- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Most Patients With Medicare Need Additional Financial Assistance to Get Novel Oral Therapies
Karmanos Cancer Institute, in Detroit, Michigan, established a specialty pharmacy to help alleviate the financial burden many patients face when paying for their oral novel therapeutics.
It’s no surprise that oral novel therapeutics (ONTs) used to treat hematologic malignancies are expensive. What is surprising is that most Medicare patients require additional financial assistance to help pay for these therapies each month, according to data presented on December 7, 2019, during at the 61st American Society of Hematology Annual Meeting and Exposition in Orlando, Florida.
Karmanos Cancer Institute, in Detroit, Michigan, established a specialty pharmacy to help alleviate the financial burden many patients face when paying for their ONTs. The pharmacy helps streamline the often frustrating and complex process of obtaining prior authorization (PA) and determining patient payment obligation. Federal regulations prohibit Medicare beneficiaries from using co-pay cards to decrease their out-of-pocket costs because CMS believes that doing so will drive up overall costs for insurers. Karmanos then goes one step further on behalf of patients, automatically applying for financial assistance when necessary, in the form of co-pay cards and foundation grant funding, before determining what a patient will ultimately have to pay and when their drugs will be delivered.
Hoping to establish patterns of cost and the need for financial assistance since the specialty pharmacy was established, first author Erlene K. Seymour, MD, and her team used a retrospective review of data from March 2018 through May 2019. During this time, the prescription claims totaled over $2 million. Data were gathered on the following: drug prescribed, type of insurance (Medicare, Medicaid, private), insurer cost, final patient cost-sharing, costs covered by foundation grant assistance or co-pay cards (if needed), and number of days between written prescription and (1) PA and (2) drug delivery to patient (see Table).
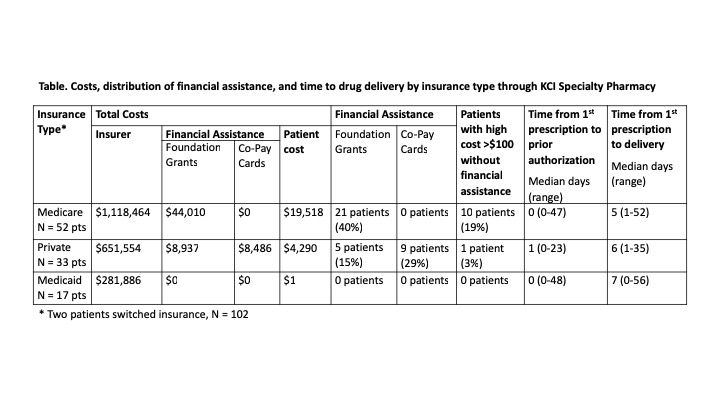
Overall, 35% of the patients needed help with payment, most of which was done through foundation grants versus co-pay cards (26% vs 9%). Medicare accounted for half of all reimbursement; 40% of these patients needed foundation grant assistance, and 19% ended up with high co-pays of $100 or more. Fifty-two percent of patients had Medicare; 33%, private coverage; and 17%, Medicaid. From most to least costs covered, Medicare topped the list by paying half, followed by foundation grant assistance, the patients themselves, and co-pay cards. Also, neither insurance type nor grant need factored into time needed for PA or drug delivery: 1 and 7 days, respectively.
“Of the $2 million in total drug costs, 4% was total patient co-payments, which presented as high co-pays for many patients. Thirty-six percent of these patients received financial assistance, mostly through foundation grants,” Seymour said in an email to The American Journal of Managed Care.® “Karmanos Specialty Pharmacy implemented an efficient process of applying for financial assistance, which decreased total patient cost by 79%. However, the fact that so many required assistance or continued to pay high co-pays emphasizes the need to cap these costs for our patients.”
Reference
Seymour EK, Daniel L, Pointer E, Smith ST, Schiffer CA. High dependence on Medicare and foundation grant assistance among patients with hematologic malignancies receiving novel oral therapeutics. Presented at: 61st American Society of Hematology Annual Meeting & Exposition; December 7-10, 2019; Orlando, Florida. Abstract 64. ash.confex.com/ash/2019/webprogram/Paper128905.html.
