- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Patients With Eye Diseases at Increased Risk of Falls, Fractures
Patients who had cataracts, age-related macular degeneration, and/or glaucoma were at an increased risk of falling and sustaining fractures.
Advice, access, and referrals to fall prevention services could be beneficial in patients who have 1 or more eye diseases, as they have an increased risk of falls and fractures, according to a study published in JAMA Ophthalmology.
Age-related macular degeneration (AMD), glaucoma, and cataracts are the leading causes of visual loss related to age, with vision loss being associated with increases in morbidity and mortality due to physical injuries and disabilities. Falls can be caused by poor vision, but the specific diseases related to that poor vision have not been evaluated for their association with falling. This study aimed to investigate if risk of falls or fractures was higher in patients with cataracts, AMD, or glaucoma compared with patients without these eye diseases.
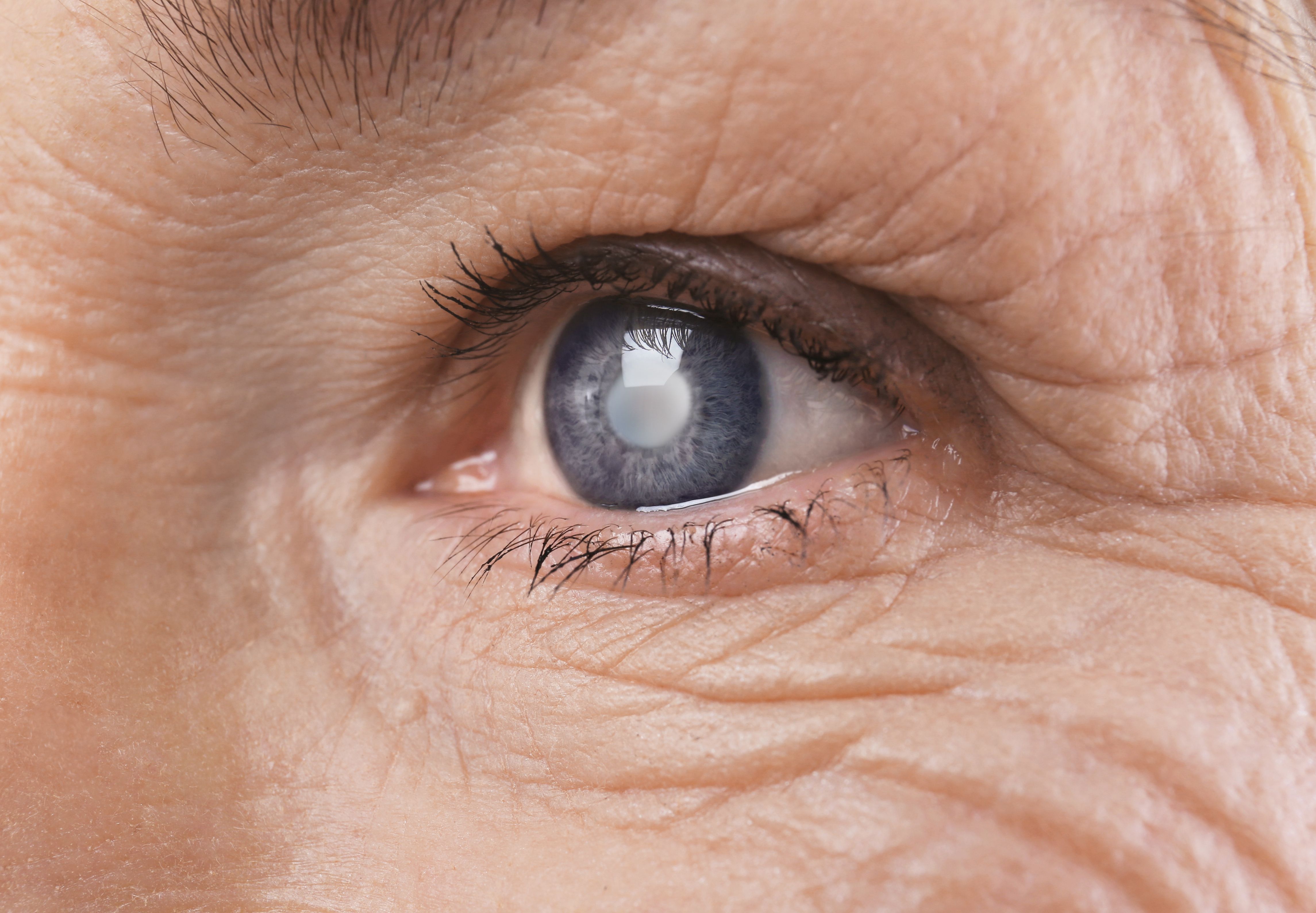
Eye of older woman | Image credit: Africa Studio - stock.adobe.com
The retrospective cohort study used the Clinical Practice Research Datalink GOLD and Aurum UK databases for this study. The data came from more than 2200 primary care practices and included 18 million patients. Demographics, clinical events, prescriptions, and specialist referrals were included in the dataset.
There were 3 cohorts for patients 18 years and older who had cataracts, AMD, or glaucoma. Patients were identified from April 1, 2007, to March 31, 2020. Monocular vs binocular diagnoses were not determined. The first recorded eye disease was used as the study entry date, and the end of follow-up was the date of death, date the study ended, date of deregistration from the practice, or the last day of data collection. The rates of incident falls and incident fractures were the primary outcomes of the study, which were identified using the codes from International Statistical Classification of Diseases and Related Health Problems, Tenth Revision. Medications that were linked to an increase in the risk of falling and fracturing bones were also investigated.
The cohort had a mean (SD) age of 74.3 (11.5) years, which was split into 73.8 (11.0) years in the cataract group, 79.4 (9.4) years in the AMD group, and 69.8 (13.1) years in the glaucoma group. Women made up more than half of each group (57.2%, 62.2%, and 51.9%, respectively). A higher level of comorbidities and morbidity was found in all populations with an eye disease. These populations also had a higher proportion of patients using benzodiazepines, antidepressants, antihypertensives, systemic steroids, antidiabetes medication, and medications with a high anticholinergic burden.
An increased incidence of falls and fractures occurred in patients with eye diseases during the study period. Compared with the controls, patients with cataracts (29.7% vs 13.9%), AMD (37.1% vs 20.7%), and glaucoma (25.0% vs 12.8%) had a higher proportion of patients who fell. A similar result was found in patients who had fractures, with a higher proportion of patients with cataracts (14.4% vs 8.2%), AMD (17.8% vs 11.6%), and glaucoma (12.2% vs 7.3%) having fractures compared with controls.
A multivariable Cox regression analysis found an increased risk of falls in patients with cataracts (HR, 1.36; 95% CI, 1.35-1.38), AMD (HR, 1.25; 95% CI, 1.23-1.27), and glaucoma (HR, 1.38; 95% CI, 1.35-1.41) vs controls. Fractures also had an increased risk of occurring in patients with glaucoma (HR, 1.31; 95% CI, 1.27-1.35), cataracts (HR, 1.28; 95% CI, 1.27-1.30), and AMD (HR, 1.18; 95% CI, 1.15-1.21).
There were some limitations to this study. Imperfect data that relied on coding and follow-ups that were irregular could have resulted from using retrospective data. Misclassification bias also is possible due to some patients who could have an undiagnosed eye disease. In addition, visual function was not evaluated objectively, treatments during follow-up were not evaluated, some of the fractures may not have been due to falls, and an underestimation of falls is possible.
Patients who have eye diseases, specifically cataracts, AMD, or glaucoma, are at a higher risk of falling and fracturing a bone due to their disease. Having patients receive fall prevention services and targeted interventions after receiving advice and referrals should be a priority in order to prevent adverse outcomes in this population.
Reference
Tsang JY, Wright A, Carr MJ, et al. Risk of falls and fractures in individuals with cataract, age-related macular degeneration, or glaucoma. JAMA Ophthalmol. Published online December 28, 2023. doi:10.1001/jamaophthalmol.2023.5858
Subjective and Objective Impacts of Ambulatory AI Scribes
January 8th 2026Although the vast majority of physicians using an artificial intelligence (AI) scribe perceived a reduction in documentation time, those with the most actual time savings had higher relative baseline levels of documentation time.
Read More
