- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
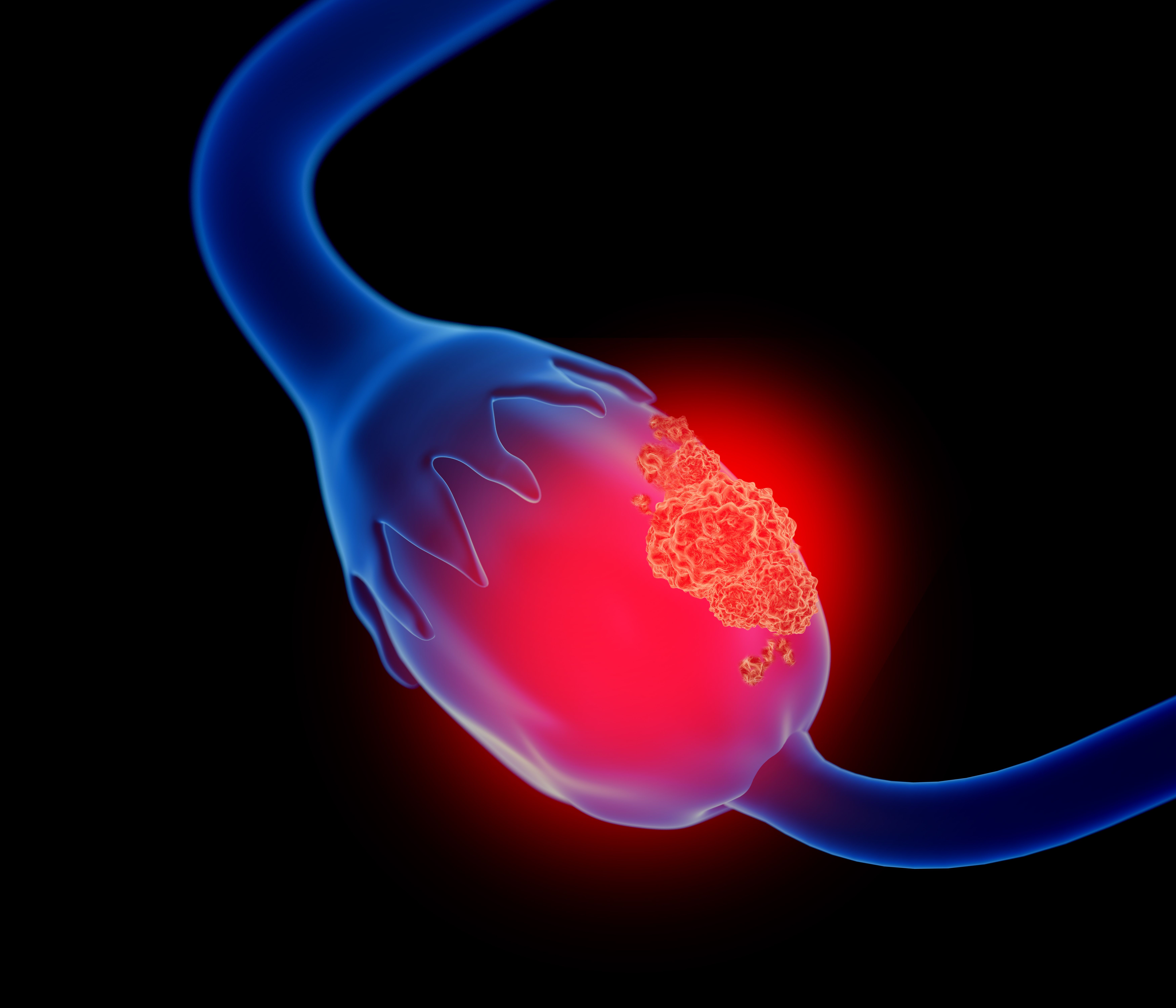
Patients With Endometriosis May Have Higher Ovarian Cancer Risk
Patients with endometriosis have a 4.2-fold greater ovarian cancer risk, highlighting the need for further research into the biological links between endometriosis subtypes and ovarian cancer.
Patients with endometriosis have a 4.2-fold increased ovarian cancer risk, according to a study published in JAMA.1
The researchers noted that endometriosis affects about 11% of reproductive-age women.2 Although infertility and pelvic pain are the most well-known endometriosis comorbidities, ovarian, endometrial, and breast cancers are also associated with endometriosis.
More specifically, a past systematic review and meta-analysis found that women with endometriosis have almost 2 times the risk of ovarian cancer (summary relative risk [SRR], 1.93; 95% CI, 1.68-2.22; n = 24 studies).3 There is also strong evidence of an association between endometriosis and clear cell (SRR, 3.44; 95% CI, 2.82-4.20; n = 5 studies), low-grade serous (SRR, 2.33; 95% CI, 1.64-3.31; n = 2 studies), and endometroid (SRR, 2.33; 95% CI, 1.82-2.98; n = 5 studies) ovarian cancer.
Conversely, few studies have explored the associations between ovarian cancer and endometriosis subtypes, like ovarian endometriomas, superficial peritoneal endometriosis, and deep infiltrating endometriosis.1 Therefore, the researchers evaluated the associations of both endometriosis and endometriosis subtypes with overall and histotype-specific ovarian cancer incidence.
Patients with endometriosis have a 4.2-fold greater risk of ovarian cancer, highlighting the need for further research into the biological links between endometriosis subtypes and ovarian cancer | Image Credit: Lars Neumann - stock.adobe.com
To do so, they used the Utah Population Database (UPDB), which links vital records, health facility records, Utah Cancer Registry records, and the University of Utah and Intermountain Health electronic health records (EHRs) of more than 11 million patients.4 They created a retrospective endometriosis cohort, using UPDB data from 1992 to 2019, identifying all women aged 18 to 55 years with 1 or more endometriosis diagnoses.1
Of the identified patients, 72.1% had 1 endometriosis diagnostic record, 14.3% had 2, and 13.6% had 3. The researchers subtyped these diagnoses into 5 categories using the International Classification of Diseases, Ninth Edition (ICD-9) and Tenth Edition (ICD-10) codes. The categories included superficial peritoneal endometriosis (n = 39,3277; 49.8%), ovarian endometriomas (n = 18,977; 24.1%), ovarian endometriomas and concurrent deep infiltrating endometriosis (n = 1374; 1.7%), deep infiltrating endometriosis (n = 1028; 1.3%), and other (n = 18,237; 23.1%).
To improve efficiency, the researchers used a matched cohort design. "Exposed” women with endometriosis diagnoses (n = 78,893) were matched in a 1:5 ratio to “unexposed” women without known endometriosis (n = 379,043) by birthplace (Utah or other) and birth year; all unexposed women lived in Utah as of their matched endometriosis case’s diagnosis date.
The researchers also identified ovarian cancer diagnoses between 1992 and 2019 (n = 597) using the Utah Cancer Registry. They then used Surveillance, Epidemiology, and End Results Program morphology codes to assign cases to histotypes, namely low-grade serous, high-grade serous, mucinous, endometrioid, clear cell, and other. Because of the small case counts for less common histotypes, the researchers grouped cases into type 1 (clear cell, endometrioid, mucinous, and low-grade serous) and type 2 (high-grade serous) ovarian cancer for their analyses.
From their initial cohort, the researchers excluded those who died (n = 11), had prevalent cancers (n = 2458), underwent a bilateral oophorectomy where they surgically removed both ovaries (n = 4482), or had ovarian cancer before their index date or that of their matched endometriosis case’s (n = 79). The final study population included 450,906 women, of whom, 78,476 had endometriosis and 372,430 did not.
Their main analyses assessed superficial peritoneal endometriosis, deep infiltrating endometriosis and/or endometriomas, and other endometriosis; however, the researchers also conducted analyses assessing all subtypes separately. Also, exposed women were followed up from their endometriosis index date, while unexposed women were followed up from the endometriosis index date of whom they were matched. More specifically, each patient was followed up until ovarian cancer diagnosis, death, bilateral oophorectomy, or December 31, 2019, whichever came first.
The women included in the study population had a mean (SD] age of 36 (10) years at first endometriosis diagnosis and had a mean follow-up of 12 (7) years. Most (75%) had given birth, and 6% underwent a bilateral oophorectomy during follow-up. Compared with those without endometriosis, patients with endometriosis were more likely to have never given birth (31% vs 24%) and to have undergone a hysterectomy during follow-up (39% vs 6%).
Additionally, the researchers determined that patients with endometriosis had a higher risk of all ovarian cancer histotypes (adjusted HR [aHR], 4.20; 95% CI, 3.59-4.91). More specifically, ovarian cancer risk was highest for those with deep infiltrating endometriosis and/or ovarian endometriomas (aHR, 9.66; 95% CI, 7.77-12.00).
Lastly, they found that patients with deep infiltrating endometriosis and/or ovarian endometriomas had the highest risk of both type 1 (aHR, 18.96; 95% CI, 13.78-26.08) and type 2 (aHR, 3.72; 95% CI, 2.31-5.98) ovarian cancer.
The researchers acknowledged their limitations, one being the possible misclassification of endometriosis. This was because of the absence of a biomarker for diagnosing endometriosis, along with the challenges of diagnosing endometriosis in women without symptoms or access to care. Despite their limitations, the researchers suggested areas for further research.
“Studies that can better characterize the biology underlying these associations are urgently needed to guide improved ovarian cancer screening and prevention strategies among women with severe endometriosis, with or without other important ovarian cancer risk factors (eg, BRCA1/2 variations) and to inform novel molecular targets for ovarian cancer treatments,” the authors concluded.
References
1. Barnard ME, Farland LV, Yan B, et al. Endometriosis typology and ovarian cancer risk. JAMA. Published online July 17, 2024. doi:10.1001/jama.2024.9210
2. Buck Louis GM, Hediger ML, Peterson CM, et al. Incidence of endometriosis by study population and diagnostic method: the ENDO study. Fertil Steril. 2011;96(2):360-365. doi:10.1016/j.fertnstert.2011.05.087
3. Kvaskoff M, Mahamat-Saleh Y, Farland LV, et al. Endometriosis and cancer: a systematic review and meta-analysis. Hum Reprod Update. 2021;27(2):393-420. doi:10.1093/humupd/dmaa045
4. Prahalad S, Zeft AS, Pimentel R, et al. Quantification of the familial contribution to juvenile idiopathic arthritis. Arthritis Rheum. 2010;62(8):2525-2529. doi:10.1002/art.27516
