- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
New Model Predicts Stroke Severity and Improves Functional Independence
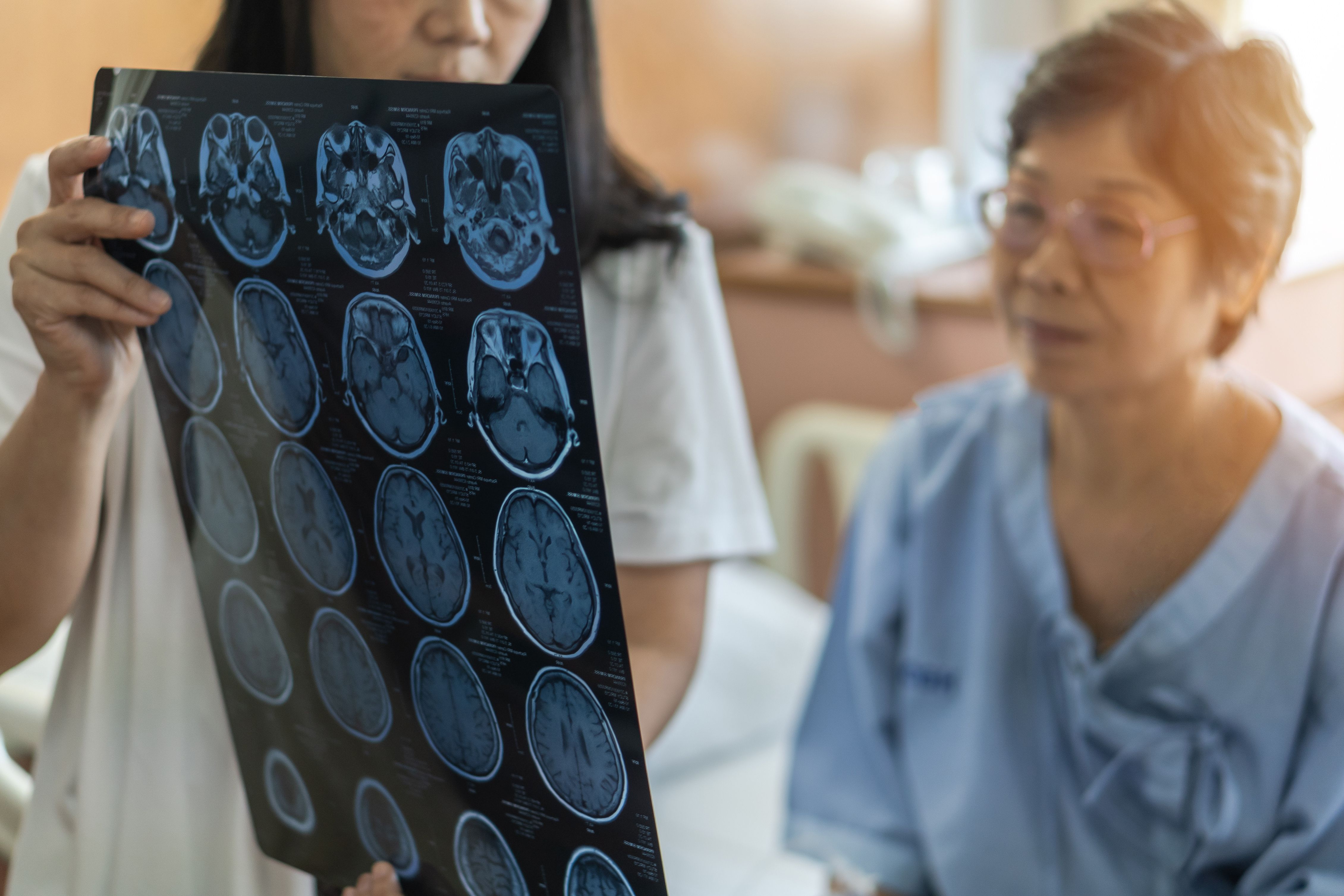
A new predictive model developed by Ochsner Health helps clinicians make real-time decisions for patients who had a stroke undergoing urgent carotid intervention, improving chances of regaining functional independence.
A new predictive model developed by Ochsner Health helps clinicians make real-time decisions for patients who had a stroke undergoing urgent carotid intervention, improving chances of regaining functional independence. | Image Credit: Chinnapong - stock.adobe.com
Functional independence following acute stroke can be predicted with high accuracy using a novel, data-driven model that incorporates factors like stroke severity and frailty, according to a study published in the Journal of the American College of Surgeons.1
Developed by Ochsner Health, the model uses a data-driven approach, offering real-time decision support. The tool combines 4 critical clinical metrics: stroke severity, frailty risk score, time to intervention, and thrombolysis use.
Stroke ranks second in worldwide mortality rates and fifth in US mortality. Stroke risk increases with age but can occur at any age.2 Stroke is the leading cause of serious long-term disability and can reduce mobility in over half of patients over 65.
Carotid artery disease causes up to 20% of ischemic strokes.1 Blood clots or other particles block brain blood vessels, and plaque buildup can also cause blockages.3
Early action is crucial to reduce stroke risk and prevent neurological decline.1 The ability to recognize signs and symptoms of stroke allows patients to react quickly, increasing their overall chances of survival.2 Signs of stroke onset include sudden numbness (especially on 1 side), confusion, speech problems, and vision impairment.4
Carotid endarterectomy (CEA) and carotid artery stenting (CAS) are popular interventions for acute carotid-related stroke.1 CEA surgically removes plaque from narrowed carotid arteries.5 CAS uses a catheter and stent to open clogged arteries and restore brain blood flow.
A retrospective cohort study analyzed data from 302 patients with prior strokes who underwent CEA and CAS at a Comprehensive Stroke Center (2015-2023).1 The primary outcome was functional independence (Modified Rankin Scale [mRS] score ≤ 2), and the secondary outcome was a composite of 30-day stroke, death, and myocardial infarction (MI).
The average time to intervention was 3 days overall (CEA, 3.8 days; CAS, 1.3). More than half of the patients (72.8%) were deemed functionally independent upon discharge. The cohort's mean age was 65.8 years, 37.4% were female, and 73.2% were White.
Cardiovascular comorbidities included hypertension (89.1%), hyperlipidemia (76.5%), tobacco use (67.5%), diabetes (34.1%), and coronary artery disease (26.5%). There were 26.2% of patients had a history of prior stroke before presenting with an index carotid-related cerebral ischemic event. Patients who were discharged as functionally dependent were often older and had experienced a higher number of stroke incidences (P = .071 and P = .190, respectively).
Procedural Characteristics and Clinical Outcomes
During the study period, 70.9% of patients underwent CEA and 29.1% underwent CAS. Also, 76.6% of the CEA group and 63.6% of the CAS group were deemed functionally independent at discharge. Patients who underwent CAS with thrombolysis (CAS + thrombolysis or CAS + thrombolysis + thrombectomy) had the lowest rates of functional independence at discharge (CAS + thrombolysis, 38.5%; CAS + thrombolysis + thrombectomy, 57.1%). Rates of being deemed functionally independent at discharge increased among patients who underwent CAS alone (70%) or CAS with thrombectomy (71.4%).
The 30-day adverse event rate (stroke, MI, or death) was 8.3% overall: 6.5% after CEA and 12.5% after CAS. This difference may have been due to a higher proportion of severe stroke cases in the CAS group.
Frailty Risk and Stroke Severity
Patients who were deemed functionally independent had lower frailty risk (median score, 24.7; IQR, 14.3-35.3) than patients considered functionally dependent (median 37.2; IQR, 24.4-48.7). Frailty risk was categorized as low (7.9%), intermediate (50.3%), and high (41.7%).
Time to Intervention and Length of Stay
The average time to intervention was 3 days (IQR, 1-4 days) in both cohorts, with 49.7% of the group receiving treatment within 48 hours (P = .173). Patients deemed functionally dependent had longer hospital stays (median, 10 days) than patients considered independent (median, 6 days).
Model Performance
The model correctly classified 93% of patients who are functionally independent, demonstrating strong predictive performance. The 30-day adverse event rate was higher in patients classified as functionally dependent (8.3% overall).
Limitations
The study design limits generalizability, and future research should validate the model across multiple centers. Further investigation of key clinical variables is also warranted.
Integrating frailty assessments into the electronic medical record system highlights the model's practicality and potential for widespread adoption. The model personalizes treatment to improve acute stroke care outcomes by informing clinical decisions.
“Predicting a patient’s recovery potential with such reliability gives us an unprecedented level of confidence in our treatment decisions,” said Leo Seoane, MD, executive vice president and chief academic officer at Ochsner Health and founding dean for the Xavier Ochsner College of Medicine.6
References
- Bazan HA, Fort D, Snyder L, et al. Precision in stroke care: anovel model for predicting functional independence in urgent carotid intervention patients. J Am Coll Surg. Published online January 17, 2025. doi:10.1097/xcs.0000000000001276
- Stroke facts. Stroke. CDC. April 25, 2024. Accessed January 30, 2025. https://www.cdc.gov/stroke/data-research/facts-stats/index.html
- About stroke. CDC. April 25, 2024. Accessed January 30, 2025. https://www.cdc.gov/stroke/about/index.html
- Signs and symptoms of stroke. CDC. October 24, 2024. Accessed January 30, 2025. https://www.cdc.gov/stroke/signs-symptoms/index.html
- Vasavada AM, Singh P, Firdaus A, et al. Carotid endarterectomy versus stenting for the treatment of patients with carotid artery stenosis: an updated systematic review and meta-analysis. Cureus. 2023;15(2):e35070. doi:10.7759/cureus.35070
- New tool predicts stroke outcome with 93% accuracy, guiding better carotid surgery decisions. Newswise. January 28, 2025. Accessed January 30, 2025. https://www.newswise.com/articles/new-tool-predicts-stroke-outcome-with-93-accuracy-guiding-better-carotid-surgery-decisions/?sc=dwhr&xy=10046402
Dr Joseph Biggio Discusses Ochsner Health's Connected MOM Program, COVID-19 Pregnancy Challenges
September 15th 2020At Ochsner Health, the largest nonprofit academic health care system in Louisiana, providers are leveraging the system’s Connected Maternity Online Monitoring (MOM) digital medicine program to minimize expectant mothers’ risks of contracting COVID-19.
Listen
Advancing Early Detection and Equitable Access in Alzheimer Disease Care
December 11th 2025Experts at a roundtable in Boston, Massachusetts, on November 3, 2025, discussed improving early Alzheimer disease diagnosis, addressing workforce and equity gaps, and expanding access to new disease-modifying therapies.
Read More
Transforming Alzheimer Disease Research Into Real-World Care: Q&A With B. Joy Snider, MD, PhD
December 10th 2025In 2025, each issue of Population Health, Equity & Outcomes has featured a profile of a health system leader transforming care in their area of expertise. This issue spotlights a conversation with B. Joy Snider, MD, PhD, professor of neurology at Washington University in St Louis.
Read More
