure, Richardson said. He said the relationships between exposure to the drug with safety and toxicity have not been sufficiently explored. The FDA is seeking to improve the evaluation and optimization of oncology drugs through its Project Optimus program.21
The experience with PI3K inhibitors in hematology highlights the pitfalls of using data from single-arm trials for drug approvals, according to FDA officials. All the drugs under discussion gained indications for FL, SLL, and/or MZL based on ORR data from single-arm trials. In general, the limitations of single-arm trials include challenges in interpreting safety and efficacy data without comparator arms, questions about whether response rates will be predictive of clinical benefit, and difficulties interpreting the results of time-to-event end points such as PFS.3,4
Moving forward, the FDA will be looking for randomized clinical trial data in drug applications for PI3K inhibitors in hematologic malignancies, with OS as the preferred end point. The PI3K inhibitor journey also holds lessons for drug development in general, noted Yvette Kasamon, MD, during the webinar. Kasamon, who also is a clinical team leader in the Division of Hematologic Malignancies II in the FDA’s Office of Oncologic Diseases, said these lessons include the need for adequate justification for dosing levels, the limitations of single-arm trials, and the importance of OS as an end point.21
The Need For Randomized Data
The impact of the FDA’s stance on PI3K inhibitors is reverberating in the drug development f ield. In March 2022, the FDA informed the developers of the selective PI3Kδ inhibitor zandelisib that randomized data would be required for a new drug application, according to the drug’s developers, MEI Pharma, Inc and Kyowa Kirin Co, Ltd.22
The drugmakers had planned to seek accelerated approval for zandelisib based on data from the single-arm phase 2 TIDAL study (NCT03768505) in patients with R/R FL or MZL after 2 or more prior therapies. The FDA’s position on the need for randomized data marks the first time the agency has declined to consider results of a single-arm study as a basis for accelerated approval, representatives of the companies said.22
The supporting data are expected to eventually come from the ongoing phase 3 COASTAL study (NCT04745832) comparing zandelisib plus rituximab against standard-of-care chemotherapy plus rituximab in patients with R/R FL or MZL who have received more than 1 prior line of therapy including an anti-CD20 antibody in combination with chemotherapy or lenalidomide (Revlimid).22
A month later, the ODAC panel formally endorsed the need for randomized data for this class of drugs to be considered for FDA approval for hematologic indications. That decision likely will hamper plans for several investigational PI3K inhibitors under development for hematologic cancers, market analysts say.23
Finding Better Ways to Target PI3K
Investigators have been focusing on several strategies to boost the efficacy of PI3K inhibitors, with a focus on reducing toxicities, designing combination regimens, and overcoming resistance.
Some experts believe that exploring new scheduling and dosing regimens would result in fewer toxicities and an improved therapeutic index.18 In this vein, some studies of novel PI3K inhibitors have tested intermittent dosing, as opposed to continuous dosing at the maximum tolerated dose identified in phase 1 trials.2
Although combining PI3K inhibitors with other targeted therapies has been challenging, there may be opportunities for rational combinations in patients with PIK3CA-mutant tumors.1,24,25
In terms of resistance to PI3K inhibition, several mechanisms of intrinsic and acquired resistance have been described, such as reactivation of the PI3K pathway through feedback loops and activation of compensatory parallel signaling cascades.2,26 In a patient with PIK3CA-mutated breast cancer, for example, the inhibition of PI3K signaling led to recurrent PTEN loss, which in turn may limit the antiproliferative impact of PI3K-directed therapy.2
References
- Vivanco L, Sawyers CL. The phosphatidylinositol 3-Kinase AKT pathway in human cancer. Nat Rev Cancer. 2002;2(7):489-501. doi:10.1038/nrc839
- Vanhaesebroeck B, Perry MWD, Brown JR, André F, Okkenhaug K. PI3K inhibitors are finally coming of age. Nat Rev Drug Discov. 2021;20(10):741-769. doi:10.1038/s41573-021-00209-1
- Phosphatidylinositol 3-Kinase (PI3K) inhibitors in hematologic malignancies. FDA. April 21, 2022. Accessed October 19, 2022. https:// bit.ly/3gdTXbP
- Gormley N. FDA introductory comments. Oncologic Drugs Advisory Committee Meeting. April 21, 2022. Accessed October 19, 2022. https://bit.ly/3Sfivyo
- FDA withdrew its approval for the cancer medicine Ukoniq (umbralisib) due to safety concerns. FDA. Drug Safety Podcast. July 7, 2022. Accessed November 1, 2022. https://bit.ly/3FC651c
- Lovely B. Duvelisib loses support for CLL/SLL indication following ODAC meeting. OncLive®. September 23, 2022. Accessed October 19, 2022. https://bit.ly/3MLGEM1
- Aliqopa. Prescribing information. Bayer Healthcare Pharmaceuticals Inc; 2022. Accessed October 19, 2022. https://bit.ly/3CLcjsu Bayer AG.
- Annual report 2021. March 1, 2022. Accessed October 19, 2022. https://bit.ly/3CJz6oE
- Piqray. Prescribing information. Novartis Pharmaceuticals Corporation; 2022. Accessed October 19, 2022. https://bit.ly/3TAXU8U
- FDA approves alpelisib for PIK3CA-related overgrowth spectrum.FDA. Updated April 6, 2022. Accessed October 19, 2022. https:// bit.ly/3DaMiUV
- Rare Disease Database: PIK3CA-related overgrowth spectrum. National Organization for Rare Disorders. Published 2022. Accessed October 19, 2022. https://bit.ly/3srmWfr
- OncLive® staff. ODAC unanimously votes to recommend randomized data for approval of PI3K inhibitors in hematologic cancers. OncLive®. April 21, 2022. Accessed October 19, 2022. https://bit.ly/3TzaxRV
- Zydelig. Prescribing information. Gilead Sciences Inc; 2022. Accessed October 19, 2022. https://bit.ly/3VFUu6N
- Duvelisib (Copiktra, Verastem, Inc.) for adult patients with relapsed or refractory chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL). FDA. Updated September 24, 2018. https:// bit.ly/3fu43Wd
- Copiktra. Prescribing information. Secura Bio Inc; 2021. Accessed November 3, 2022. https://bit.ly/3h7g9oL
- Secura Bio. Duvelisib for treatment of patients with relapsed or refractory chronic lymphocytic leukemia/small lymphocytic lymphoma. September 23, 2022. Accessed November 3, 2022. https://bit. ly/3h8BzSk
- Secura Bio announces Copiktra (duvelisib) strategic focus on T-cell lymphoma and voluntary U.S. withdrawal of the relapsed or refractory follicular lymphoma indication. News release. Secura Bio Inc. December 3, 2021. Accessed November 3, 2022. https://prn.to/3UEdIIP
- Pipeline: clinical trials. Secura Bio. Accessed November 3, 2022. https://bit.ly/3T39VTV
- FDA grants accelerated approval to umbralisib for marginal zone lymphoma and follicular lymphoma. FDA. Updated February 5, 2021. Accessed November 3, 2022. https://bit.ly/3Dxwg6A
- TG Therapeutics, Inc.; withdrawal of approval of new drug application for Ukoniq (umbralisib tosylate) tablets, equivalent to 200 milligrams base. Fed Regist. Published online May 31, 2022. Accessed November 3, 2022. https://bit.ly/3sZxPVX
- Richardson NC, Kasamon Y. The saga of phosphatidylinositol 3-kinase (PI3K) inhibitors. FDA Grand Rounds. May 12, 2022. Accessed October 19, 2022. https://bit.ly/3TDtSkP
- MEI Pharma and Kyowa Kirin provide regulatory update on zandelisib following meeting with the FDA. News release. MEI Pharma Inc and Kyowa Kirin Co Ltd. March 24, 2022. Accessed October 19, 2022. https://yhoo.it/3tOTmC5
- Plieth J. What next for developers seeking to emulate Zydelig? Evaluate Vantage. April 22, 2022. Accessed October 19, 2022. https://bit.ly/3ThnxvT
- FDA approves alpelisib for metastatic breast cancer. FDA. Updated May 28, 2019. Accessed October 20, 2022. https://bit.ly/3yWIpQU
- André F, Ciruelos EM, Juric D, et al. Alpelisib plus fulvestrant for PIK3CA-mutated, hormone receptor-positive, human epidermal growth factor receptor-2-negative advanced breast cancer: final overall survival results from SOLAR-1. Ann Oncol. 2021;32(2):208217. doi:10.1016/j.annonc.2020.11.011
- Castel P, Toska E, Engelman JA, Scaltriti M. The present and future of PI3K inhibitors for cancer therapy. Nat Cancer. 2021;2(6):587597. doi:10.1038/s43018-021-00218-4
