- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Patients With MPNs Have Increased Risk of Thrombosis, Hemorrhage, Leukemic Transformation
Compared with matched controls, patients with myeloproliferative neoplasms (MPNs) had a higher risk of developing thrombosis, hemorrhage, and leukemic transformation, according to a longitudinal cohort study.
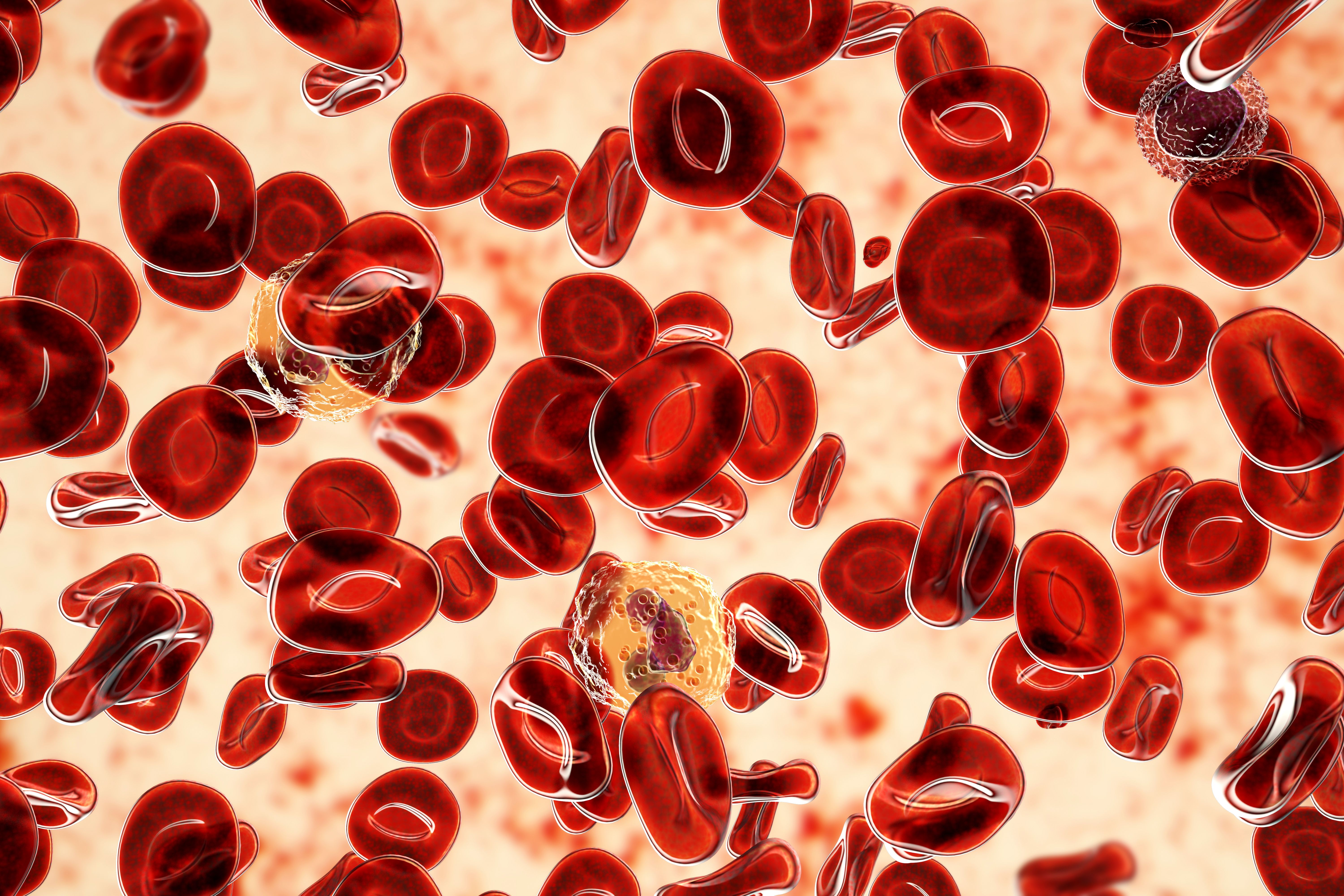
Polycythemia vera is one of the diseases categorized as myeloproliferative neoplasms.
Image credit: Dr_Microbe - stock.adobe.com
Patients with myeloproliferative neoplasms (MPNs) are at a higher risk of developing arterial thrombosis, venous thrombosis, hemorrhage, and leukemia transformation compared with matched controls without MPNs, highlighting the need for strategies to reduce the risk of these events, according to a study published in Thrombosis Research.1
MPNs are a group of diseases that begin with a mutation in the bone marrow that causes too many red blood cells, white blood cells, or platelets.2 MPNs include essential thrombocythemia (ET), polycythemia vera (PV), and primary myelofibrosis (PMF).
Although new treatments and adapted disease management have increased the expected overall survival of patients with MPNs, the incidence of MPNs has also increased over the last 2 decades, the researchers noted.
“In contrast to hematologic malignancy, the natural history of MPNs is benign, and the median follow-up time is usually measured in decades rather than years with supportive care alone,” they wrote.
Complications related to thrombosis and hemorrhage are a major cause of morbidity and mortality for patients with MPNs. While leukemic transformation is rare, it is fatal.
To assess the incidence and risk factors for thrombosis, hemorrhage, and leukemia transformation in patients with MPNs, the researchers conducted a population-based study using health claim data from the Korean National Health Insurance Service. Patients with MPNs were compared with matched control participants.
A total of 11,991 patients with MPN were included and 47,964 matched controls without an MPN diagnosis. The most common MPN was ET (61.3%), followed by PV (26.2%), unspecified MPNs (MPN-U; 6.2%), and PMF (6.1%). Patients with MPN had higher levels of hypertension, diabetes, dyslipidemia, atrial fibrillation/flutter, history of cancer, and chronic kidney disease compared with the individuals in the control group. Hypertension was the most common comorbidity in both groups (50.2% in the MPN group and 38.4% in the control group).
The study had a median follow up of 7.8 years, during which time:
- 30.1% in the MPN group and 19.0% in the control group developed arterial thrombosis
- 11.6% in the MPN group and 6.4% in the control group developed venous thrombosis
- 18.7% in the MPN group and 12.1% in the control group developed hemorrhage
- 4.9% in the MPN group and 0.1% in the control group developed leukemia
Patients with any MPN had overall higher risks than the participants in the matched control group for developing thrombosis, hemorrhage, or leukemic transformation. Patients with ET had the highest incidence rate (59.09 per 1000 person-years [PY]) during follow-up for arterial hypertension. Patients with PMF had the highest incidence rates for venous thrombosis (32.96 per 1000 PY), hemorrhage (55.47 per 1000 PY), and leukemic transformation (68.04 per 1000 PY).
One of the limitations of the study was that clinical factors, such as biological and molecular risk factors, were not considered due to the nature of the administrative claims database used. In Korea, prior to 2010, PMF was classified as MPN-U, which meant that in order to maximize the accuracy of the data, the study only included data after 2011. Due to the inclusion of participants from a single Asian country, the generalizability of the findings to other global populations is limited.
“We hope that these results will be used as primary data for treating and researching MPNs,” the authors concluded. “Strategies are warranted to reduce the risk of thrombosis, hemorrhage, and leukemic transformation in MPN patients.”
References
1. Hur JY, Choi N, Choi JH, Kim J, Won Y-W. Risk of thrombosis, hemorrhage and leukemic transformation in patients with myeloproliferative neoplasms: a nationwide longitudinal cohort study. Thromb Res. Published online March 6, 2024. doi:10.1016/j.thromres.2024.03.008
2. Chronic myeloproliferative neoplasms Treatment (PDQ)—patient version. National Cancer Institute. Updated November 17, 2023. Accessed March 13, 2024. https://www.cancer.gov/types/myeloproliferative/patient/chronic-treatment-pdq#:~:text=Myeloproliferative%20neoplasms%20are%20a%20group,to%20diagnose%20chronic%20myeloproliferative%20neoplasms.
Quality of Life: The Pending Outcome in Idiopathic Pulmonary Fibrosis
February 6th 2026Because evidence gaps in idiopathic pulmonary fibrosis research hinder demonstration of antifibrotic therapies’ impact on patient quality of life (QOL), integrating validated health-related QOL measures into trials is urgently needed.
Read More
