- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Mitochondrial Dysfunction Linked to MS, Further Studies Needed on Metabolic Impact
More research is necessary to understand cerebral oxygen consumption as a predictive biomarker for brain atrophy in multiple sclerosis (MS); however, this study found that mitochondrial dysfunction could have a role in the underlying pathophysiology of MS.
Mitochondrial dysfunction has been indicated as a possible mechanism in the pathophysiology of relapsing/remitting multiple sclerosis (RRMS); however, more studies are needed to determine the value of cerebral oxygen consumption as a predictive biomarker, according to a recent study published in Journal of Cerebral Blood Flow & Metabolism.
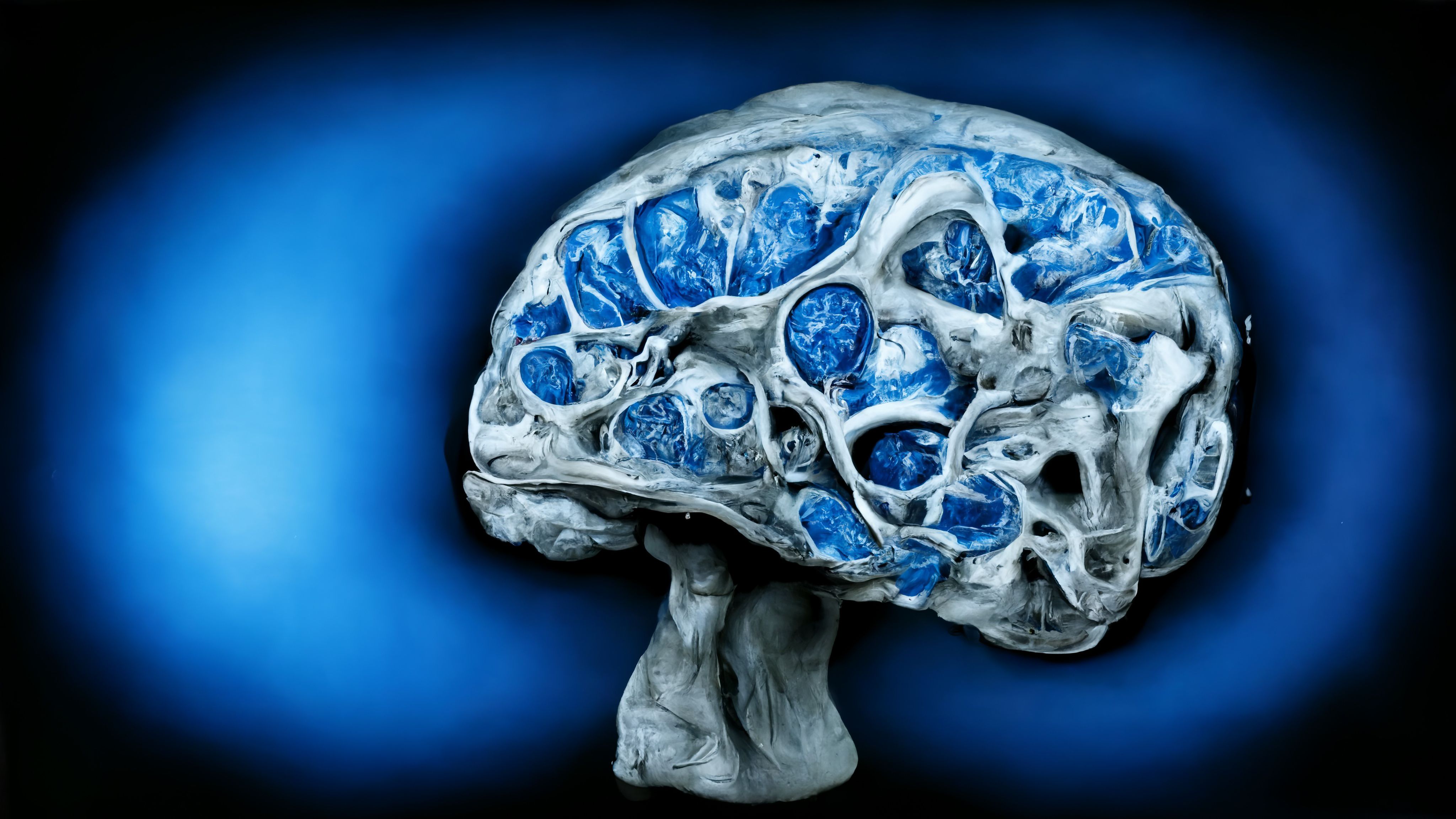
Brain Atrophy and Degeneration Concept | image credit: catalin - stock.adobe.com
Although recent progress has made multiple disease-modifying treatments (DMTs) available to patients with MS, patients are still susceptible to disease progression and cerebral atrophy—even when treatments are deemed successful. This reality leads researchers, such as the present authors, to ponder avenues for advancing the current understandings of MS pathophysiology.
The authors of the present study detail that the cerebral metabolic rate of oxygen consumption (CMRO2) is reduced in patients with MS compared with otherwise healthy individuals. Due to the observed alterations in oxygen and glucose metabolism, one theory suggests that the brains of patients with MS may be fatigued and affected by energy failures.
The mechanistic pathophysiology of this phenomenon is not completely understood. Questions remain regarding the extent to which the reduction in metabolic demand stems from brain atrophy or whether the dysfunctional metabolism is a driver of neurological damage. To confront these questions, researchers conducted a study to investigate brain atrophy and CMRO2 in a cohort of patients with RRMS. Their aim was to evaluate whether those with RRMS experienced worsening CMRO2 impairment and how much this progression could be attributed to measures of brain atrophy and Expanded Disability Status Scale (EDSS).
Forty-two patients with RRMS enrolled from the Multiple Sclerosis Clinic, Rigshospitalet, Copenhagen, Denmark, and compared with 35 healthy controls enrolled after following an online advertisement were included (aged 18-52 years). Phase-contrast mapping (PCM MRI was used to measure participants’ cerebral blood flow (CBF).
Healthy control individuals exhibited, on average, significantly higher CMRO2 compared with patients with RRMS (143.2 vs 121.2 mmol/100 g/min; P = .003). In the control group, there was a significant increase observed in CMRO2 as age increased (mean effect: þ0.7 mmol/100 g/min per year, 95% CI, 0.02-1.32; P = .04); on the other side, patients endured diminishing CMRO2 with age increase (mean effect: 0.68 mmol/100 g/min per year, 95% CI, 1.81-0.45; P = .2).
The authors did not find any significant associations in CBF between the cohorts, nor did age factor into significantly differing CBF between groups. Patients with MS additionally experienced a reduction of cerebral oxygen extraction with advancing age compared with healthy controls. Results demonstrated that the patient group had a significantly increased amount of oxygen saturation in the blood leaving the brain in the sagittal sinus compared with controls (69.58% vs 65.70%; P = .02).
Measurements of brain volume showed that the average brain parenchymal fraction (BPF) reduced with age (P < .01) and occurred at a similar rate per year between both cohorts: controls, 0.1% and patients, 0.08% (P = .034). Overall, measurements of BPF and grey matter were not significantly different and white matter fractions were also similar. Grey matter was noted to decrease with age in each group, whereas white matter was not, indicating that the associations between age and brain atrophy were comparable between the cohorts.
Although insignificant, concentrations of the neural energy metabolism marker N-acetyl aspartate (NAA) were noted to have an opposing relationship in controls compared with patients. For controls, CMRO2 trended upward with a concentration of NAA whereas patients exhibited a downward trend despite there being no age-related differences in NAA concentration.
CMRO2 was also not significantly correlated with patients’ EDSS scores.
Reflecting on their findings, the researchers recognize then need for further studies to examine the relationship between reductions in cerebral oxygen consumption and brain atrophy. However, their results do indicate mitochondrial dysfunction in the underlying pathophysiology of RRMS.
Reference
Knudsen MH, Vestergaard MB, Lindberg U, et al. Age-related decline in cerebral oxygen consumption in multiple sclerosis. J Cereb Blood Flow Metab. 2024:271678X231224502. doi:10.1177/0271678X231224502
